Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Case Report
Blunt abdominal trauma resulting in pancreatic injury in a pediatric patient in Australia: a case report -
Harmanjit Dev, MBBS
 , Colin Kikiros, MBBS
, Colin Kikiros, MBBS
-
Journal of Trauma and Injury 2023;36(3):310-314.
DOI: https://doi.org/10.20408/jti.2023.0013
Published online: August 24, 2023
- 656 Views
- 40 Download
Department of Paediatric Surgery, Perth Children’s Hospital, Nedlands, WA, Australia
- Correspondence to Harmanjit Dev, MBBS, Department of Paediatric Surgery, Perth Children’s Hospital, 15 Hospital Ave, Nedlands, WA 6009, Australia Tel: +61-08-6456-4269, Email: harman_dev@hotmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Pancreatic trauma from a blunt injury is fairly uncommon in the pediatric population. Furthermore, such trauma with associated disruption of the pancreatic duct (PD) is even less prevalent and is associated with high morbidity and mortality. Pancreatic injuries in the pediatric population are often missed and hence require a thorough workup in children presenting with any form of abdominal injury. This case report describes a young boy who presented with abdominal pain and did not initially inform medical staff about any injury. For this reason, his initial provisional diagnosis was appendicitis, but he was later found to have transection of the pancreas with injury to the PD on imaging. The management of such injuries in pediatric patients often poses a challenge due to a lack of pediatric physicians trained to perform interventions such as endoscopic retrograde cholangiopancreatography. Furthermore, such interventions carry a higher risk when performed on children due to the smaller size of their pancreatic ducts. As a result, our patient had to be transferred to an adult center to undergo this procedure. Thus, maintaining a high degree of suspicion, along with a detailed history and examination, is crucial for the early diagnosis and management of pancreatic injuries.
- Visceral injuries in children account for only about 10% of all trauma cases, with the majority involving head and extremity injuries [1]. Pancreatic injuries, which are relatively rare and potentially life-threatening in children, make up 0.6% of all abdominal trauma cases in this population, and pancreatic duct (PD) injuries are even less common. A study by Canty and Weinman [2] reported that among 14,245 pediatric trauma patients admitted to a US-based hospital, a mere 0.12% had PD injuries. Studies also indicate that over 75% of pancreatic injuries in children result from blunt trauma, most commonly caused by handlebar injuries or seatbelts. It is crucial to recognize that diagnosing blunt pancreatic injuries can be challenging and requires a high degree of suspicion for proper management [3]. Furthermore, pancreatic injuries can range from minor contusions to severe damage involving the PD [4].
- Our report concerns a patient who initially presented with a history and clinical symptoms suggestive of appendicitis. However, upon further examination and investigation, the true cause of his abdominal pain was revealed.
INTRODUCTION
- We present the case of a 10-year-old boy with no significant past medical or surgical history, who was transferred from a peripheral hospital to our pediatric emergency department. He was referred to our general surgical department for possible appendicitis in the late evening. During his initial surgical assessment, the impression was indeed that of appendicitis due to a 2-day history of gradually worsening abdominal pain accompanied by vomiting. Furthermore, upon admission, his inflammatory markers were elevated, with a C-reactive protein (CRP) of 75 mg/L and a white cell count (WCC) of 15×109/L. He was scheduled for a fasting review and abdominal ultrasound (USS) the following morning. The next day, the boy was evaluated by the day surgical team, and a complete history and examination were conducted once again. The child and his mother reported that he had returned home with severe abdominal pain after playing with his friends and had been asymptomatic prior to this incident.
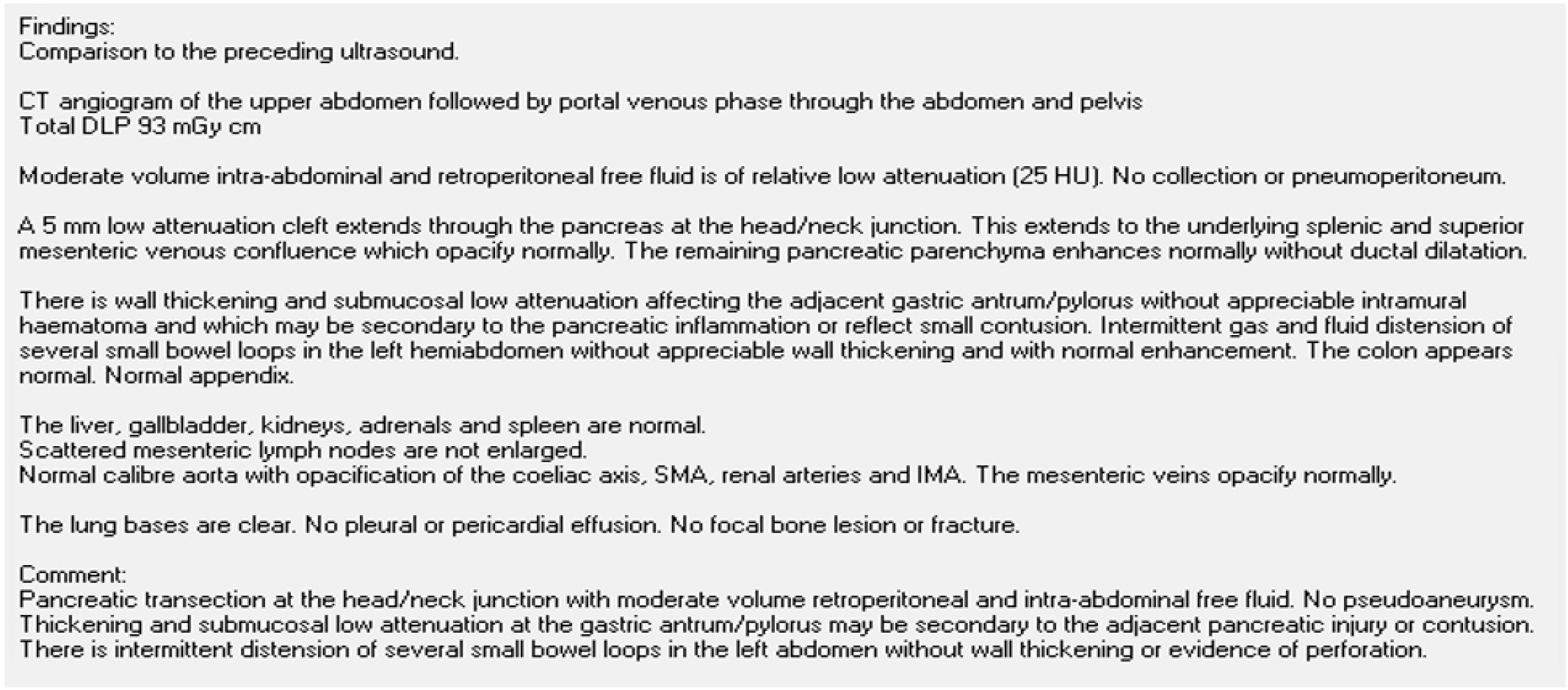
- In summary, the child experienced a gradual onset of abdominal discomfort while playing outside with his friends. Subsequently, he suffered from nausea and two instances of nonbilious vomiting. He did not exhibit any other signs of infection, such as fever or diarrhea. Based on this history, we were not convinced that the child had appendicitis, as he lacked significant infectious symptoms; his vomiting could have been a result of pain. Upon conducting further blood tests, his CRP level rose to 106 mg/L, while his WCC dropped to 11×109/L (Fig. 1).
- We subsequently inquired if the child had experienced any incidents while playing outside, such as an injury. He then remembered that he had been riding his quadbike and collided with a tree. Upon further questioning, he disclosed that the steering wheel had indeed struck his upper abdomen during the impact. He experienced mild abdominal pain at the time but continued to play on the trampoline. Since he appeared relatively pain-free after the quadbike incident and proceeded to jump on the trampoline, his parents did not initially attribute the pain to the accident. The child informed us that it was only after jumping on the trampoline that the pain rapidly intensified.
- His observations remained stable, with no signs of fever. Upon examination, he appeared uncomfortable and exhibited a mildly distended abdomen without any visible bruising. He experienced generalized tenderness, tested positive for Rovsing sign, and displayed guarding with peritonism. Based on this comprehensive history and examination findings, our impression was that he had either sustained a blunt visceral injury or was suffering from perforated appendicitis. As planned, he underwent abdominal USS, which revealed "moderate volume free fluid with echogenic dependent debris concerning for blood products." There was no evidence of pneumoperitoneum, but an abdominal visceral injury could not be ruled out. Consequently, a nasogastric tube (NGT) was inserted, and he was started on broad-spectrum intravenous antibiotics. We also added a lipase test to his initial blood work following the USS review, which showed an elevated level of 3,680 U/L (normal level is <45 U/L).
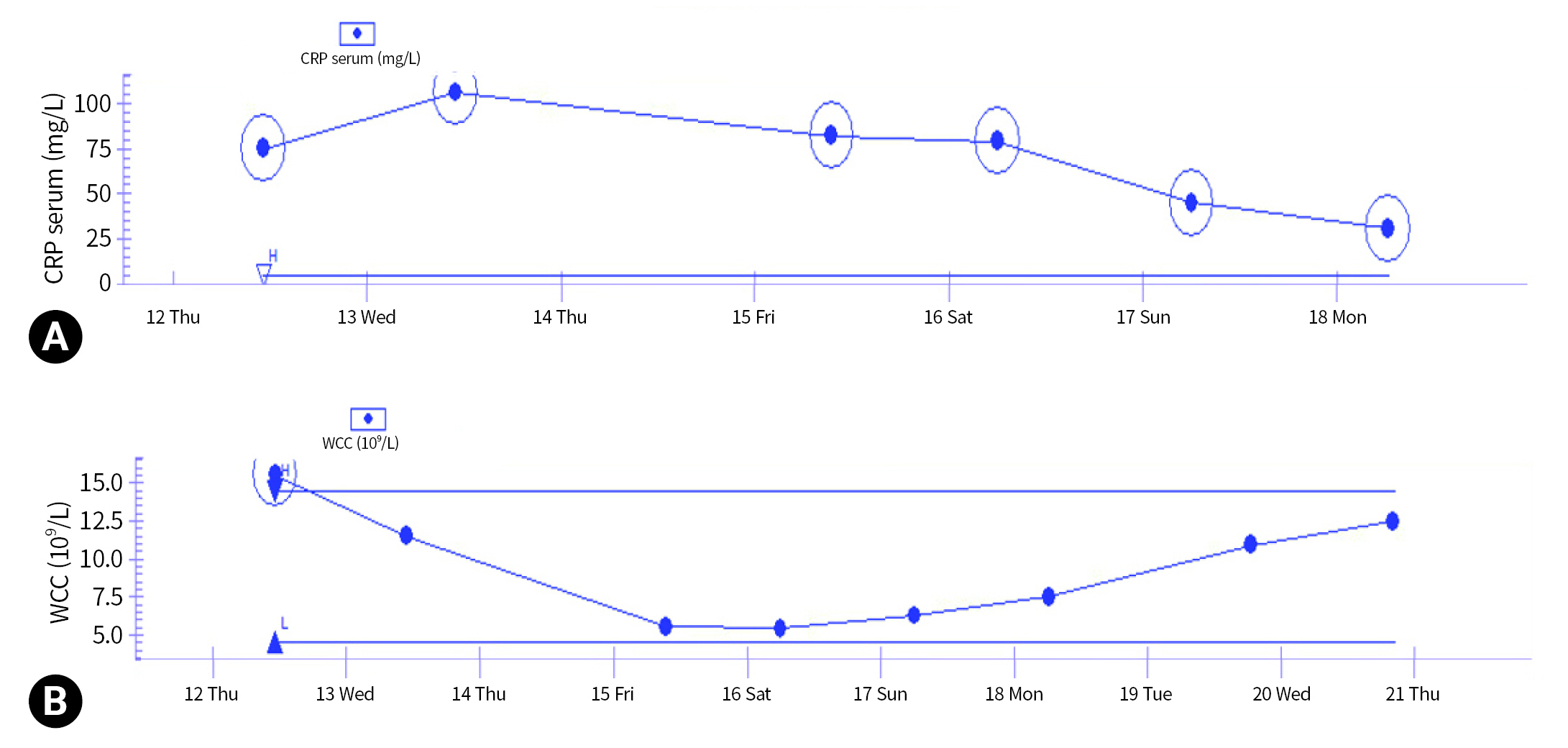
- Upon reviewing the USS report, an urgent computed tomography (CT) scan of the patient's abdomen and pelvis was requested for a more detailed evaluation. The CT scan revealed a pancreatic transection accompanied by a moderate volume of retroperitoneal and intra-abdominal free fluid (Fig. 2). Additional findings included thickening in the gastric pylorus region, likely due to the adjacent pancreatic injury, and a normal appendix (Fig. 3). Consequently, the child's abdominal discomfort was indeed caused by pancreatic injury resulting from the previously mentioned blunt abdominal trauma sustained during the quadbike accident. Moreover, since the transection was located near the pancreatic head/neck junction, we had a high suspicion of PD injury.
- For further specialist management, we contacted the gastroenterology team at an adult hospital located on the same campus as our hospital. This was because our pediatric gastroenterology team does not perform endoscopic retrograde cholangiopancreatography (ERCP). The child was transferred to the adult center on the same day for the procedure. During ERCP, the patient was found to have acute pancreatitis and a high-grade leak from the main PD injury at the level of the neck. There was also resistance at the site of the leak when attempting to cannulate the duct with a 5F catheter. A 3.5F catheter (the smallest available at the time) was then used to achieve deeper cannulation; however, the same resistance was noted. Eventually, a 5F single pigtail PD stent was inserted with the stent positioned just at the site of injury. It was unable to traverse to the distal body. The patient was then transferred back to our care for further post-ERCP treatment.
- He remained under our care for a total of 11 days, during which he made significant progress following the ERCP. We closely monitored his blood glucose levels, liver function, electrolytes, and inflammatory markers. The acute pain team was involved in optimizing his analgesia. To support his nutritional status, he received total parenteral nutrition (TPN) for approximately 5 days. Prior to discharge, we gradually weaned him off TPN and slowly upgraded his diet from clear fluids to a full oral diet, as tolerated. We also removed his NGT. As a result, his abdomen became softer, less distended, and his pain continued to decrease. Upon discharge, his blood tests showed improvement, he was tolerating a full oral diet, and he experienced no abdominal pain. Furthermore, a repeat USS performed prior to discharge revealed no peripancreatic collection and a reduction in free fluid.
- The patient subsequently underwent scheduled outpatient magnetic resonance cholangiopancreatography at 2 weeks, which revealed no pseudocyst and an interval resolution of peripancreatic free fluid. Disruption of the pancreatic neck parenchyma was observed again, but without any concerns of PD dilatation. He then proceeded to have his stent removed as a day procedure 6 weeks after the initial ERCP. Following this, a follow-up USS examination demonstrated mild thinning of the pancreatic neck, but no collection or duct dilatation. Overall, the patient has remained in good health since discharge, with appropriate weight gain.
- Ethics statement
- Informed consent was obtained from the patient’s parents. The anonymity of the patient was also maintained.
CASE REPORT
- As previously stated, blunt pancreatic injuries in the pediatric population are uncommon and present both diagnostic and therapeutic challenges. Furthermore, pancreatic injuries can lead to high morbidity and mortality [4]. Consequently, it is crucial to consider this possibility when evaluating a child with a history of abdominal trauma, even in the absence of visible external signs. Additionally, there are various grades of pancreatic injury based on the extent of parenchymal and/or ductal damage [5]. The degree of the injury determines both the patient's condition and the most suitable management approach. Minor contusions are typically managed conservatively, while major injuries may necessitate interventions such as an ERCP.
- When a child is suspected of having abdominal trauma, it is crucial to conduct further investigations using both blood tests and imaging to ensure that a visceral injury is not overlooked. Serum amylase and lipase levels have been identified as sensitive indicators of pancreatic cell damage and can therefore be utilized in the initial workup when pancreatic injury is suspected. Specifically, lipase and/or amylase levels in the admission blood samples are a reliable sign of acute pancreatic injury, and this simple test should be performed on all patients presenting with undifferentiated and atypical abdominal pain.
- In addition, various imaging modalities can be employed in such cases. Abdominal USS is typically the first modality utilized. Depending on the findings of the USS, further evaluation can be conducted using CT and/or magnetic resonance imaging [3]. Early detection through an initial CT scan, combined with other imaging modalities and follow-up scans, may enhance the prognosis [6]. Studies have reported that interventional management was beneficial in patients with high-grade pancreatic injuries, as it resulted in shorter lengths of stay and fewer complications such as pseudocyst and fistula formation [4,7].
- Furthermore, reports indicate that ERCP is the most sensitive method for diagnosing PD injuries, although there is a risk of post-ERCP pancreatitis [8]. This modality can be used in select patients not only for diagnostic purposes but also for therapeutic intervention, as demonstrated in our case. A retrospective single-institution study that evaluated pediatric patients with pancreatic trauma over a 10-year period identified only four patients with PD injuries due to blunt trauma [9]. These patients underwent ERCP and stent placement without any post-procedure complications. In cases of proximal PD injuries where stent placement is not possible or has failed, conservative management may be considered, with the eventual formation and subsequent drainage of a pseudocyst. Distal injuries, in contrast, may require treatment with distal pancreatectomy [2].
- The placement of a stent proximal to the site of injury, as done in our patient, has been reported to allow continuous leakage of pancreatic enzymes and/or formation of a pseudocyst. In contrast, a stent that fully bridges the site of PD injury can better promote healing by preventing further leakage [9,10]. However, inserting a stent across the site of PD injury can be challenging, especially if there is a delay in initiating treatment [9]. Nevertheless, in our case, the PD stent led to significant clinical improvement despite it being short.
- Although ERCP offers direct visualization of ductal injuries and serves as a definitive management method for certain patients, their use in pediatric patients is limited. This may be due to the challenges of cannulating a small ampulla and the risk of post-ERCP complications, such as pancreatitis [9]. Furthermore, the limited availability of physicians who can perform emergency ERCP in children presents another obstacle [6].
- Pancreatic trauma, especially with PD injury, is uncommon amongst pediatric patients and poses a significant diagnostic challenge. It is essential to conduct a comprehensive history to ascertain if any trauma occurred prior to a child presenting with abdominal pain, as this may lead to high morbidity and mortality. This is especially true for patients with atypical pain that does not align with a typical infectious presentation. Early blood tests and the utilization of imaging techniques can further assist in diagnosing traumatic pancreatic injuries, enabling appropriate and timely management.
DISCUSSION
-
Author contributions
Conceptualization: all authors; Methodology: all authors; Project administration: all authors; Visualization: HD; Writing–original draft: HD; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION

- 1. Notrica DM. Pediatric blunt abdominal trauma: current management. Curr Opin Crit Care 2015;21:531–7. PubMed
- 2. Canty TG Sr, Weinman D. Management of major pancreatic duct injuries in children. J Trauma 2001;50:1001–7. ArticlePubMed
- 3. Antonsen I, Berle V, Soreide K. Blunt pancreatic injury in children. Tidsskr Nor Laegeforen 2017;137(17).
- 4. Goldberg-Murow M, Steiner Z, Lakovsky Y, et al. Blunt high-grade pancreatic injury in children: a 20-year experience in two pediatric surgical centers. Isr Med Assoc J 2021;23:180–5. PubMed
- 5. Moore EE, Cogbill TH, Malangoni MA, et al. Organ injury scaling, II: pancreas, duodenum, small bowel, colon, and rectum. J Trauma 1990;30:1427–9. PubMed
- 6. Kumar A, Panda A, Gamanagatti S. Blunt pancreatic trauma: a persistent diagnostic conundrum. World J Radiol 2016;8:159–73. ArticlePubMedPMC
- 7. Naik-Mathuria BJ, Rosenfeld EH, Gosain A, et al. Proposed clinical pathway for nonoperative management of high-grade pediatric pancreatic injuries based on a multicenter analysis: a pediatric trauma society collaborative. J Trauma Acute Care Surg 2017;83:589–96. PubMed
- 8. Keil R, Drabek J, Lochmannova J, et al. What is the role of endoscopic retrograde cholangiopancreatography in assessing traumatic rupture of the pancreatic in children? Scand J Gastroenterol 2016;51:218–24. ArticlePubMed
- 9. Ishikawa M, Shimojima N, Koyama T, et al. Efficacy of early endoscopic intervention in pediatric pancreatic duct injury management. Pediatr Surg Int 2021;37:1711–8. ArticlePubMedPDF
- 10. Varadarajulu S, Noone TC, Tutuian R, Hawes RH, Cotton PB. Predictors of outcome in pancreatic duct disruption managed by endoscopic transpapillary stent placement. Gastrointest Endosc 2005;61:568–75. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Massive traumatic abdominal wall hernia in pediatric multitrauma in Australia: a case report
- Penetrating gallbladder injury in a pediatric patient: a case report
- Pancreaticoduodenectomy as an option for treating a hemodynamically unstable traumatic pancreatic head injury with a pelvic bone fracture in Korea: a case report
- Delayed open abdomen closure using a combination of acellular dermal matrix and skin graft in Korea: a case report
- Penetrating sacral injury with a metallic pipe: a case report and literature review
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite




