Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(2); 2023 > Article
-
Case Report
Delayed open abdomen closure using a combination of acellular dermal matrix and skin graft in Korea: a case report -
Yoonseob Kim1
 , Tae Ah Kim1
, Tae Ah Kim1 , Hyung Min Hahn2
, Hyung Min Hahn2 , Byung Hee Kang1
, Byung Hee Kang1
-
Journal of Trauma and Injury 2023;36(2):152-156.
DOI: https://doi.org/10.20408/jti.2022.0024
Published online: November 4, 2022
- 1,250 Views
- 38 Download
1Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
2Department of Plastic and Reconstructive Surgery, Ajou University School of Medicine, Suwon, Korea
- Correspondence to Byung Hee Kang, MD Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, 164 World cup-ro, Yeongtong-gu, Suwon 16499, Korea Tel: +82-31-219-7764 Email: kbhname@aumc.ac.kr
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Delayed closure of an open abdomen (OA) is a clinically challenging task despite its various modalities. It is substantially more difficult when the duration of OA treatment is prolonged due to a patient’s condition. We introduced the management of a patient who had a delayed OA treatment spanning approximately 3 months due to severe abdominal contamination. The 64-year-old male patient had an injured pelvis pressed by a road roller. After visiting a trauma center, the patient initially underwent damage control surgery and OA management; however, early primary abdominal closure failed due to severe peritonitis. After negative pressure wound therapy for several months, an acellular dermal matrix graft followed by a skin graft were successfully used as treatments. A combination of acellular dermal matrix graft, negative pressure wound therapy, and skin graft techniques is a considerable management sequence for patients subjected to delayed OA treatment.
- Open abdomen (OA) management is a life-saving strategy for patients with trauma who requires damage control surgery for a severe abdomen injury, such as compartment syndrome, uncontrolled abdominal contamination, and abdominal wall tissue loss [1]. Although OA is a helpful method in the early stages of treatment for patients with trauma, it may result in delayed morbidity from conditions such as incisional hernia, abdominal abscess, and enteroatmospheric fistula (EAF). Therefore, after the initial resuscitation stage, the abdominal wall should be closed at an early stage. The closure rates of OA are archived during the first 7 to 10 days of treatment; however, afterward, the timing of abdominal closure tends to extend to 20–40 days and make poor outcome [2,3].
- Primary fascia closure is the best method of OA closure; however, it cannot be performed under many conditions. If it cannot be performed at an early stage, then it is unlikely to be performed at a late stage. As alternatives, various definitive closure methods for a difficult abdomen include bilateral anterior rectus sheath flap, component separation method, abdominal closure method using a mesh, planned ventral hernia, thigh musculocutaneous flap, early planned ventral hernia, and posterior component separation method [4]; however, no conclusion has been reached regarding the most suitable method.
- In this case, we performed abdominal wall restoration using an acellular dermal matrix (ADM) and skin grafts in a patient under long-term OA treatment due to intestinal perforation accompanied by open pelvic fractures and wound infection.
INTRODUCTION
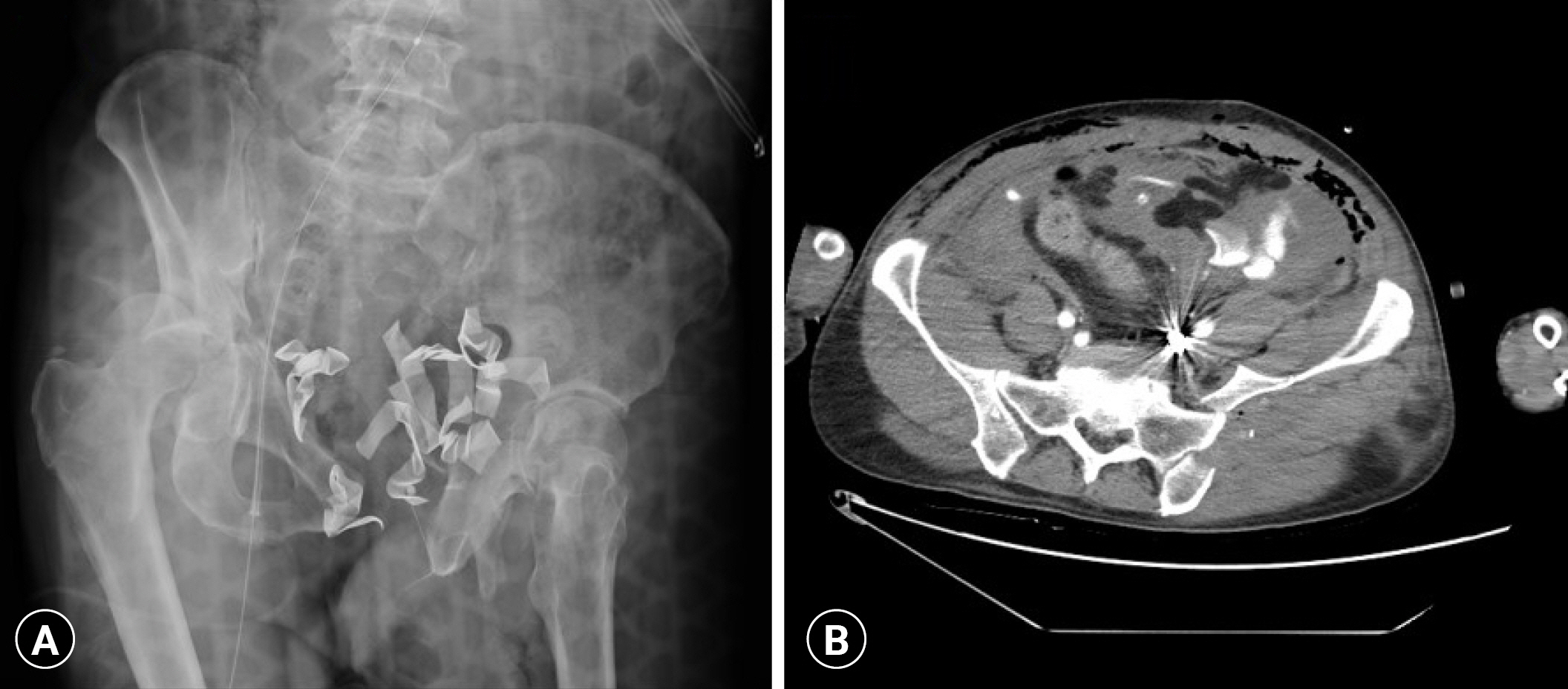
- A 64-year-old male patient, who had an injured pelvis that was pressed by a small road roller, visited a trauma center. The patient had a blood pressure of 64/32 mmHg, a heart rate of 63 beats/min, and was stupor with a Glasgow Coma Score of 13 (eye, 2; verbal, 5; motor, 6). On physical examination, active bleeding was observed in an open pelvic fracture from the left inguinal to the scrotal area. Massive transfusion, resuscitative endovascular balloon occlusion of the aorta, and pre-peritoneal pelvic packing were performed simultaneously. A radiograph taken at the trauma bay showed a severe pelvic bone fracture (Fig. 1A). The patient was immediately moved to the operating room for emergency surgery.
- The surgical findings showed ruptured pelvic floor muscles and a perforated rectum with multiple pelvic arterial injuries. Sigmoid colon hematoma was also identified. Hemostasis was attempted through ligation of bleeding vessels and perforated rectum was closed primarily. Following this, gauze packing was performed for the diffuse oozing. After wound irrigation with warm saline, the operation ended with an OA. Pelvic external fixation was performed by an orthopedic surgery team, followed by a damage control surgery.
- A day after the damage control surgery, the patient’s vital signs stabilized. Computed tomography scans were performed (Fig. 1B), followed by a second-look operation via a long midline abdominal incision; sigmoid colon segmental resection was performed due to sigmoid colon perforation with multiple mesenteric injuries. Sigmoid colon stump was made without anastomosis due to a severely contaminated abdomen and a high chance of leakage. Colon anastomosis or end colostomy was planned in the third operation, depending on the patient’s status. Likewise, the operation ended with an OA because of oozing from the abdominal cavity and severe intestinal swelling.
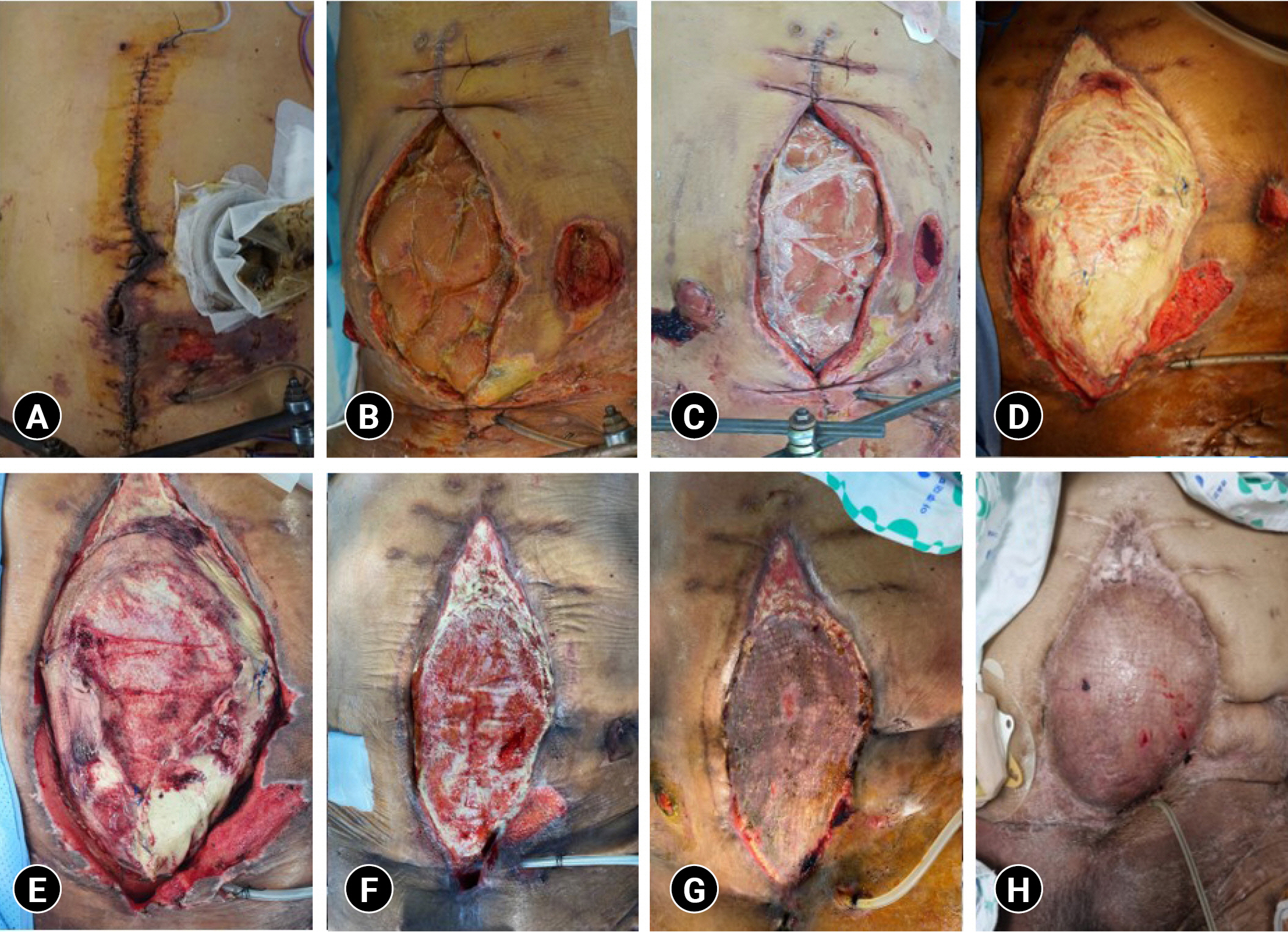
- The third operation was performed on the 3rd day of hospitalization; the OA was closed after the hemostasis of soft tissue bleeding in the pelvis and end-colostomy maturation in the left lower abdomen (Fig. 2A). However, on the 18th day of hospitalization, intestinal necrosis was observed on the colostomy site. The patient went into shock, and emergency surgery was performed. During the surgery, the EAF of the transverse colon and intestinal necrosis of the terminal ileum and cecum were observed, and a total colectomy was performed. Subsequently, an end ileostomy was formed in the right lower abdomen, and the surgery was terminated with an OA because of intraabdominal swelling (Fig. 2B). Abdominal closure was delayed for several weeks due to soft tissue necrosis, coagulopathy, and continued intraabdominal sepsis.
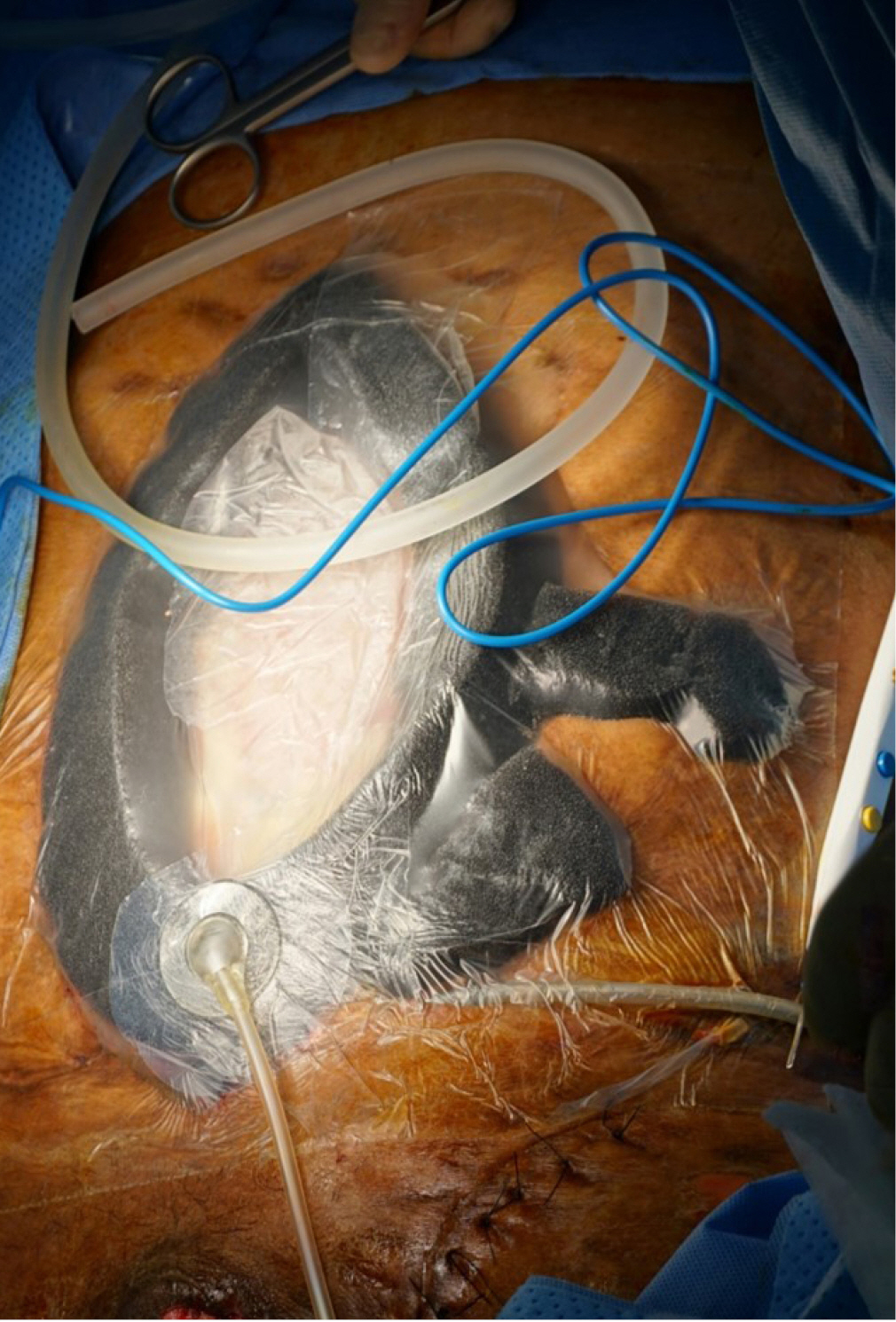
- The OA was managed through continuous negative pressure wound therapy (NPWT). To avoid direct pressure on the intestine, we used a sterile bag as the first layer of dressing directly in contact with the intestine and a soft silicon dressing (Mepitel, Mölnycke Health Care)) as the second layer of dressing (Fig. 2C). The pressure of the dressing was usually maintained at 120 mmHg (Fig. 3). Wound debridement and irrigation were repeated every 2 to 3 days in the operating room. Coagulation and abdominal inflammation considerably improved; however, primary fascia closure was not feasible due to massive and destructive tissue loss.
- After consulting with a plastic surgeon, we applied an ADM graft and planned a skin graft. As an intermediate step, wound covering with an ADM graft was attempted on the 48th day of hospitalization (Fig. 2D). Afterward, the ADM graft was partially lost; however, granulation tissue formation resulted in a membrane covering most of the surgical area (Fig. 2E, F). A split-thickness skin graft was used by the plastic surgery team 100 days after the second OA was created. The skin graft was well stabilized; it healed without an EAF or ulcer (Fig. 2G). Abdominal wall defects were not observed until the last follow-up (Fig. 2H) and patients were transferred to local hospital.
- Ethics statements
- Informed consent was obtained from the patient.
CASE REPORT
- In this case, we demonstrated that a chronically inflamed OA could be repaired through constant wound management. The management of patients with OA requires three fundamental steps: (1) hemodynamic resuscitation, (2) source control of abdominal infection, and (3) delayed abdominal closure [3]. Thus, a severe abdominal infection may extend the period of the second step, resulting in delayed abdominal closure. In this case, abdominal contamination had seriously progressed due to multiple necrosis of the small and large intestines and the occurrence of an EAF following rectal and colon damage.
- An OA can be definitively closed in various ways. According to a recent guideline, these are principally divided into nonmesh-mediated and mesh-mediated techniques. Nonmesh-mediated techniques include primary fascia closure, component separation method, and planned ventral hernia. Primary fascia closure is an ideal solution to restore abdominal closure; however, it is difficult to perform in an OA with fascial retraction [5]. The component separation method may be useful in managing an abdominal wound with fascial retraction; however, it should only be considered as a definitive closure technique; it destabilizes the outer layer of the abdominal wall, allowing the skin to shift in relation to the underlying myoaponeurotic tissue, making its application difficult in patients with enterostomies [6]. A planned ventral hernia is another treatment option to cover the abdominal viscera. It can be considered in cases of persistent contamination, several comorbidities, or severely ill patients [1]. Various skin coverage techniques that involve using skin grafts, or vascularized, pedicled, or free flaps, can be performed by comprehensively considering the condition of the wound, donor site, and patient [7]. In mesh-mediated techniques, a nonabsorbable synthetic mesh (i.e., polypropylene mesh) or biological prostheses can be used as wound closing materials. Synthetic meshes in contaminated fields are not recommended by the guidelines for emergency abdominal wall reconstruction [1,8].
- Despite several treatment strategies for OA treatment, using a synthetic mesh was contraindicated in our patient due to prolonged intraabdominal infection. Likewise, the component separation method could not be performed because the abdominal soft tissues, including the skin, subcutaneous fat, and fascia, became fibrotic tissue.
- Since its introduction in the mid-1990s, NPWT has continuously developed and become a popular treatment modality for managing acute and chronic wounds [2,9]. As a treatment modality, it provides the following clinical benefits: control of drainage of fluids, reduction of local edema, reduction of bacterial load, and early development of granulation tissue by angiogenic stimulation [10]. Therefore, we used NPWT as a wound management method for the reduction of tissue edema and stimulation of granulation tissue development.
- NPWT is an effective technique to reconstruct the abdominal wall; however, it poses a risk of developing complications, such as a fistula. In a systematic review, Boele et al. [11] reported primary fascia closure rates ranging from 35% to 92% and fistula rates ranging from 0% to 15%]. To avoid this complication, we used a sterile bowel bag as an impermeable barrier to protect and avoid direct pressure on the intestine; the sponge was in contact with the wound margin. Fascia retraction and intraabdominal adhesions may occur in a prolonged OA. If the fascia cannot be closed primarily, the defect may bridge with the ADM. At this time, NPWT can be instituted to help reduce edema, control wound exudates, and maintain the abdominal domain while encouraging abdominal fascial closure. It can be used in combination with a biological mesh to facilitate granulation and skin closure [12,13]. The skin graft can be used after the granulation tissue has grown on the ADM.
- There were three reasons for selecting ADM grafts. First, we intended to prevent the loss of additional nutrients and moisture by using it as a temporary coverage. ADM acts like a barrier because it has a dermis structure like that of human skin. Also, ADM with skin graft is expected to be better for hernia prevention than skin graft alone. Second, ADM promotes the wound healing process. Third, ADM could prevent adhesion by direct contact with internal organs, thereby lowering the chance of intestinal obstruction. However, ADM is quite expensive because it is not covered by the National Medical Insurance of Korea (it costs approximately 20,000 KRW/cm2).
- In conclusion, definitive abdominal closure can be performed through stepwise management. The combination of ADM and skin graft may be considered a reasonable treatment option, especially in patients with a prolonged OA.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Data sharing statement
Not applicable.
-
Author contributions
Conceptualization: YK, TAK, BHK; Data curation: YK, TAK; Methodology: TAK; Project administration: TAK, BHK; Visualization: YK, HMH; Writing-original draft: YK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
ARTICLE INFORMATION

- 1. Coccolini F, Roberts D, Ansaloni L, et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg 2018;13:7. PubMedPMC
- 2. Regner JL, Kobayashi L, Coimbra R. Surgical strategies for management of the open abdomen. World J Surg 2012;36:497–510. ArticlePubMedPDF
- 3. Chen Y, Ye J, Song W, Chen J, Yuan Y, Ren J. Comparison of outcomes between early fascial closure and delayed abdominal closure in patients with open abdomen: a systematic review and meta-analysis. Gastroenterol Res Pract 2014;2014:784056. ArticlePubMedPMCPDF
- 4. Nagashima F, Inoue S. A feasible operative treatment strategy for trauma patient with difficulties in closing the abdomen during open abdomen management (OAM) following damage control surgery-secondary publication. J Acute Care Surg 2020;10:83–9. ArticlePDF
- 5. Yetisir F, Sarer AE, Acar HZ, Aygar M. Delayed closure of 61 open abdomen patients based on an algorithm. Indian J Surg 2017;79:38–44. ArticlePubMedPMCPDF
- 6. Heller L, McNichols CH, Ramirez OM. Component separations. Semin Plast Surg 2012;26:25–8. ArticlePubMedPMC
- 7. Chiara O, Cimbanassi S, Biffl W, et al. International consensus conference on open abdomen in trauma. J Trauma Acute Care Surg 2016;80:173–83. ArticlePubMed
- 8. Sartelli M, Coccolini F, van Ramshorst GH, et al. WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg 2013;8:50. PubMedPMC
- 9. Capobianco CM, Zgonis T. An overview of negative pressure wound therapy for the lower extremity. Clin Podiatr Med Surg 2009;26:619–31. ArticlePubMed
- 10. Jones DA, Neves Filho WV, Guimaraes JS, Castro DA, Ferracini AM. The use of negative pressure wound therapy in the treatment of infected wounds. Case studies. Rev Bras Ortop 2016;51:646–51. PubMedPMC
- 11. Boele van Hensbroek P, Wind J, Dijkgraaf MG, Busch OR, Goslings JC. Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg 2009;33:199–207. ArticlePubMedPMC
- 12. Silverman RP. Acellular dermal matrix in abdominal wall reconstruction. Aesthet Surg J 2011;31(7 Suppl):24S–9S. ArticlePubMed
- 13. Caviggioli F, Klinger FM, Lisa A, et al. Matching biological mesh and negative pressure wound therapy in reconstructing an open abdomen defect. Case Rep Med 2014;2014:235930. ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite