Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Case Report
Pancreaticoduodenectomy as an option for treating a hemodynamically unstable traumatic pancreatic head injury with a pelvic bone fracture in Korea: a case report -
Sung Yub Jeong, MD1,2
 , Yoonhyun Lee, MD3
, Yoonhyun Lee, MD3 , Hojun Lee, MD2
, Hojun Lee, MD2
-
Journal of Trauma and Injury 2023;36(3):261-264.
DOI: https://doi.org/10.20408/jti.2022.0059
Published online: December 7, 2022
- 1,280 Views
- 28 Download
1Department of Surgery, Armed Forces Capital Hospital, Seongnam, Korea
2Armed Forces Trauma Center, Armed Forces Capital Hospital, Seongnam, Korea
3Department of Surgery, Armed Forces Seoul Center District Hospital, Seoul, Korea
- Correspondence to Hojun Lee, MD Armed Forces Trauma Center, Armed Forces Capital Hospital, 81 Saemaeul-ro 177 beon-gil, Bundang-gu, Seongnam 13574, Korea Tel: +82-31-789-2848 E-mail: hzl224@hanmail.net
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Pancreatic trauma occurs in 0.2% of patients with blunt trauma and 5% of severe abdominal injuries, which are associated with high mortality rates (up to 60%). Traumatic pancreatoduodenectomy (PD) has significant morbidity and appreciable mortality owing to complicating factors, associated injuries, and shock. The initial reconstruction in patients with severe pancreatic injuries aggravates their status by causing hypothermia, coagulopathy, and acidosis, which increase the risk for early mortality. A staging operation in which PD follows damage control surgery is a good option for hemodynamically unstable patients. We report the case of a patient who was treated by staging PD for an injured pancreatic head.
- Pancreatic trauma occurs in 0.2% of brunt trauma patients and 5% of severe abdominal injuries, which are associated with high morbidity and mortality rates [1]. The American Association for the Surgery of Trauma (AAST) scale for pancreatic injuries was introduced in 1990; these guidelines divide pancreatic injuries into five stages, and pancreaticoduodenectomy (PD) is the procedure of choice for grades 4 and 5 [2]. Operating on the pancreatic head is technically challenging and requires delicate resection and complex reconstruction. Such a procedure necessitates exceptional surgical training and expertise [3]. The initial reconstruction in severely injured patients with complex pancreatic injuries worsens their initial status by causing hypothermia, coagulopathy, and acidosis, which increase the risk of early mortality [4]. The concept of damage control surgery has been established in recent decades [5], and hemodynamically unstable patients have an initial damage control operation followed by subsequent PD and reconstruction once they are stable [6]. We report the case of a patient who was treated by staging PD for a pancreatic head injury.
INTRODUCTION
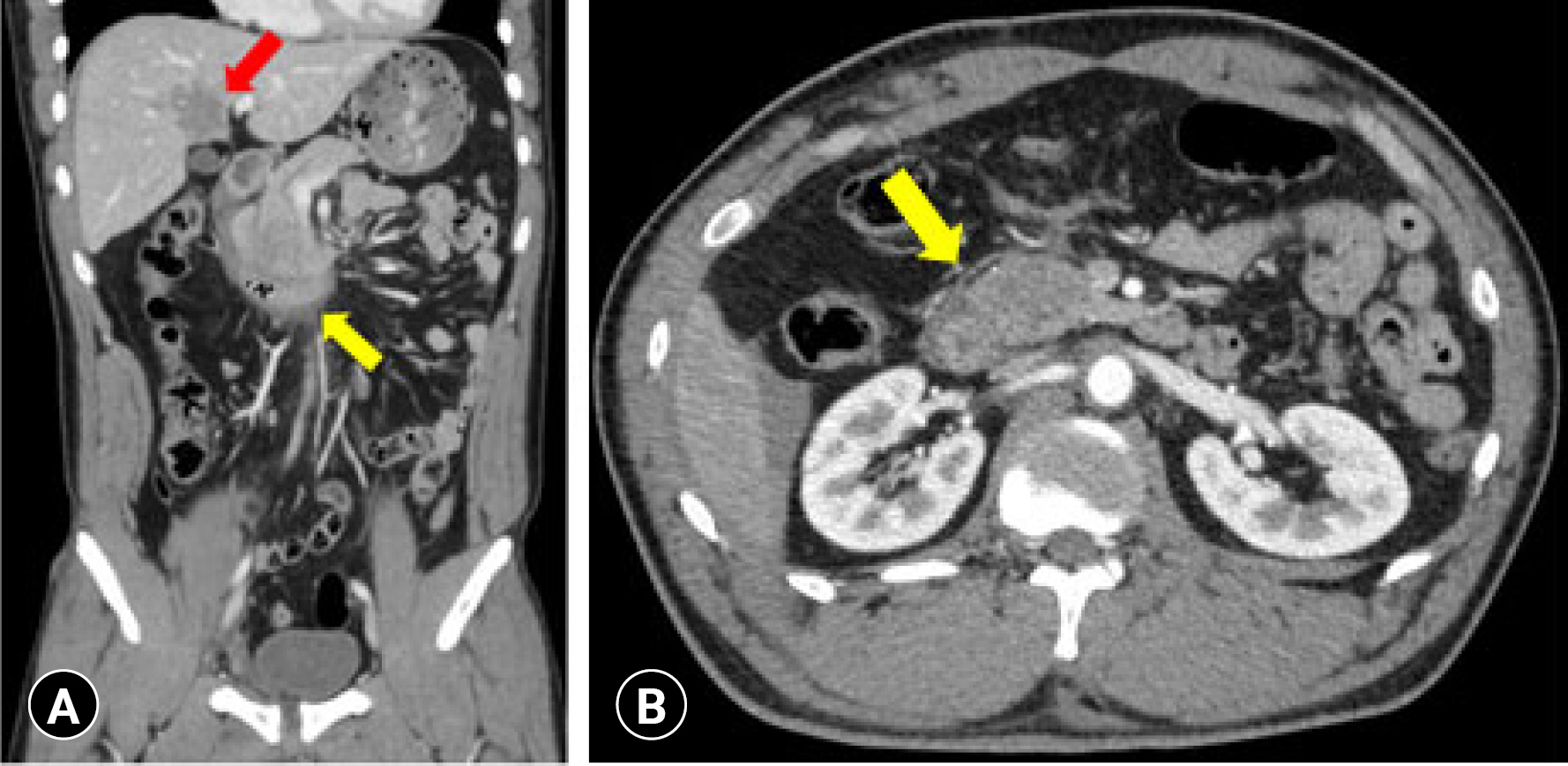
- A previously healthy 30-year-old male sergeant was transferred to the Armed Forces Trauma Center by air-ambulance from a community hospital. He had suffered a crush injury due to a military towing car accident. Contrast-enhanced abdominal-pelvic computed tomography (APCT) at the community hospital showed a pancreatic head injury, extensive hemoperitoneum, liver laceration (grade 2) (Fig. 1), and an open-book type pelvic bone fracture (Fig. 2A). The initial vital signs were a blood pressure of 80/60 mmHg, a heart rate of 112 beats/min, a respiratory rate of 18 breaths/min, and a temperature of 36.2 °C. Focused assessment with sonography for trauma showed positive results in the right flank area. Since the patient’s vital signs were unstable, we decided to perform an exploratory laparotomy without hesitation with the traumatic orthopedic team.
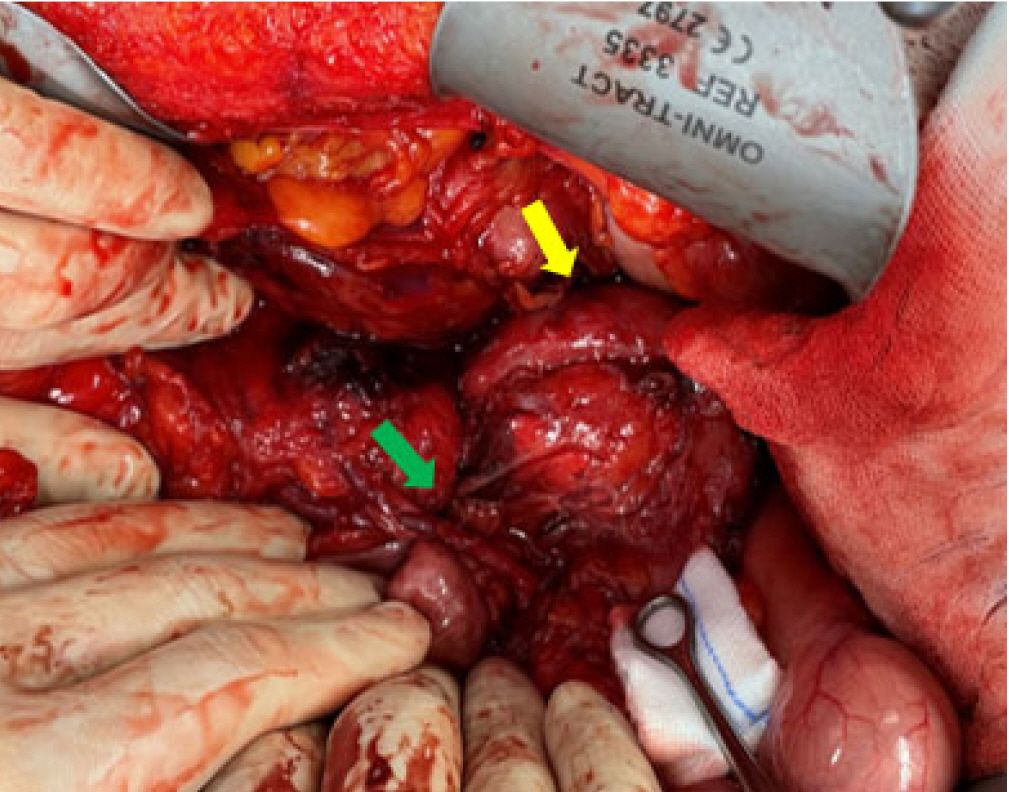
- Exploratory laparotomy was conducted with collaboration between the trauma team, hepato-biliary-pancreas (HBP) team, and orthopedics (OS) team. The grade 2 liver laceration was controlled with hemostatic gauze. Next, bleeding control was performed on the lateral side of the superior mesentery vein, the main pancreatic duct injury was identified, and the duodenal perforation site was repaired with primary sutures (Fig. 3). Two-branch indwelling Jackson-Pratt drains were placed around the pancreatic injury site to drain the pancreatic juices. During laparotomy, external screw fixation was simultaneously performed in the pelvic bone by the OS team (Fig. 2B). After damage control surgery was finished, the patient was sent to the trauma intensive care unit. At 24 hours postoperatively, the patient was resuscitated in the trauma intensive care unit and given a transfusion and fluid therapy until vital signs were stabilized.
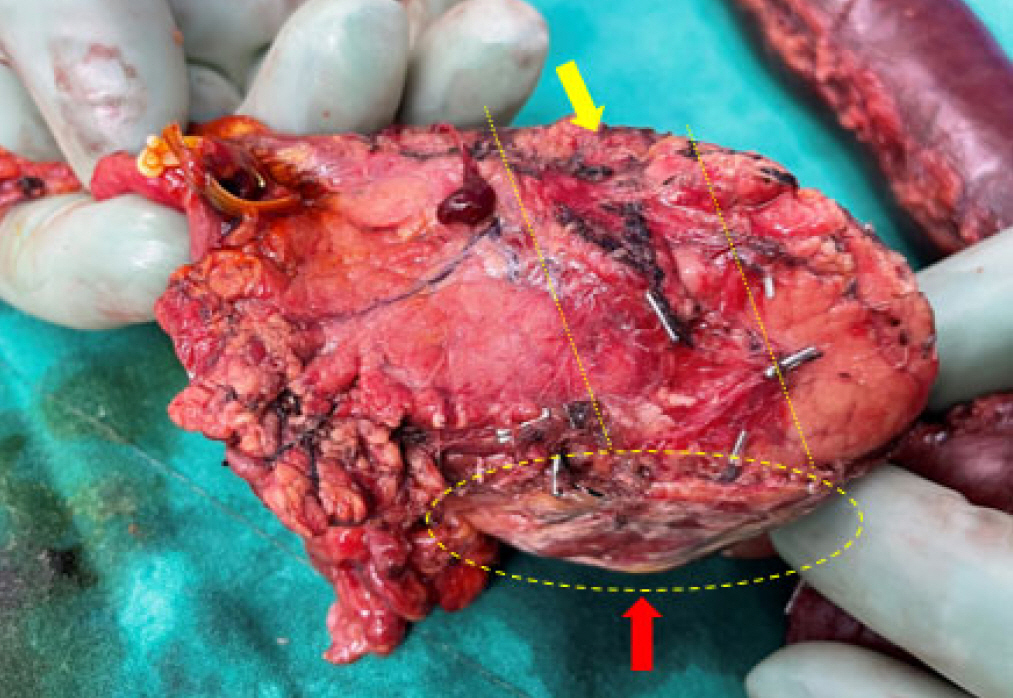
- The PD operation began 24 hours after the initial damage control surgery. The pancreatic head was crushed, the main duct was disrupted, and pancreatic juice leakage was confirmed (Fig. 4). The pancreas was resected at the neck level to maintain a healthy main duct and avoid pancreaticojejunostomy site leakage. Duct-to-mucosa anastomosis at the pancreaticojejunostomy was performed with a short silicone catheter inserted through the site of anastomosis. The postoperative course went smoothly. APCT detected no complications at postoperative day (POD) 7 and POD 28. The patient was discharged in good condition on POD 42 with an injury severity score of 50 without complications. New-onset diabetes mellites did not occur at postoperative 6 months.
- Ethics statement
- The study was approved by the Institutional Review Board of the Armed Forces Capital Hospital (No. AFCH IRB 2022-09-001). The Institutional Review Board waived the requirement for written informed consent. Our study was conducted in accordance with the Declaration of Helsinki.
CASE REPORT
- Howell et al. (as cited in Israr et al. [7]) were the first to report PD for treating trauma patients in 1961. PD for trauma is seldom necessary and should be reserved for severe pancreatic head injuries that cannot be preserved otherwise [8]. There are specific indications for PD for trauma. First, there needs to be extensive devitalization of the head of the pancreas or duodenum with no prospect of repair. Second, there needs to be a ductal disruption in the pancreatic head with an AAST grade of 5 and injuries to the duodenum and distal common bile duct. Lastly, there needs to be an injury to the ampulla of Vater, with a disruption of the main pancreatic duct from the duodenum [6,9].
- Operative mortality after blunt trauma to the pancreas has been reported in up to 60% of cases because of acute complications such as pancreatic juice leakage, pseudoaneurysm, and bile leakage. Moreover, despite trauma bay resuscitation, pancreatic injury patients have severe associated injuries and major blood loss, acidosis, coagulopathy, hypothermia, and persisting hypotension [4,9,10]. For these reasons, surgeons may face a dilemma regarding the need to perform damage control surgery followed by definite PD when encountering these patients. Additionally, the management of pancreatic injuries is complex and often requires a multidisciplinary approach. Experienced trauma and HBP surgeons, intensive care unit physicians, and radiologists should collaborate intensively to offer patients the best results. In our case, a multidisciplinary approach between the trauma, HBP, and OS teams started before the patient’s arrival.
- Numerous pancreatic injury patients are in a hemodynamically unstable condition, and since the introduction of the damage control strategy in 1983, staging PD has become an increasingly viable option that has decreased the high mortality rate of pancreatic injuries [11,12]. Our patient was hemodynamically unstable with hemoperitoneum and a pelvic bone fracture. For these reasons, our multidisciplinary hospital team decided on damage control surgery followed by PD. The PD was conducted by an experienced HBP team, which reduced the risk of acute postoperative complications.
- Our successful treatment of staging PD for a traumatic pancreatic injury demonstrates that PD after damage control surgery in hemodynamically unstable patients is a viable option.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
-
Author contributions
Conceptualization: all authors; Data curation: SYJ; Formal analysis: all authors; Methodology: all authors; Project administration: all authors; Visualization: SYJ; Writing–original draft: SYJ, HL; Writing–review & editing: all authors.
All authors read and approved the final manuscript.
-
Additional information
This study was presented at the 9th Pan-Pacific Trauma Congress (PPTC) in June 2022 in Gyeongju, Korea.
ARTICLE INFORMATION


- 1. Fisher M, Brasel K. Evolving management of pancreatic injury. Curr Opin Crit Care 2011;17:613–7. ArticlePubMed
- 2. Moore EE, Cogbill TH, Malangoni MA, et al. Organ injury scaling, II: pancreas, duodenum, small bowel, colon, and rectum. J Trauma 1990;30:1427–9. PubMed
- 3. Krige JE, Thomson SR. Operative strategies in pancreatic trauma: keep it safe and simple. S Afr J Surg 2011;49:106–9. PubMed
- 4. Wang GF, Li YS, Li JS. Damage control surgery for severe pancreatic trauma. Hepatobiliary Pancreat Dis Int 2007;6:569–71. PubMed
- 5. Iacono C, Zicari M, Conci S, et al. Management of pancreatic trauma: a pancreatic surgeon's point of view. Pancreatology 2016;16:302–8. ArticlePubMed
- 6. Krige JE, Nicol AJ, Navsaria PH. Emergency pancreatoduodenectomy for complex injuries of the pancreas and duodenum. HPB (Oxford) 2014;16:1043–9. ArticlePubMedPMC
- 7. Israr S, Rubalcava NS, Weinberg JA, Jones M, Gillespie TL. Management of biliary stricture following emergent pancreaticoduodenectomy for trauma: report of two cases. Cureus 2018;10:e2829. ArticlePubMedPMC
- 8. Subramanian A, Dente CJ, Feliciano DV. The management of pancreatic trauma in the modern era. Surg Clin North Am 2007;87:1515–32. ArticlePubMed
- 9. van der Wilden GM, Yeh D, Hwabejire JO, et al. Trauma whipple: do or don’t after severe pancreaticoduodenal injuries? An analysis of the National Trauma Data Bank (NTDB). World J Surg 2014;38:335–40. ArticlePubMedPDF
- 10. Grigorian A, Dosch AR, Delaplain PT, et al. The modern trauma pancreaticoduodenectomy for penetrating trauma: a propensity-matched analysis. Updates Surg 2021;73:711–8. ArticlePubMedPMCPDF
- 11. Rotondo MF, Schwab CW, McGonigal MD, et al. 'Damage control': an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993;35:375–82. PubMed
- 12. de Carvalho ME, Cunha AG. Pancreaticodudonectomy in trauma: one or two stages? Injury 2020;51:592–6. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Blunt abdominal trauma resulting in pancreatic injury in a pediatric patient in Australia: a case report
- Successful minimally invasive management using transcatheter arterial embolization in a hemodynamically stable elderly patient with mesenteric vascular injury in a hybrid emergency room system in Korea: a case report
- Endovascular treatment of traumatic iliac venous injury combined with phlegmasia cerulea dolens in Korea: a case report
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite