Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Original Article
Comparison of pediatric injury patterns before and during the COVID-19 pandemic in Korea: a retrospective study -
Geom Pil Nam, MD1
 , Woo Sung Choi, MD1
, Woo Sung Choi, MD1 , Jin-Seong Cho, MD1,2
, Jin-Seong Cho, MD1,2 , Yong Su Lim, MD1,2
, Yong Su Lim, MD1,2 , Jae-Hyug Woo, MD1,2
, Jae-Hyug Woo, MD1,2 , Jae Ho Jang, MD1,2
, Jae Ho Jang, MD1,2 , Jea Yeon Choi, MD1,2
, Jea Yeon Choi, MD1,2
-
Journal of Trauma and Injury 2023;36(4):343-353.
DOI: https://doi.org/10.20408/jti.2023.0053
Published online: December 22, 2023
- 650 Views
- 12 Download
1Department of Emergency Medicine, Gachon University Gil Medical Center, Incheon, Korea
2Department of Emergency Medicine, Gachon University College of Medicine, Incheon, Korea
- Correspondence to Woo Sung Choi, MD Department of Emergency Medicine, Gachon University Gil Medical Center, 21 Namdong-daero 774beon-gil, Namdong-gu, Incheon 21565, Korea Tel: +82-32-460-3015 Email: choiwoosung@gilhospital.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- The COVID-19 pandemic led to significant changes in the lifestyle patterns of children and affected the patterns of pediatric injuries. This study analyzed the changing patterns of pediatric injury overall and by age groups, based on the datasets before and during the COVID-19 pandemic.
-
Methods
- This study is based on the data of patients who presented with injuries at 23 hospital emergency departments participating in the Emergency Department-based Injury In-depth Surveillance (EDIIS) conducted by the Korea Disease Control and Prevention Agency. The surveillance data was categorized by injury mechanism, location, activity, and severity. We analyzed the injury patterns of pediatric patients aged 0 to 15 years. Subgroup analysis was conducted by age group in children aged 7 to 15 years, 1 to 6 years, and <1 year.
-
Results
- When comparing the COVID-19 pandemic period to the pre–COVID-19 period, the total number of pediatric patients with injuries decreased by 38.7%, while the proportions of in-home injuries (57.9% vs. 67.9%), and minor injuries (38.9% vs. 39.7%) increased. In the 7 to 15 years group, bicycle riding injuries (50.9% vs. 65.6%) and personal mobility device injuries (2.4% vs. 4.6%) increased. The 1 to 6 years group also showed an increase in bicycle accident injuries (15.8% vs. 22.4%). In the <1 year group, injuries from falls increased (44.5% vs. 49.9%). Self-harm injuries in the 7 to 15 years group also increased (1.6% vs. 2.8%).
-
Conclusions
- During the COVID-19 pandemic period, the overall number of pediatric injuries decreased, while injuries occurring at home and during indoor activities increased. Traffic accidents involving bicycles and personal mobility devices and self-harm injuries increased in the 7 to 15 years group. In the <1 year group, the incidence of falls increased. Medical and societal preparedness is needed so that we might anticipate these changes in the patterns of pediatric injuries during future infectious disease pandemics.
- Background
- COVID-19 was first reported in Wuhan, Hubei Province, China at the end of 2019. In the United States, the number of COVID-19 cases gradually increased between January and February 2020, and significantly increased in March 2020 [1]. On March 11, 2020, COVID-19 was declared a pandemic by the World Health Organization (WHO) [2]. On January 20, 2020, the first confirmed case of COVID-19 imported from Wuhan was reported in Korea. By March 31, 2020, Korea had a total of 9,786 confirmed cases of COVID-19, with 162 deaths and 4,216 individuals under nonhospital isolation [3]. To avoid overwhelming healthcare systems with the continuing increase in confirmed cases, home quarantine and social distancing measures were implemented worldwide. These COVID-19 containment measures led to significant changes in the lifestyle patterns of both adults and children, as well as shifts in the mechanism of traumatic injuries being seen in emergency departments [4].
- Previous studies reported that activities in schools and childcare facilities decreased while activities at home increased during the COVID-19 pandemic. This shift in activities led to changes in the patterns of injuries observed in emergency departments before and after the COVID-19 outbreak [5]. Specifically, it was found that blunt trauma and exercise-related injuries decreased, while penetrating injuries and intentional injuries increased [6]. However, most studies focused on adults, and those studies that targeted pediatric populations were limited to patients from a single hospital or high-severity institutions such as trauma centers.
- Objectives
- The purpose of this study was to analyze the changing patterns of pediatric injuries overall and by age groups, based on a large dataset from 23 hospital emergency departments, before and during the COVID-19 pandemic.
INTRODUCTION
- Ethics statement
- The study protocol was reviewed and approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GBIRB2023-177). The requirement for informed consent was waived due to the retrospective nature of the study. The study was conducted in compliance with the principles of the Declaration of Helsinki.
- Study design and patients
- This study was based on the data of patients who presented with injuries at 23 hospital emergency departments participating in the Emergency Department-based Injury In-depth Surveillance (EDIIS) conducted by the Korea Disease Control and Prevention Agency (KDCA; Cheongju, Korea). The study included 21 university hospitals and two general hospitals that were involved in the in-depth surveillance. Among them, 13 hospitals were in metropolitan areas, while the remaining 10 hospitals were distributed in various regions, with one or two hospitals per region. Each hospital was assigned a dedicated coordinator to collect the data. The collected data underwent primary verification by analyzing data integrity, including checking for duplicates and missing essential items. If errors were identified, the responsible researchers were asked to make corrections, and iterative quality management was performed to minimize error rates.
- Data collection
- The surveillance data included date of visit, age, sex, mode of arrival, mechanism of injury, location of injury, activity at the time of injury, emergency department treatment outcome, and the excess mortality ratio–adjusted Injury Severity Score (EMR-ISS). The mechanism of injury was classified into categories such as traffic accidents, slips, falls, blunt trauma, penetrating injuries, burns, intoxication, overexertion, foreign body insertion, and others. The location of injury was classified as home, schools/education facilities, sports facilities, roads and transportation facilities, commercial facilities, and others. The activity at the time of injury was surveyed and classified into categories including school activities, exercise, leisure activities, basic daily activities, and others.
- The EMR-ISS was calculated using the S and T codes of the International Classification of Diseases (ICD). Each diagnosis was assigned a severity score ranging from 1 to 5. The EMR-ISS was calculated by squaring the three highest scoring codes, regardless of the body region, and adding them together [7]. To assess the severity of trauma, the EMR-ISS was used and scores were classified as mild (<9), moderate (9–24), and severe (25–74) [8]. To analyze treatment outcomes, they were categorized as discharge after emergency department treatment, admission, intensive care unit (ICU) admission, surgery, and death.
- Statistical analysis
- The collected data were analyzed using SPSS ver. 24.0 (IBM Corp). The chi-square test was employed to compare the frequencies of categorical variables between groups. The Mann-Whitney U-test was used for univariate analysis of continuous variables. A P-value of <0.05 was considered statistically significant.
METHODS
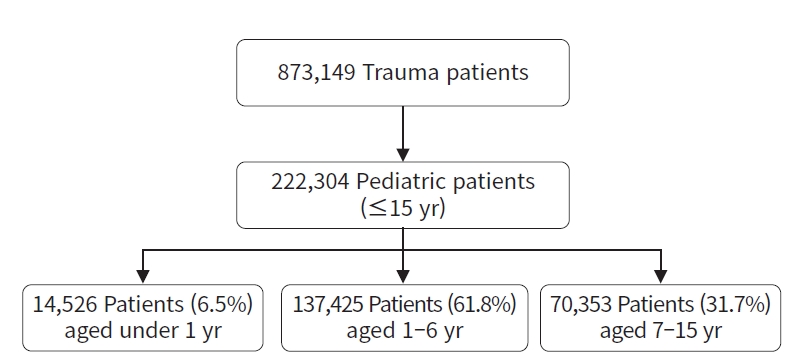
- The total number of injured patients treated in the 23 hospital emergency departments in Korea during the pre–COVID-19 period (March 12, 2018, to December 31, 2019) and the COVID-19 pandemic period (March 12, 2020, to December 31, 2021) was 873,149, of whom 222,304 were ≤15 years old. Among them, 14,526 patients (6.5%) were <1 year, 137,425 patients (61.8%) were 1 to 6 years, and 70,353 patients (31.7%) were 7 to 15 years (Fig. 1). Characteristics of the patients and their injuries are shown in Table 1.
- The number of pediatric patients 0 to 15 years old who were treated in the emergency department decreased by 38.7%, from 137,880 during the pre–COVID-19 period to 84,424 during the COVID-19 pandemic period. In both periods, the proportion of boys was higher (62.1% vs. 61.3%, P<0.001), and 1 to 6 years had the highest number of visits to the emergency department (61.3% vs. 62.7%, P<0.001). When comparing the pre–COVID-19 period to the COVID-19 pandemic period for mechanism of injury, blunt trauma decreased by 2.4 percentage points (30.9% vs. 28.5%), while falls increased by 1.3 percentage points (15.0% vs. 16.3%), foreign body insertion increased by 2.3 percentage points (7.7% vs. 10.0%), and traffic accidents decreased by 0.3 percentage points (6.5% vs. 6.2%). There were statistically significant differences in injury mechanisms between the two periods (P<0.001).
- During the COVID-19 pandemic, injuries occurred predominantly at home with a 10.0 percentage points higher frequency than the pre–COVID-19 period (57.9% vs. 67.9%). Injuries occurring in education facilities decreased 4.0 percentage points (9.2% vs. 5.2%), and there was a statistically significant decrease in injury rates associated with outdoor activities (P<0.001). Regarding injury intention, self-harm increased by 0.4 percentage points (0.5% vs. 0.9%). Comparison of the EMR-ISSs showed that severe injuries (2.9% vs. 2.8%) and moderate injuries (57.1% vs. 56.9%) decreased, while minor injuries increased (38.9% vs. 39.7%), with a statistically significant difference (P<0.001).
- In the subgroup analysis of pediatric patients aged 7 to 15 years (Table 2), the total number of patients decreased by 42.3%, with 44,615 in the pre–COVID-19 period and 25,738 in the COVID-19 pandemic period. The mechanism of injury showed a 5.9 percentage points decrease in blunt trauma (32.8% vs. 26.9%), while traffic accidents increased by 1.8 percentage points (12.8% vs. 14.6%).
- When considering location, injuries occurred predominantly at home during the pandemic, a 14.6 percentage points increase over the pre–COVID-19 period (32.6% vs. 47.2%). Injuries that occurred in education facilities showed a 10.5 percentage points decrease (18.7% vs. 8.2%), indicating a decrease in the occurrence of injuries associated with school-related outdoor activities.
- In terms of activity at the time of injury, in the COVID-19 pandemic there was a 5.7 percentage points decrease in injuries during educational activities compared to the pre–COVID-19 period (9.6% vs. 3.9%). Exercise-related injuries decreased by 5.7 percentage points (15.2% vs. 9.5%), while injuries during leisure activities increased by 5.2 percentage points (25.1% vs. 30.3%). Injuries during daily activities increased by 6.1 percentage points (42.3% vs. 48.4%). Regarding injury intention, self-harm increased by 1.2 percentage points (1.6% vs. 2.8%). Analysis of the EMR-ISS showed that severe injuries (3.6% vs. 3.5%) and moderate injuries (49.0% vs. 47.1%) decreased, while minor injuries increased (46.5% vs. 48.5%).
- In the subgroup analysis of patients aged 1 to 6 years who presented to the emergency departments with injuries (Table 3), the number of patients decreased by 37.3%, with 84,477 in the pre–COVID-19 period and 52,948 in the COVID-19 pandemic period. Blunt injuries decreased (31.2% vs. 30.6%), traffic accidents decreased (3.6% vs. 2.5%), and foreign body insertion increased by 2.2 percentage points (8.8% vs. 11.0%). During the COVID-19 pandemic period, injuries occurred predominantly at home, with a 7.3 percentage points increase compared to the pre–COVID-19 period (68.1% vs. 75.4%). Education facilities showed a 0.8 percentage points decrease (5.1% vs. 4.3%), reflecting a statistically significant decrease in injury rates associated with outdoor activities (P<0.001). In terms of the EMR-ISS, severe injuries (2.1% vs. 1.9%) and moderate injuries (60.4% vs. 60.8%) decreased, while minor injuries increased (36.3% vs. 36.8%).
- In the subgroup analysis of infants <1 year who presented to the emergency department (Table 4), there were 8,788 patients in the pre–COVID-19 period and 5,738 patients in the COVID-19 pandemic period, representing a decrease of 37.3%. In terms of injury mechanism, falls increased by 5.4 percentage points (44.5% vs. 49.9%), while blunt injuries decreased (17.7% vs. 15.8%). Regarding location, there was a 2.6 percentage points increase in injuries at home (89.0% vs. 91.5%). In terms of activity at the time of injury, daily activities increased by 1.0 percentage points (93.4% vs. 94.4%). The EMR-ISS showed that severe injuries (8.1% vs. 6.4%) and moderate injuries (65.9% vs. 65.3%) decreased, while minor injuries increased (25.1% vs. 27.6%).
- For detailed analysis of the mechanism of traffic accidents across all age groups, further subgroup analysis was performed comparing traffic accidents during the pre–COVID-19 and COVID-19 pandemic periods (Fig. S1). In infants under 1 year, vehicle accidents decreased by 1.2 percentage points (95.7% vs. 94.5%). In the 1 to 6 years group, there was an increase in bicycle accidents (15.8% vs. 22.4%) and pedestrian accidents (32.0% vs. 35.9%), as well as a 0.2 percentage points increase in personal mobility device accidents (4.2% vs. 4.4%), whereas, vehicle accidents decreased (47.1% vs. 35.8%). In the 7 to 15 years group, pedestrian accidents decreased by 8.8 percentage points (25.6% vs. 16.8%), and vehicle accidents decreased by 8.0 percentage points (18.9% vs. 10.9%). However, there was an increase of 14.7 percentage points in bicycle accidents (50.9% vs. 65.6%) and a 2.2 percentage points increase in personal mobility device accidents (2.4% vs. 4.6%).
RESULTS
- The COVID-19 pandemic resulted in significant changes in the lifestyle patterns of children, including their home environment, educational institutions, and outdoor activities. These changes also affected the injury patterns of pediatric trauma patients presenting to the emergency department. This study investigated the changes in pediatric trauma before and during the COVID-19 pandemic. Given that lifestyle patterns and types of injuries vary among different age groups, the analysis was conducted separately for children <1 year, 1 to 6 years, and 7 to 15 years, focusing on injury mechanisms, activities and locations at the time of injury, intent, and severity. An additional detailed analysis of traffic accidents was conducted.
- Incidence of injuries
- Other studies have analyzed the changes in pediatric trauma following the COVID-19 pandemic. Sheridan et al. [9] reported a significant decrease in the number of admissions and procedures related to acute pediatric trauma care at a level I trauma center (Cork University Hospital, Cork, Ireland) during the COVID-19 pandemic. Haddadin et al. [10] compared 30,289 infants seen in a single level I pediatric trauma center for acute respiratory illness and trauma between March and May from 2018 to 2020 and reported a 34% decrease in cases due to trauma. Bessoff et al. [11] investigated 8,772 patients across five level I and one level II pediatric trauma centers in the United States and found a 13% decrease in trauma-related cases in 2020. In our study, the pre–COVID-19 period included 137,880 patients, while the COVID-19 pandemic period included 84,424 patients, representing a decrease of 38.7% in pediatric injuries seen in the emergency department. This decrease can be attributed to various factors such as reduced outdoor activities and the closure of schools and commercial facilities, resulting in a decrease in factors that contribute to the incidence of trauma. Specifically, the frequency of blunt trauma, slipping, and falls decreased significantly, indicating an overall decrease in pediatric trauma mechanisms that account for a significant proportion of trauma cases (Table 1). This result is consistent with the significant reduction in sports-related injuries (e.g., blunt trauma and slipping) during the COVID-19 pandemic period, as reported by Fahy et al. [5].
- Increased injuries at home
- A decrease in the number of injuries does not necessarily mean that children were safer during the COVID-19 pandemic period. Fahy et al. [5] reported a 17% increase in trauma cases resulting from accidents within the home during the COVID-19 pandemic. In addition, Malige et al. [12] conducted a retrospective review of all injuries (1,112 patients) recorded in 42 hospitals from 2017 to 2020, and reported a higher proportion of injuries occurring at home during the COVID-19 pandemic compared to the pre–COVID-19 period (54.9% vs. 44.7%, P=0.01). In the present study, the frequency of blunt trauma, slipping, and falls decreased significantly (Table 1). However, injuries occurring in education facilities, sports facilities, and commercial facilities all decreased. In all age groups except those under 1 year, there was a decrease in the frequency of injuries during educational and exercise activities conducted outside the home, particularly a significant decrease in the 7 to 15 years group (Table 2). However, injuries during daily activities and leisure activities increased across all age groups. The increased frequency of leisure activities can be attributed to personal activities such as dog walking, children's play, watching movies, watching sports games, going to the cinema, having parties, going camping, and dancing. These findings indicate that homes have become a new risk environment for pediatric injuries during the era of infectious disease pandemics, emphasizing the need for preventive measures against the types of injuries that can occur at home and during indoor activities.
- Increased minor injuries
- Bessoff et al. [11] reported an increase in the proportion of severely injured patients (ISS, ≥25) based on analysis of hospital admissions in five level I and one level II pediatric trauma centers in the United States. Similarly, Malige et al. [12] reported higher ICU admission rates and higher mortality rates during the pandemic. However, in contrast to these overseas findings, our study showed a decrease in the proportion of moderate injuries and an increase in the proportion of mild injuries (Table 1). This trend of decreased severity can be attributed to the reduction in mechanisms such as blunt trauma, slipping, and falls, which can cause fractures and multiple injuries. Furthermore, the previously mentioned studies focused mainly on trauma centers, and primarily targeted the early stages of the COVID-19 pandemic. In contrast, our study included the initial isolation period from 2020 to 2021, encompassing the entire pandemic period, which may account for the differences observed. In addition, Sanford et al. [13] included penetrating injuries such as gunshot wounds/pellet gun injuries, as did Bessoff et al. [11] who included an analysis of penetrating injuries such as firearm injuries. However, firearm possession is illegal in Korea, making gunshot wounds rare. Therefore, cultural factors related to firearm use can be considered a contributing factor to the differences in severity between this study and previous studies.
- Increased injuries while riding a bicycle or personal mobility device
- According to Rajput et al. [14], there was a 73% decrease in the number of drivers and a consequent 46.6% decrease in the frequency of traffic accidents in March 2020 compared to the pre–COVID-19 pandemic period. Similarly, our study showed a decrease in the overall frequency of traffic accidents. However, when conducting a detailed analysis of the frequency and types of traffic accidents by age group, the frequency of traffic accidents for children aged <7 years decreased, but there was an increase observed in the group aged 7 to 15 years (Table 2). When conducting a subgroup analysis of traffic accidents in the 7 to 15 years group (Table 5), it was found that the proportion of bicycle accidents increased. There was also an increase in accidents involving personal mobility vehicles (Fig. S1). Consequently, although the overall rate of traffic accidents in the 7 to 15 years group increased, this was attributed to an increase in accidents involving bicycles and personal mobility devices rather than an increase in vehicle accidents. The increase in bicycle-related accidents among the 7 to 15 years group can be attributed to increased leisure time resulting from the decrease in structured activities and supervision during the COVID-19 pandemic period. In addition, the culture of avoiding public transportation and minimizing contact with others may have contributed to the increased use of bicycles. In fact, a study by Ko et al. [15] reported a significant increase in bicycle sales following the COVID-19 outbreak.
- Self-harm injuries
- Regarding self-harm injuries during the COVID-19 pandemic, Flynn-O’Brien et al. [16] reported an increase in intentional injuries among children based on socioeconomic status during the pandemic. de Oliveira et al. [17] also reported a significant increase in self-harm cases due to substance abuse or overdose among female adolescents who were more vulnerable to violence and self-neglect during the COVID-19 pandemic. In our study, there was an increase in self-harm injuries among children aged 7 to 15 years (Table 2). The subgroup analysis of injured 7- to 15-year patients who attempted self-harm showed a 1.7 percentage points increase in self-injury (28.6% vs. 30.3%) and a 5.7 percentage points increase in falls (6.9% vs. 12.6%). Substance abuse decreased (54.0% vs. 49.5%). Flynn-O’Brien et al. [16] reported an increase in firearm injuries among children under 12 years old, mainly during the first 6 months of the pandemic. However, firearm possession is not allowed in Korea, resulting in a low incidence of penetrating injuries related to firearms. These results may be associated with the stress and psychological distress experienced by children during the COVID-19 pandemic. Children in this age group are particularly vulnerable to the impact of social isolation and disruption in their daily lives, which can lead to loneliness, anxiety, and depression. School closures and reduced supervision compromised the important functions of social support and positive reinforcement, which exacerbated negative emotions. Lewit et al. [18] reported that the economic downturn caused by the COVID-19 pandemic increased the rate of self-harm among children. Consequently, the increase in pediatric self-harm injuries in our study may have also been affected by family conflicts, financial stress, and the economic difficulties faced by families during the COVID-19 pandemic.
- Infant fall injuries
- Shi et al. [19] reported an increase in falls among the pediatric population (average age, 7 years) in New Hampshire in the United States. In our study, the proportion of falls among all injuries was analyzed for each age group. The results showed a relatively significant increase in the proportion of falls in the under 1 year group (Table 4, Fig. S1) . This could be attributed to the COVID-19 pandemic, which led to working at home and the closure of daycares and educational institutions. This newly increased telecommuting environment resulted in an increased workload for parents in households with children. Parents performed the roles of caregivers and day workers, all within the confines of their home. This significantly increased workload inevitably affected the likelihood of accidents, especially the increased rate of injuries from falls in children <1 year old.
- Limitations
- This study had some limitations. First, although 24 hospitals participated, they were mainly located in metropolitan and urban areas, and the survey focused on university hospitals, making it difficult to generalize the results to the entire country. Second, the study primarily targeted tertiary hospitals and did not include pediatric patients visiting primary or secondary healthcare facilities. Conducting a survey primarily in tertiary hospitals may introduce a selection bias since it includes patients with more severe conditions or injuries that may not accurately reflect the injury trends in the general pediatric population. Third, there was a limitation in the data collection of ISS; this study analyzed injury severity based on the EMR-ISS, which may less accurately reflect the severity of injuries.
- Conclusions
- During the COVID-19 pandemic period, the overall number of pediatric injuries decreased, while injuries occurring at home and during indoor activities increased. Traffic accidents involving bicycles and personal mobility devices increased among the 7 to 15 years, as did self-harm injuries. In the <1 year group, the incidence of falls increased. Medical and societal preparedness is needed to anticipate these changes in the patterns of pediatric injuries in future infectious disease pandemics.
DISCUSSION
-
Author contributions
Conceptualization: WSC, JSC; Data curation: GPN, JSC; Formal analysis: GPN, WSC, JYC, YSL; Methodology: GPN, YSL, JYC, JHW; Project administration: GPN, WSC, JHJ, JSC; Visualization: WSC, JHW, JHJ; Writing– original draft: GPN; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION
Supplementary materials
Fig. S1.
| Variable |
No. of patients (%) |
P-value | |
|---|---|---|---|
| Pre–COVID-19 (n=137,880) | COVID-19 (n=84,424) | ||
| Sex | <0.001 | ||
| Male | 85,684 (62.1) | 51,759 (61.3) | |
| Female | 52,196 (37.9) | 32,665 (38.7) | |
| Age (yr) | <0.001 | ||
| <1 | 8,788 (6.4) | 5,738 (6.8) | |
| 1–6 | 84,477 (61.3) | 52,948 (62.7) | |
| 7–15 | 44,615 (32.3) | 25,738 (30.5) | |
| Injury mechanism | <0.001 | ||
| Traffic accident | 8,950 (6.5) | 5,194 (6.2) | |
| Slip and fall | 32,125 (23.3) | 19,494 (23.1) | |
| Fall from a height | 20,625 (15.0) | 13,749 (16.3) | |
| Blunt force | 42,549 (30.9) | 24,040 (28.5) | |
| Penetrating | 9,653 (7.0) | 6,287 (7.4) | |
| Overexertion/overuse | 7,040 (5.1) | 3,599 (4.3) | |
| Burn | 3,272 (2.4) | 1,597 (1.9) | |
| Poisoning | 1,818 (1.3) | 1,320 (1.6) | |
| Insertion of foreign objects | 10,668 (7.7) | 8,430 (10.0) | |
| Other | 1,180 (0.8) | 714 (0.7) | |
| Location | <0.001 | ||
| Home | 79,882 (57.9) | 57,319 (67.9) | |
| Education facility | 12,659 (9.2) | 4,425 (5.2) | |
| Sports facility | 6,331 (4.6) | 2,718 (3.2) | |
| Transportation facility | 17,518 (12.7) | 9,543 (11.3) | |
| Social facility | 16,540 (12.0) | 7,625 (9.0) | |
| Other | 4,950 (3.6) | 2,794 (3.4) | |
| Activity | <0.001 | ||
| Indoor (daily activity) | 92,222 (66.9) | 59,175 (70.1) | |
| Outdoor | |||
| Education | 7,095 (5.1) | 2,315 (2.7) | |
| Exercise | 7,673 (5.6) | 2,867 (3.4) | |
| Leisurea) | 25,574 (18.5) | 17,436 (20.7) | |
| Other | 5,316 (3.9) | 2,631 (3.1) | |
| Transportation by ambulance | 14,473 (10.5) | 9,735 (11.5) | <0.001 |
| Intention | <0.001 | ||
| Unintentional | 135,595 (98.3) | 82,701 (98.0) | |
| Self-harm | 696 (0.5) | 736 (0.9) | |
| Violence | 1,482 (1.2) | 937 (1.1) | |
| Other | 107 (0.1) | 50 (0.0) | |
| Time of injury | <0.001 | ||
| 00:00–0:800 | 6,640 (4.8) | 4,114 (4.9) | |
| 08:00–16:00 | 50,178 (36.4) | 28,423 (33.7) | |
| 16:00–24:00 | 80,774 (58.7) | 51,766 (61.3) | |
| Unknown | 288 (0.2) | 121 (0.1) | |
| ED disposition | <0.001 | ||
| Discharge | 131,870 (95.6) | 80,049 (94.8) | |
| Admission | |||
| General ward | 4,518 (3.3) | 3,123 (3.7) | |
| Intensive care unit | 695 (0.5) | 522 (0.6) | |
| Operation | 739 (0.5) | 683 (0.8) | |
| Death | 58 (0.1) | 47 (0.1) | |
| EMR-ISS | <0.001 | ||
| Mild (<9) | 53,669 (38.9) | 33,541 (39.7) | |
| Moderate (9–24) | 78,694 (57.1) | 48,074 (56.9) | |
| Severe (>24) | 4,047 (2.9) | 2,273 (2.8) | |
| Unknown | 1,470 (1.1) | 536 (0.6) | |
| Variable |
No. of patients (%) |
P-value | |
|---|---|---|---|
| Pre–COVID-19 (n=44,615) | COVID-19 (n=25,738) | ||
| Injury mechanism | <0.001 | ||
| Traffic accident | 5,695 (12.8) | 3,759 (14.6) | |
| Slip and fall | 9,652 (21.6) | 5,513 (21.4) | |
| Fall from a height | 4,039 (9.1) | 2,630 (10.2) | |
| Blunt force | 14,640 (32.8) | 6,913 (26.9) | |
| Penetrating | 3,798 (8.5) | 2,530 (9.8) | |
| Overexertion/overuse | 2,459 (5.5) | 1,056 (4.1) | |
| Burn | 800 (1.8) | 439 (1.7) | |
| Poisoning | 638 (1.4) | 539 (2.1) | |
| Insertion of foreign objects | 2,543 (5.7) | 2,127 (8.3) | |
| Other | 351 (0.8) | 232 (0.9) | |
| Location | <0.001 | ||
| Home | 14,572 (32.6) | 12,153 (47.2) | |
| Education facility | 8,344 (18.7) | 2,120 (8.2) | |
| Sports facility | 5,211 (11.7) | 2,239 (8.7) | |
| Transportation facility | 8,817 (19.8) | 5,293 (20.6) | |
| Social facility | 5,708 (12.8) | 2,798 (10.9) | |
| Other | 1,963 (4.4) | 1,135 (4.4) | |
| Activity | <0.001 | ||
| Indoor (daily activity) | 18,869 (42.3) | 12,467 (48.4) | |
| Outdoor | |||
| Education | 4,285 (9.6) | 995 (3.9) | |
| Exercise | 6,767 (15.2) | 2,451 (9.5) | |
| Leisurea) | 11,230 (25.1) | 7,800 (30.3) | |
| Other | 3,464 (7.8) | 2,025 (7.9) | |
| Intention | <0.001 | ||
| Unintentional | 42,551 (95.4) | 24,170 (93.9) | |
| Self-harm | 693 (1.5) | 733 (2.8) | |
| Violence | 1,323 (3.0) | 817 (3.3) | |
| Other | 48 (0.1) | 18 (0.0) | |
| EMR-ISS | <0.001 | ||
| Mild (<9) | 20,767 (46.5) | 12,486 (48.5) | |
| Moderate (9–24) | 21,851 (49.0) | 12,122 (47.1) | |
| Severe (>24) | 1,595 (3.6) | 911 (3.5) | |
| Unknown | 402 (0.9) | 219 (0.9) | |
| Variable |
No. of patients (%) |
P-value | |
|---|---|---|---|
| Pre–COVID-19 (n=84,477) | COVID-19 (n=52,948) | ||
| Injury mechanism | <0.001 | ||
| Traffic accident | 3,024 (3.6) | 1,344 (2.5) | |
| Slip and fall | 21,631 (25.6) | 13,497 (25.5) | |
| Fall from a height | 12,675 (15.0) | 8,258 (15.6) | |
| Blunt force | 26,350 (31.2) | 16,217 (30.6) | |
| Penetrating | 5,446 (6.4) | 3,506 (6.6) | |
| Overexertion/overuse | 4,223 (5.0) | 2,318 (4.4) | |
| Burn | 2,018 (2.4) | 936 (1.8) | |
| Poisoning | 981 (1.2) | 663 (1.3) | |
| Insertion of foreign objects | 7,418 (8.8) | 5,818 (11.0) | |
| Other | 711 (0.8) | 391 (0.7) | |
| Location | <0.001 | ||
| Home | 57,492 (68.1) | 39,913 (75.4) | |
| Education facility | 4,290 (5.1) | 2,285 (4.3) | |
| Sports facility | 1,116 (1.3) | 478 (0.9) | |
| Transportation facility | 8,186 (9.7) | 4017 (7.6) | |
| Social facility | 10,541 (12.5) | 4,677 (8.8) | |
| Other | 2,852 (3.3) | 1,578 (3.0) | |
| Activity | <0.001 | ||
| Indoor (daily activity) | 65,149 (77.1) | 41,292 (78.0) | |
| Outdoor | |||
| Education | 2,798 (3.3) | 1,310 (2.5) | |
| Exercise | 905 (1.1) | 416 (0.8) | |
| Leisurea) | 13,935 (16.5) | 9,393 (17.7) | |
| Other | 1,690 (2.0) | 537 (1.0) | |
| Intention | 0.584 | ||
| Unintentional | 84,275 (99.7) | 52,814 (99.8) | |
| Self-harm | 3 (0.0) | 3 (0.0) | |
| Violence | 145 (0.2) | 103 (0.2) | |
| Other | 54 (0.1) | 28 (0.0) | |
| EMR-ISS | <0.001 | ||
| Mild (<9) | 30,694 (36.3) | 19,471 (36.8) | |
| Moderate (9–24) | 51,053 (60.4) | 32,205 (60.8) | |
| Severe (>24) | 1,740 (2.1) | 998 (1.9) | |
| Unknown | 990 (1.2) | 274 (0.5) | |
| Variable |
No. of patients (%) |
P-value | |
|---|---|---|---|
| Pre–COVID-19 (n=8,788) | COVID-19 (n=5,738) | ||
| Injury mechanism | <0.001 | ||
| Traffic accident | 231 (2.6) | 91 (1.6) | |
| Slip and fall | 842 (9.6) | 484 (8.4) | |
| Fall from a height | 3,911 (44.5) | 2,861 (49.9) | |
| Blunt force | 1,559 (17.7) | 910 (15.8) | |
| Penetrating | 409 (4.7) | 251 (4.4) | |
| Overexertion/overuse | 358 (4.1) | 225 (3.9) | |
| Burn | 454 (5.2) | 222 (3.9) | |
| Poisoning | 199 (2.3) | 118 (2.0) | |
| Insertion of foreign objects | 707 (8.0) | 485 (8.5) | |
| Other | 118 (1.3) | 91 (1.6) | |
| Location | <0.001 | ||
| Home | 7,818 (89.0) | 5,253 (91.5) | |
| Education facility | 25 (0.3) | 20 (0.3) | |
| Sports facility | 4 (0.0) | 1 (0.0) | |
| Transportation facility | 515 (5.9) | 233 (4.1) | |
| Social facility | 291 (3.3) | 150 (2.6) | |
| Other | 135 (1.5) | 81 (1.5) | |
| Activity | 0.007 | ||
| Indoor (daily activity) | 8,204 (93.4) | 5,416 (94.4) | |
| Outdoor | |||
| Education | 12 (0.1) | 10 (0.2) | |
| Exercise | 1 | 0 | |
| Leisurea) | 409 (4.7) | 243 (4.2) | |
| Other | 162 (1.8) | 69 (1.2) | |
| Intention | 0.207 | ||
| Unintentional | 8,769 (99.8) | 5,717 (99.7) | |
| Self-harm | 0 | 0 | |
| Violence | 14 (0.2) | 17 (0.3) | |
| Other | 5 (0.1) | 4 (0.1) | |
| EMR-ISS | <0.001 | ||
| Mild (<9) | 2,208 (25.1) | 1,584 (27.6) | |
| Moderate (9–24) | 5,790 (65.9) | 3,747 (65.3) | |
| Severe (>24) | 712 (8.1) | 364 (6.4) | |
| Unknown | 78 (0.9) | 43 (0.7) | |
| Mechanism |
No. of patients (%) by age group |
|||||
|---|---|---|---|---|---|---|
|
<1 yr (n=322) |
1–6 yr (n=4,316) |
7–15 yr (n=9,245) |
||||
| Pre–COVID-19 (n=231) | COVID-19 (n=91) | Pre–COVID-19 (n=2,995) | COVID-19 (n=1,321) | Pre–COVID-19 (n=5,566) | COVID-19 (n=3,679) | |
| Pedestrian | 6 (2.6) | 4 (4.4) | 967 (32.0) | 483 (35.9) | 1,457 (25.6) | 630 (16.8) |
| Bicycle | 2 (0.9) | 0 | 477 (15.8) | 301 (22.4) | 2,900 (50.9) | 2,467 (65.6) |
| Personal mobility devicea) | 2 (0.9) | 1 (1.1) | 127 (4.2) | 59 (4.4) | 134 (2.4) | 173 (4.6) |
| Vehicle | 221 (95.6) | 86 (94.5) | 1,424 (47.1) | 478 (35.8) | 1,075 (18.9) | 409 (10.9) |
- 1. Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RS, Horvat CM. Trends in US pediatric hospital admissions in 2020 compared with the decade before the COVID-19 pandemic. JAMA Netw Open 2021;4:e2037227ArticlePubMedPMC
- 2. Li J, Shen X, Shao J, et al. How to manage pediatric orthopaedic patients: strategies to provide safer care during the COVID-19 outbreak in Wuhan, People’s Republic of China. J Bone Joint Surg Am 2020;102:e86PubMed
- 3. JYC. COVID-19 in South Korea. Postgrad Med J 2020;96:399–402. ArticlePubMedPDF
- 4. Yarımkaya E, Esenturk OK. Promoting physical activity for children with autism spectrum disorders during Coronavirus outbreak: benefits, strategies, and examples. Int J Dev Disabil 2020;68:430–5. ArticlePubMedPMC
- 5. Fahy S, Moore J, Kelly M, Flannery O, Kenny P. Analysing the variation in volume and nature of trauma presentations during COVID-19 lockdown in Ireland. Bone Jt Open 2020;1:261–6. ArticlePubMedPMCPDF
- 6. Johnson MA, Halloran K, Carpenter C, et al. Changes in pediatric sports injury presentation during the COVID-19 pandemic: a multicenter analysis. Orthop J Sports Med 2021;9:23259671211010826. ArticlePubMedPMCPDF
- 7. Kim J, Shin SD, Im TH, et al. Development and validation of the excess mortality ratio-adjusted Injury Severity Score using the International Classification of Diseases 10th Edition. Acad Emerg Med 2009;16:454–64. ArticlePubMed
- 8. Park SH, Min JY, Cha WC, Jo IJ, Kim T. National surveillance of injury in children and adolescents in the Republic of Korea: 2011-2017. Int J Environ Res Public Health 2020;17:9132. ArticlePubMedPMC
- 9. Sheridan GA, Nagle M, Russell S, et al. Pediatric trauma and the COVID-19 pandemic: a 12-year comparison in a level-1 trauma center. HSS J 2020;16(Suppl 1):92–6. ArticlePubMedPMCPDF
- 10. Haddadin Z, Blozinski A, Fernandez K, et al. Changes in pediatric emergency department visits during the COVID-19 pandemic. Hosp Pediatr 2021;11:e57–60. ArticlePubMedPDF
- 11. Bessoff KE, Han RW, Cho M, et al. Epidemiology of pediatric trauma during the COVID-19 pandemic shelter in place. Surg Open Sci 2021;6:5–9. ArticlePubMedPMC
- 12. Malige A, Deemer A, Sobel AD. The effect of COVID-19 on pediatric traumatic orthopaedic injuries: a database study. J Am Acad Orthop Surg Glob Res Rev 2022;6:e22.00012ArticlePubMedPMC
- 13. Sanford EL, Zagory J, Blackwell JM, Szmuk P, Ryan M, Ambardekar A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg 2021;56:918–22. ArticlePubMedPMC
- 14. Rajput K, Sud A, Rees M, Rutka O. Epidemiology of trauma presentations to a major trauma centre in the North West of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg 2021;47:631–6. ArticlePubMedPDF
- 15. Ko BS, Cho SH, Noh DY, Kim JG. Epidemiological characteristics of bicycle-related injuries with the emergence of the COVID-19. Korean J Sports Med 2021;39:110–6. Article
- 16. Flynn-O’Brien KT, Collings AT, Farazi M, et al. Pediatric injury trends and relationships with social vulnerability during the COVID-19 pandemic: a multi-institutional analysis. J Trauma Acute Care Surg 2023;94:133–40. ArticlePubMed
- 17. de Oliveira SM, Galdeano EA, da Trindade EM, et al. Epidemiological study of violence against children and its increase during the COVID-19 pandemic. Int J Environ Res Public Health 2021;18:10061. ArticlePubMedPMC
- 18. Lewit RA, Kotagal M, Duron VP, et al. Association of economic recession and social distancing with pediatric non-accidental trauma during COVID-19. J Surg Res 2022;276:110–9. ArticlePubMedPMC
- 19. Shi Y, Kvasnovsky C, Khan S, et al. Impact of the COVID-19 pandemic on trauma activations at a pediatric level 1 trauma center in New York. Pediatr Surg Int 2021;37:1409–14. ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Changes in interpersonal violence and utilization of trauma recovery services at an urban trauma center in the United States during the COVID-19 pandemic: a retrospective, comparative study
- Usefulness of presepsin as a prognostic indicator for patients with trauma in the emergency department in Korea: a retrospective study
- No frequency change of prehospital treatments by emergency medical services providers for traumatic cardiac arrest patients before and after the COVID-19 pandemic in Korea: an observational study
- The practicality of interleukin-6 in prognosis of blunt chest trauma in Korea: a retrospective study
- Factors associated with the injury severity of falls from a similar height and features of the injury site in Korea: a retrospective study
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


