Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Original Article
No frequency change of prehospital treatments by emergency medical services providers for traumatic cardiac arrest patients before and after the COVID-19 pandemic in Korea: an observational study -
Ju Heon Lee, MD
 , Hyung Il Kim, MD
, Hyung Il Kim, MD
-
Journal of Trauma and Injury 2023;36(3):172-179.
DOI: https://doi.org/10.20408/jti.2023.0009
Published online: August 2, 2023
- 977 Views
- 59 Download
Department of Emergency Medicine, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- Correspondence to Hyung Il Kim, MD Department of Emergency Medicine, Dankook University Hospital, Dankook University College of Medicine, 201 Manghyang-ro, Dongnam-gu, Cheonan 31116, Korea Tel: +81-041-550-6840 Email: hilovesjj@naver.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Out-of-hospital traumatic cardiac arrest (TCA) often has a poor prognosis despite rescue efforts. Although the incidence and mortality of out-of-hospital cardiac arrest have increased, bystander cardiopulmonary resuscitation (CPR) has decreased in some countries during the COVID-19 pandemic. In the prehospital setting, immediate treatment of cardiac arrest is required without knowing the patient’s COVID-19 status. Because COVID-19 is usually transmitted through the respiratory tract, airway management can put medical personnel at risk for infection. This study explored whether on-scene treatments involving CPR for TCA patients changed during the COVID-19 pandemic in Korea.
-
Methods
- This retrospective study used data from emergency medical services (EMS) run sheets in Gangwon Province from January 2019 to December 2021. Patients whose initial problem was cardiac arrest and who received CPR were included. Data in 2019 were classified as pre–COVID-19 and all subsequent data (from 2020 and 2021) as post–COVID-19. Age, sex, possible cause of cardiac arrest, and treatments including airway maneuvers, oropharyngeal airway (OPA) or i-gel insertion, endotracheal intubation (ETI), bag-valve mask (BVM) ventilation, intravenous (IV) line establishment, neck collar application, and wound dressing with hemostasis were investigated.
-
Results
- During the study period, 2,007 patients received CPR, of whom 596 patients had TCA and 367 had disease-origin cardiac arrest (DCA). Among the patients with TCA, 192 (32.2%) were pre–COVID-19 and 404 (67.8%) were post–COVID-19. In the TCA group, prehospital treatments did not decrease. The average frequencies were 59.7% for airway maneuvers, 47.5% for OPA, 57.4% for BVM, and 51.3% for neck collar application. The rates of ETI, i-gel insertion, and IV-line establishment increased. The treatment rate for TCA was significantly higher than that for DCA.
-
Conclusions
- Prehospital treatments by EMS workers for patients with TCA did not decrease during the COVID-19 pandemic. Instead, the rates of ETI, i-gel insertion, and IV-line establishment increased.
- Background
- Advances in emergency care such as the establishment of trauma centers, helicopter transport of patients, and trauma education for doctors and emergency medical technicians (EMTs) have improved the survival of patients with severe trauma. Nonetheless, traumatic cardiac arrest (TCA) has a poor prognosis, and its survival is reported to be lower than that of non-TCA [1–3]. Since the rapid transfer of patients with major trauma is critical, the Korean emergency medical services (EMS) recommend <10 minutes of on-scene stay time after rescue, and transfer to an appropriate trauma center while performing essential treatments to maintain airway, breathing, and circulation [4].
- The spread of COVID-19 around the world created medical crises and led to many changes in public health systems. In Korea, the first COVID-19 case was reported in January 2020, and as of February 2023, 30 million people have been diagnosed and 33,000 have died [5,6]. Since COVID-19 is highly contagious, the National Fire Agency of Korea established nationwide guidelines in February 2020, calling for all EMTs to wear personal protective equipment (PPE) to reduce the spread of secondary infection to other patients and to keep EMTs safe. Because COVID-19 is usually transmitted through the respiratory tract, management of a patient’s airway can expose medical personnel to infection. However, it is difficult to know a patient’s precise condition at the scene where immediate treatment is required. While the patient's condition is unstable in the prehospital or emergency department setting, there may be minimal information available, including COVID-19 status. This is particularly true when responding to a patient in cardiac arrest, where cardiopulmonary resuscitation (CPR) and accompanying airway management should be performed without delay, exposing medical personnel to respiratory infectious diseases.
- Objectives
- This study investigated whether on-scene treatments involving CPR for patients with TCA changed during the COVID-19 pandemic in Korea.
INTRODUCTION
- Ethics statement
- Approval of the Institutional Review Board was not required because this was a retrospective study and did not include personal information except for patients’ sex and age.
- Study design
- This is a case series. This retrospective study analyzed the data from EMS run sheets.
- Study period and participants
- The EMS of Korea is organized by the National Fire Agency, and there are 17 fire headquarters located in metropolitan cities and provinces. When an emergency call is received and EMS personnel are dispatched, an EMS run sheet (recording sheet) is created each time a patient is treated and transferred. This retrospective study analyzed the data from these EMS run sheets.
- We analyzed data from January 2019 to December 2021 on patients in Gangwon Province who required EMS services for cardiac arrest and received CPR. Because the first COVID-19 patient was reported in January 2020 in Korea, data in 2019 were classified as pre–COVID-19 and data in 2020 and 2021 were classified as post–COVID-19. The inclusion criteria were limited to patients who received CPR by EMS personnel in response to an initial call of cardiac arrest. Cases in which help was requested for other initial symptoms such as dyspnea without cardiac arrest, but then developed cardiac arrest during transport were excluded. Patients who were not given CPR (e.g., do-not-resuscitate [DNR] status), were transported by helicopter, or had incomplete records were also excluded. Non-TCA cases included all patients who experienced arrest due to non-cardiac origins; for example, disease, hanging, or drowning. Gangwon Province has an area of 20,569 km2 with a population of approximately 1.54 million. As of 2021, there were 246 level I EMTs (24.3%), 390 level II EMTs (38.5%), 114 nurses (11.2%), and 264 other designations (26.0%), for a total of 1,014 emergency rescue workers in Gangwon Province. In addition, for approximately 80% of calls, EMTs were dispatched in teams of three. The patients’ age, sex, possible cause of cardiac arrest (identified at the scene), and treatments performed during CPR (airway maneuvers, oropharyngeal airway [OPA], or i-gel [Intersurgical] insertion, endotracheal intubation [ETI], bag-valve mask [BVM] ventilation, intravenous [IV] line establishment, neck collar application, and wound dressing with hemostasis) were analyzed.
- Statistics
- Categorical data were expressed as frequency and percentage. Continuous data were expressed as averages and standard deviations. Comparisons were calculated using the chi-square test. IBM SPSS ver. 26.0 (IBM Corp) was used for analysis, and statistical significance was set at a P-value <0.05.
METHODS
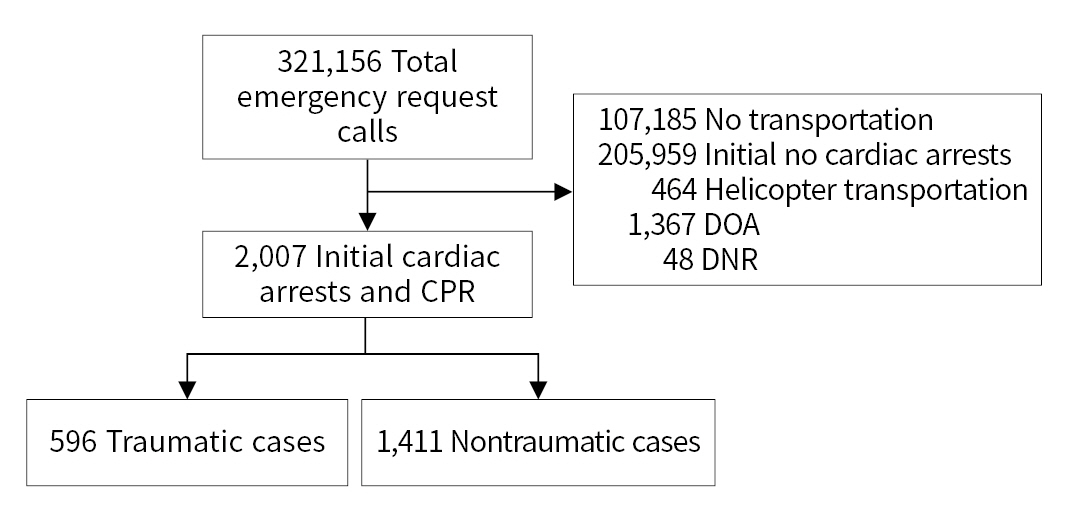
- During the 3-year study period, 321,156 emergency request calls were received, encompassing 107,185 patients who were not transferred, 205,959 cases without initial cardiac arrest, and 2,007 patients with initial cardiac arrest who received CPR (Fig. 1). Among the 2,007 patients who met our study criteria, help was dispatched for 616 in the pre–COVID-19 stage and 1,391 in the post–COVID-19 stage. The average age of the study patients was 56.9 years, and 69.6% were male. There were 596 patients with TCA, of whom 192 (32.2%) were in the pre–COVID-19 stage and 404 (67.8%) were in the post–COVID-19 stage. There were 367 patients with disease-origin cardiac arrest (DCA), of whom 70 (19.1%) and 297 (80.9%) were in the pre– and post–COVID-19 stages, respectively. There were 1,411 non-TCA patients, with 424 (30.0%) and 987 patients (70.0%) in the pre– and post–COVID-19 stages, respectively. Cardiac arrest due to disease and hanging in the post–COVID-19 stage increased compared to the pre–COVID-19 stage. No other statistically significant differences were found (Table 1).
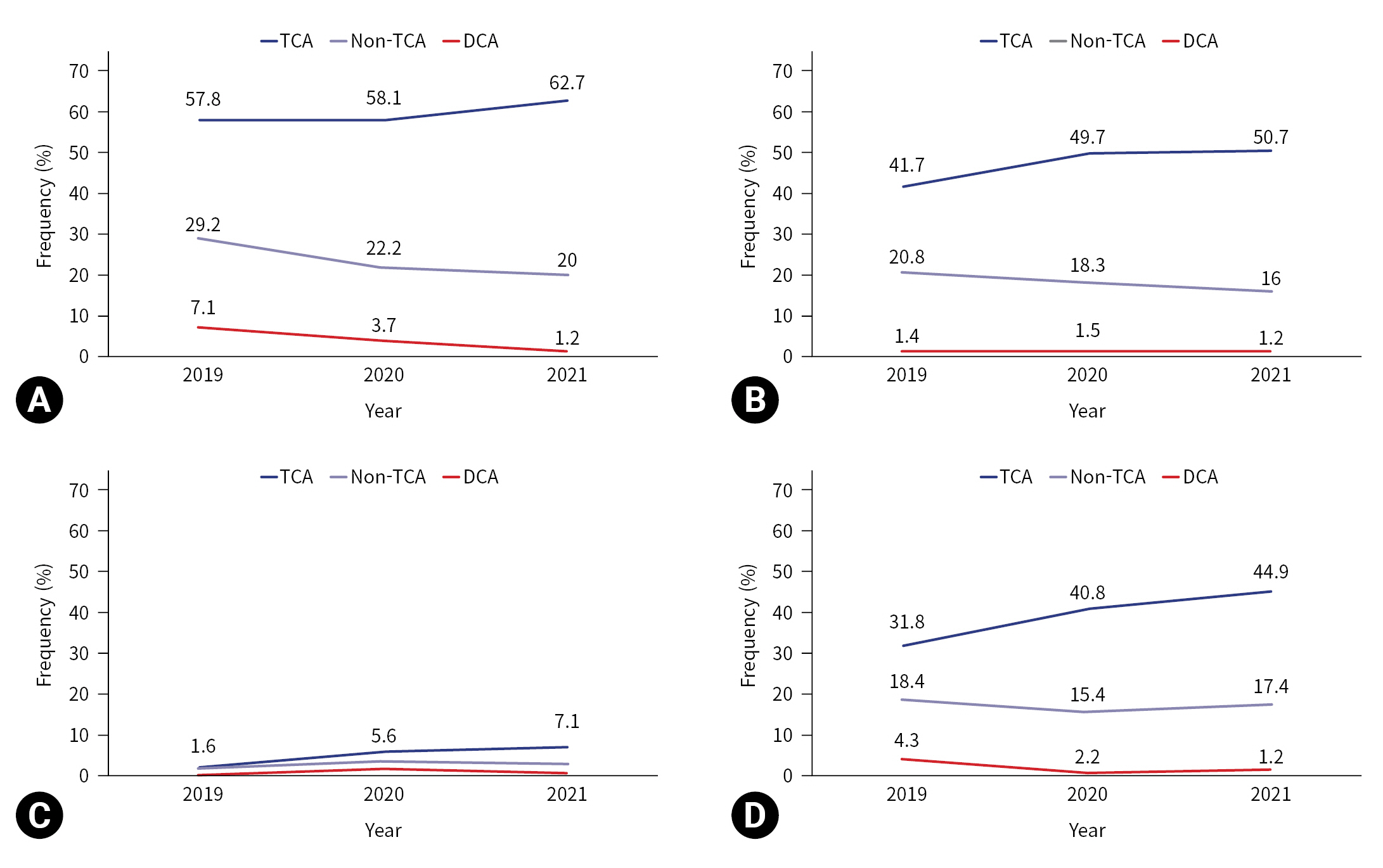
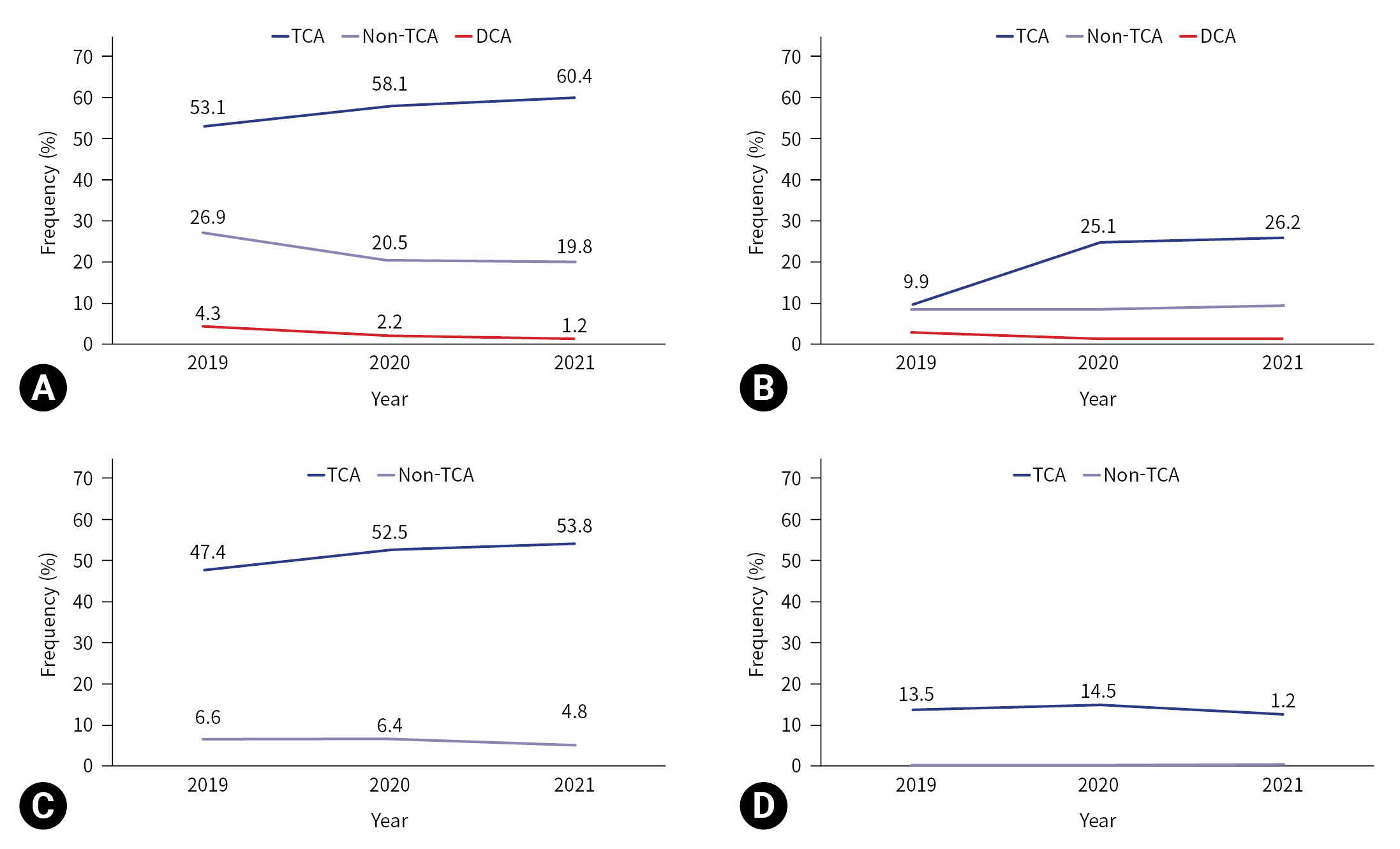
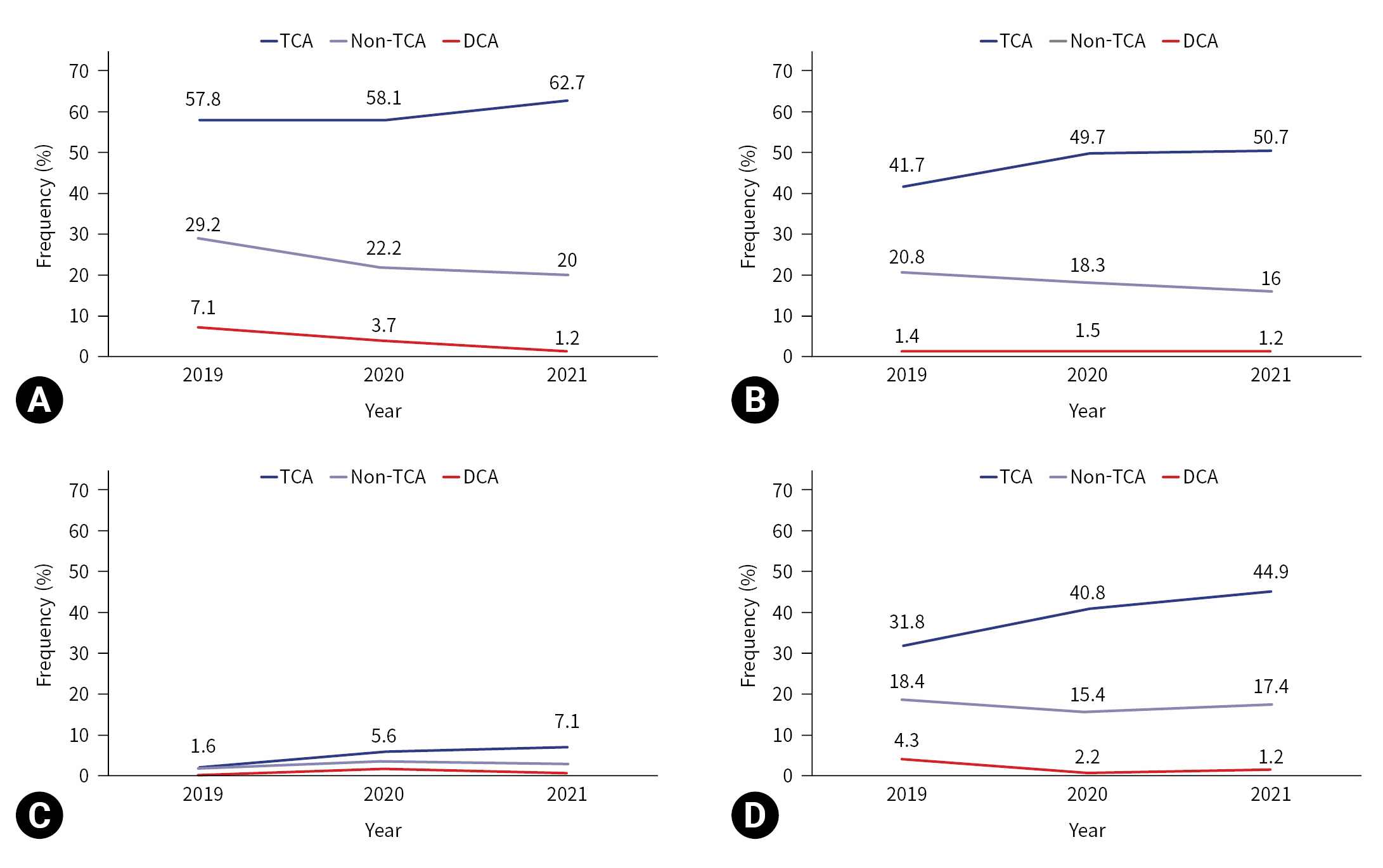
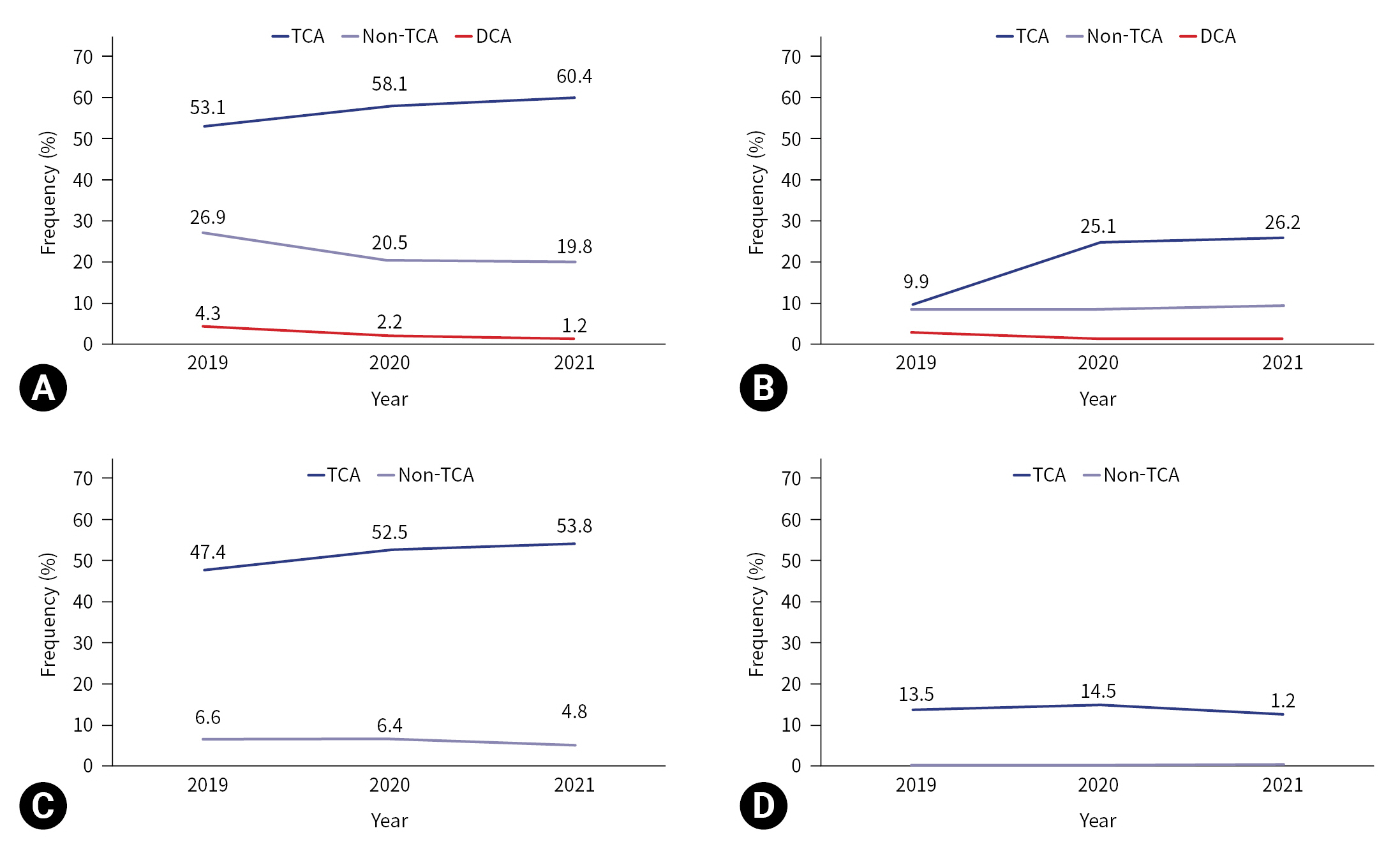
- The prehospital treatments performed during CPR by year are shown in Table 2 and Figs. 2 and 3. In cases of TCA, airway maneuvers were performed in 111 cases (57.8%) in 2019, 104 cases (58.1%) in 2020, and 141 cases (62.7%) in 2021. Whereas, in DCA, airway maneuvers were performed in five cases (7.1%) in 2019, five cases (3.7%) in 2020, and two cases (1.2%) in 2021. An OPA was inserted in 80 TCA cases (41.7%) in 2019, 89 TCA cases (49.7%) in 2020, and 114 TCA cases (50.7%) in 2021, while an OPA was inserted in one DCA case (1.4%) in 2019, two DCA cases (1.5%) in 2020, and two DCA cases (1.2%) in 2021. While ETI was performed in three cases (1.6%) in 2019, 10 cases (5.6%) in 2020, and 16 cases (7.1%) in 2021 in the TCA group; in the DCA group it was performed in 0 cases (0%) in 2019, two cases (1.5%) in 2020, and one case (0.6%) in 2021. I-gel insertion and IV-line establishment increased by year in the TCA group: i-gel insertion was performed in 61 cases (31.8%) in 2019, 73 cases (40.8%) in 2020, and 101 cases (44.9%) in 2021 (P=0.022); and an IV line was established in 19 cases (9.9%) in 2019, 45 cases (25.1%) in 2020, and 59 cases (26.2%) in 2021 (P<0.001). The average rates of prehospital BVM ventilation, neck collar application, and wound dressings did not show statistically significant increases by year.
RESULTS
- Coronavirus spreads through the respiratory tract and is highly contagious. Three years into the COVID-19 pandemic, vaccines and drugs have been developed, and concerns for the severity of COVID-19 have been relatively alleviated by recent data. However, because COVID-19 was a novel infectious disease and we lacked understanding in the early stages of the pandemic, there was a need for caution and careful preparedness. Moreover, it has been reported that the incidence and mortality of out-of-hospital cardiac arrest increased in other countries since the COVID-19 outbreak, and that bystander CPR decreased [7,8]. Because new infectious disease outbreaks are still possible, we will periodically face similar situations. In the hospital, PPE must be worn meticulously when treating patients with infectious diseases, and infection transmission should be minimized with thorough disinfection after treatments. When possible, it is also important to determine whether a patient has COVID-19. However, EMTs in the field must be especially careful because patient information (i.e., infection status) may be limited, and there may be restricted time and space for appropriate PPE, increasing the infection risk. Moreover, in cardiac arrest situations where even a few minutes of delay in starting CPR contributes to a poor prognosis [9,10], infection prevention may be neglected or overlooked due to the narrow window of time for proper treatment as well as the emotional pressure. However, the chest compressions and airway treatments performed during CPR present a high risk for infection transmission, and EMTs should make every effort to wear PPE to prevent the secondary infection of other patients and themselves.
- We excluded patients who experienced cardiac arrest during transport for the following reasons. Usually, a team of two to three EMTs was dispatched to the scene in Gangwon Province, but once transfer was started, one EMT drove the ambulance and the other one or two EMTs were left in the patient care compartment. Optimal treatment in alignment with the guidelines can be difficult due to this decrease in manpower and the confined space. Additional information may also be obtained at this point (e.g., DNR requests from guardians) that changes the characteristics of the initial dispatch for cardiac arrest and influences treatment decisions. Therefore, to confirm that any changes in the initial treatment were related to infection concerns, this study was limited to cases where rescue personnel were dispatched for cardiac arrest from the beginning.
- During the study period, the emergency treatments remained unchanged or increased, including airway procedures during CPR for TCA. In addition, almost all treatments were performed at higher rates in the TCA group than in the DCA group. However, ETI was performed in only 4.9% of cases. ETI is highly dependent on the individual rescuer’s capabilities and training, and it was not often performed in the field due to lack of experience. Instead, an extraglottic airway device such as i-gel was preferred. Although ETI is the recommended airway procedure for patients with a Glasgow Coma Scale <8 in major trauma [11], it has been performed at a significantly low rate. However, there have been reports that advanced airway treatment in the prehospital setting is neither beneficial nor harmful, so it remains inconclusive whether advanced airway treatments should be performed more frequently in the field [12–14]. Other studies have also demonstrated that prehospital airway management using extraglottic airways was not inferior to endotracheal intubation and should therefore be considered [15–18].
- Only wound dressings for hemostasis showed a decreasing pattern. This should not be interpreted as a decrease in treatment, however, because the need for hemostasis is determined by external bleeding or wounds. Moreover, because the management of hemostasis is less likely to contribute to the transmission of respiratory tract infections than airway treatments, it was not considered significant in this study.
- Interestingly, all treatments differed significantly between the DCA group and the TCA group. In fact, EMTs are advised to minimize on-scene time and to transfer patients with major trauma quickly, preferably within 10 minutes after rescue. However, in non-TCA events, where EMTs may be allowed to stay on-scene for longer periods and provide advanced life support under medical oversight, we found that on-scene treatment was lower than in the TCA group.
- In light of studies reporting that several cases of severe acute respiratory syndrome (SARS) and severe fever with thrombocytopenia syndrome had spread to medical personnel during CPR [19,20], it was suspected that CPR and airway treatments would decrease in the field after the COVID-19 outbreak. However, statistically significant decreases were found only with airway maneuvers and BVM in the non-TCA group, and no differences and/or increases were found in other treatments in the trauma group. For TCA at least, it was confirmed that on-scene treatments did not decrease due to the influence of COVID-19.
- There are possible reasons for this finding. First, EMTs may have been less likely to consider the possibility of COVID-19 infection in the trauma group since the signs and symptoms of COVID-19 (e.g., dyspnea or pneumonia) were more likely in the disease group. After the COVID-19 outbreak, ETI and i-gel insertion had statistically significant increases in the TCA group and appeared unaffected by COVID-19. Another possible reason was that the patients with TCA were somewhat younger than those with DCA (55.9±18.4 years vs. 68.5±18.3 years, P<0.001), and that more effort was made to revive younger patients with relatively fewer underlying diseases. Furthermore, this may have been due to the emphasis in EMS education on the importance of treatment in major trauma and might have reflected the hiring of new EMTs with recent hospital-based clinical experiences.
- Limitations
- This study had some limitations. First, because this work was based on the EMS run sheets, in some cases the cause of cardiac arrest was not clear. The recorded cause of the cardiac arrest was based on descriptions by witnesses at the scene, and by the patient's condition and situation at the time of discovery. Therefore, the true etiology was not always clear. However, since EMTs often provide treatment based on the limited information available to them at the scene, it is appropriate to assume that the responses of the EMTs in this study were typical. Second, the data were collected from only one province and may not be generalizable to the entire country. Regional differences may exist, as exemplified by the fact that Gangwon Province is a large area that accounts for 20.5% of the country but has the lowest proportion (35.5%) of level I EMTs and nurses in the country (Seoul, 50.2%; Busan, 60.2%; Gwangju, 90.7%; Gyeonggi Province, 91.2%; national average, 65.7%). Certain skills are limited to level I EMTs and nurses in rescue situations, and a study of national data may show different results. Further study is needed to clarify the exact reasons for any changes in the treatment of TCA.
- Conclusions
- Our comparison of the prehospital EMS treatments provided to patients with TCA before the COVID-19 outbreak, to those provided during the COVID-19 outbreak showed that treatments did not decrease. In fact, endotracheal intubation, I-Gel insertion, and IV-line establishment increased.
DISCUSSION
-
Author contributions
Conceptualization: HIK; Data curation: HIK; Formal analysis: all authors; Methodology: HIK; Writing–original draft: all authors; Writing–review and editing: HIK. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data of this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION
- 1. Barnard EB, Sandbach DD, Nicholls TL, Wilson AW, Ercole A. Prehospital determinants of successful resuscitation after traumatic and non-traumatic out-of-hospital cardiac arrest. Emerg Med J 2019;36:333–9. ArticlePubMed
- 2. Escutnaire J, Genin M, Babykina E, et al. Traumatic cardiac arrest is associated with lower survival rate vs. medical cardiac arrest: results from the French national registry. Resuscitation 2018;131:48–54. ArticlePubMed
- 3. Smith JE, Rickard A, Wise D. Traumatic cardiac arrest. J R Soc Med 2015;108:11–6. ArticlePubMedPMCPDF
- 4. National Fire Agency. The standard protocols for 119 emergency medical services providers. National Fire Agency of Korea; 2019.
- 5. Kim JY, Choe PG, Oh Y, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci 2020;35:e61. ArticlePubMedPMCPDF
- 6. Korea Disease Control and Prevention Agency. COVID-19: occurrence trend of COVID-19 in Korea [Internet]. Ministry of Health and Welfare of Korea [cited 2023 Feb 23]. Available from: https://ncov.kdca.go.kr/.
- 7. Marijon E, Karam N, Jost D, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health 2020;5:e437–43. ArticlePubMedPMC
- 8. Baldi E, Sechi GM, Mare C, et al. Out-of-hospital cardiac arrest during the COVID-19 outbreak in Italy. N Engl J Med 2020;383:496–8. ArticlePubMed
- 9. Holmberg M, Holmberg S, Herlitz J. Incidence, duration and survival of ventricular fibrillation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation 2000;44:7–17. ArticlePubMed
- 10. Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med 1993;22:1652–8. ArticlePubMed
- 11. American College of Surgeons. ATLS: Advanced Trauma Life Support: student course manual. 10th ed. American College of Surgeons; 2018.
- 12. Nishimura T, Suga M, Nakao A, Ishihara S, Naito H. Prehospital advanced airway management of emergency medical service-witnessed traumatic out-of-hospital cardiac arrest patients: analysis of nationwide trauma registry. Acute Med Surg 2022;9:e786PubMedPMC
- 13. Tanabe S, Ogawa T, Akahane M, et al. Comparison of neurological outcome between tracheal intubation and supraglottic airway device insertion of out-of-hospital cardiac arrest patients: a nationwide, population-based, observational study. J Emerg Med 2013;44:389–97. ArticlePubMed
- 14. Hasegawa K, Hiraide A, Chang Y, Brown DF. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA 2013;309:257–66. ArticlePubMed
- 15. Benger JR, Kirby K, Black S, et al. Supraglottic airway device versus tracheal intubation in the initial airway management of out-of-hospital cardiac arrest: the AIRWAYS-2 cluster RCT. Health Technol Assess 2022;26:1–158. ArticlePDF
- 16. Carney N, Totten AM, Cheney T, et al. Prehospital airway management: a systematic review. Prehosp Emerg Care 2022;26:716–27. ArticlePubMed
- 17. Park MJ, Kwon WY, Kim K, et al. Prehospital supraglottic airway was associated with good neurologic outcome in cardiac arrest victims especially those who received prolonged cardiopulmonary resuscitation. Acad Emerg Med 2017;24:1464–73. ArticlePubMedPDF
- 18. Schauer SG, Naylor JF, Chow AL, et al. Survival of casualties undergoing prehospital supraglottic airway placement versus cricothyrotomy. J Spec Oper Med 2019;19:86–9. ArticlePubMed
- 19. Christian MD, Loutfy M, McDonald LC, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis 2004;10:287–93. ArticlePubMedPMC
- 20. Kim WY, Choi W, Park SW, et al. Nosocomial transmission of severe fever with thrombocytopenia syndrome in Korea. Clin Infect Dis 2015;60:1681–3. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite