Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Case Report
Isolated penetrating gluteal stab injury with uncontrolled bleeding in Türkiye: a case report -
Ali Metehan Celep, MD
 , Görkem Yiğit, MD
, Görkem Yiğit, MD , Ayla Ece Çelikten, MD
, Ayla Ece Çelikten, MD , Kudret Atakan Tekin, MD
, Kudret Atakan Tekin, MD , Ufuk Türkmen, MD
, Ufuk Türkmen, MD
-
Journal of Trauma and Injury 2023;36(4):454-457.
DOI: https://doi.org/10.20408/jti.2023.0010
Published online: August 8, 2023
- 687 Views
- 19 Download
Department of Cardiovascular Surgery, Hitit University Erol Olçok Education and Research Hospital, Çorum, Türkiye
- Correspondence to Görkem Yiğit, MD. Department of Cardiovascular Surgery, Hitit University Erol Olçok Education and Research Hospital, Çepni Mahallesi İnönü Caddesi No:176, Çorum 19040, Türkiye Tel: +90-506-677-75-77 Email: drgorkemyigit@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Arterial injuries in the gluteal region caused by a knife are rare but serious, with mortality rates of up to 25%. This case report presents the management of a young male patient admitted to the emergency department in hypovolemic shock, with uncontrollable bleeding from an isolated penetrating gluteal injury. Additionally, the details of the surgical approach employed are discussed.
- Penetrating gluteal stab injuries represent a major emergency that is infrequently encountered yet can present serious diagnostic and therapeutic challenges in emergency departments and trauma centers [1,2]. These injuries may be associated with life-threatening conditions, including visceral, vascular, neurological, inferior and/or superior gluteal artery, iliac artery, sciatic nerve, urethral, rectal, and spinal cord injuries. In cases with delayed treatment, pseudo-aneurysms may develop. A mortality risk of up to 25% is observed for serious injuries [3]. When devising a treatment strategy, it is essential to tailor interventional and surgical approaches to patients.
- The objective of this study was to emphasize the importance of selecting the optimal surgical approach for achieving the best clinical outcomes in the treatment of such injuries. Accordingly, we share our experience with a young male patient who presented to the emergency department with uncontrollable bleeding following an isolated penetrating gluteal injury.
INTRODUCTION
- A 31-year-old man was admitted to the emergency department with massive blood loss and shock after a stab wound to the buttock. At admission, he was conscious but provided vague responses to questions and reported a loss of sensation in his penis. His vital signs included blood pressure of 60/40 mmHg, respiratory rate of 20 breaths/min with shallow respiration, oxygen saturation of 88%, heart rate of 135 beats/min, and body temperature of 36 °C. While in the supine position, the patient’s abdomen appeared normal, with no tenderness or palpable masses detected. The patient’s skin was cold and moist. When he was placed in the prone position and the pressure dressing was removed, a 3×5-cm stab wound was observed in the left gluteal region, with active massive bleeding from this incision. Manual examination confirmed peripheral pulses in both lower extremities, and neurological examination revealed no motor or sensory deficits.
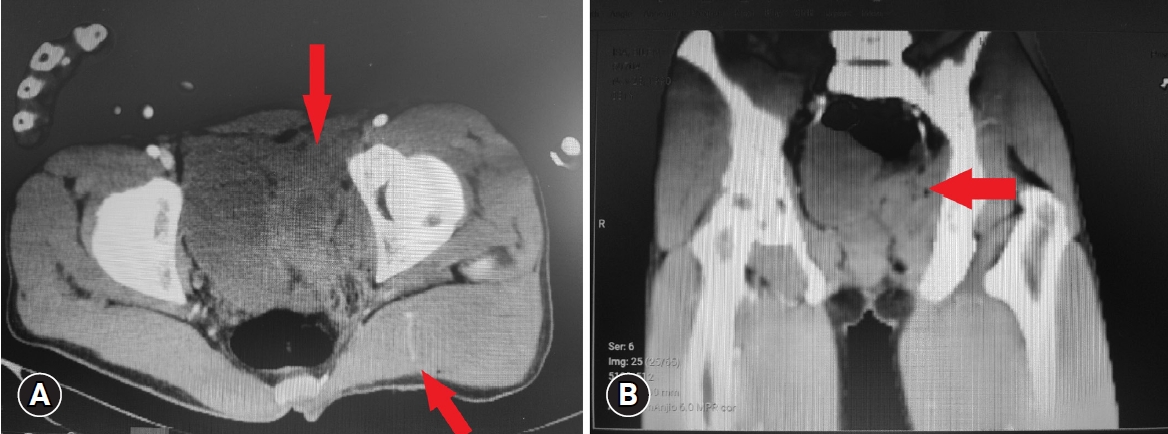
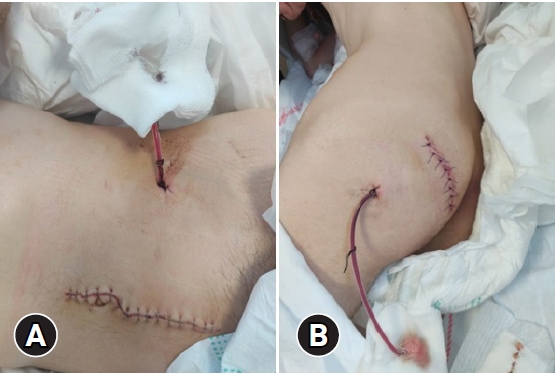
- A full suite of abdominal, pelvic, and lower extremity computed tomographic angiography (CTA) examinations were conducted to assess additional organ injury and detect arterial pathology. Intravenous Ringer lactate infusion and tetanus prophylaxis were administered as medication, and a transfusion of 2 units of erythrocyte suspension was initiated. The blood and blood products necessary for the operation were urgently prepared. CTA images were promptly evaluated in collaboration with urology, general surgery, orthopedics, and emergency medicine specialists. No pathologies, such as intra-abdominal organ perforation, rectal perforation, or ureter injury, were observed. Additionally, no free fluid or intraperitoneal air was noted in the abdomen. However, active contrast extravasation from the superior gluteal artery (SGA) branch of the internal iliac artery was detected along with pelvic hematoma (Fig. 1). Due to further deterioration of the patient’s hemodynamics and the development of deep shock, an emergency diagnostic laparotomy, rather than an interventional procedure, was performed by our team in the emergency department operating room. Following mini median laparotomy under general anesthesia, the left common iliac artery, external iliac artery, and internal iliac artery were identified and secured with slings. The ureter was suspended, and no defects were observed. Only left internal iliac artery ligation was performed (Fig. 2). No retroperitoneal bleeding was noted. The concurrent urology team evacuated the pelvic hematoma. A drain was placed, and the laparotomy incisions were closed. The patient was then placed in the prone position; by this point, his bleeding had decreased dramatically (Fig. 2). Upon expansion of the gluteal incision, a reduced amount of active bleeding was observed from the SGA and its branches. The incision was 10 cm deep. Associated bleeding was stopped with simple sutures and clips. After ensuring that all bleeding was under control, the wound area was washed with 3,000 mL of isotonic solution and 500 mg of rifocin. Drains were placed in the wound areas (Fig. 3).
- The patient was monitored in the intensive care unit, where broad-spectrum antibiotics were administered along with colloid and crystalloid fluid replacements. Four hours after surgery, and with all hemodynamic parameters under evaluation, he was extubated. On the 1st postoperative day, we observed no signs of bleeding or additional complications. Hemodynamic and laboratory parameters were normal. On the 2nd postoperative day, the patient was mobilized. By that time, dramatic improvement was observable, eliminating the need for blood products. The patient did not experience any penile numbness or erectile dysfunction. With no further issues at inpatient follow-ups, the patient was discharged on the sixth postoperative day. During the 1st month of outpatient follow-up, CTA revealed that the pelvic hematoma had been resorbed and no active bleeding focus was evident. At the 6-month follow-up, the patient exhibited no motor deficits, urinary incontinence, or erectile dysfunction, and he was able to resume his normal life.
- Ethics statement
- Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
CASE REPORT
- Penetrating gluteal injuries account for 2% to 3% of all penetrating injuries seen in emergency services admissions [4,5]. Presently, the literature indicates a mortality risk of up to 4% for any gluteal penetrating injury based on studies conducted at trauma centers [5]. Moreover, short- and long-term morbidity in patients with penetrating gluteal trauma can range from 0% to 33% [5]. In fact, our patient presented to the emergency department in shock, and his overall condition was critical.
- The structures most commonly damaged following a penetrating hip injury include the SGA, rectum, small intestine, and colon. Injuries to the iliac artery and/or vein are diagnosed less frequently, and sciatic or lumbosacral nerve injuries are extremely rare. All patients with isolated penetrating injuries should undergo surgery at experienced centers. In the present case, the successful management of a young patient with an isolated penetrating gluteal artery injury, in collaboration with experienced urology and general surgery specialists, directly contributed to survival. Delays and errors in diagnosing and treating such cases may, unfortunately, contribute to mortality.
- Bleeding from damaged vessels, gluteal aneurysm or pseudoaneurysm, gluteal compartment syndrome, perirectal hematoma, injuries to the rectum or small intestine, long-term ileus or temporary obstruction, soft tissue or urinary tract infections, sciatic nerve or lumbosacral plexus injury, impotence, and pressure sores are the most common complications of similar injuries. However, our case involved only an isolated artery injury, avoiding potential morbidities that can arise from additional pathologies.
- When a patient presents to the emergency room exhibiting signs of hemodynamic instability, hypovolemic shock, and acute internal bleeding, resuscitation and emergency intervention may be necessary [6]. The SGA is more commonly injured in penetrating trauma, while the inferior gluteal artery is more frequently affected by blunt trauma. In patients with hemodynamically unstable gluteal region injuries, it is crucial to promptly investigate intra-abdominal and intrapelvic organ injuries as well as intrapelvic vessel damage. Rapid implementation of diagnostic methods and concurrent consultation with relevant specialists can be lifesaving. CTA is a leading rapid diagnostic technique and was the method of choice for the patient in this case, who presented with shock. A multidisciplinary approach led to the decision for a median laparotomy and left internal iliac artery ligation, which was made approximately 15 minutes after the patient’s arrival at the emergency department. While methods such as interventional angiography and coil embolization of the affected vessels may be suitable for some patients, the hemodynamic situation and clinical presentation led us to the decision of open surgery in this case. In similar patients presenting with shock, an exploratory laparotomy may be required after pressure packing is placed in the wound; alternatively, it may be necessary to ligate the internal iliac artery or its branches using an extraperitoneal approach to control ongoing external hemorrhage [7]. The vital role of vascular surgeons in this process cannot be overstated.
- Penetrating gluteal injuries are potentially fatal wounds. Most patients who are hemodynamically stable can benefit from standard wound care and selective nonsurgical treatment. However, when a gluteal artery injury is confirmed or suspected, early CTA examination provides the most accurate diagnosis. For patients experiencing hypovolemic shock and exhibiting signs of internal bleeding, immediate lifesaving open surgery is the gold-standard treatment option. Penetrating injuries to the buttocks are serious pathologies that must be regarded as potentially life-threatening and should be managed with a multidisciplinary approach in trauma centers.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
-
Author contributions
Conceptualization: AMC, GY; Data curation: AEÇ, UT; Formal analysis: AEÇ, KAT, UT; Visualization: GY; Writing–original draft: AMC, GY; Writing–review & editing: all authors. All authors read and approved the final manuscript.
ARTICLE INFORMATION

- 1. Makrin V, Sorene ED, Soffer D, Weinbroum A, Oron D, Kluger Y. Stab wounds to the gluteal region: a management strategy. J Trauma 2001;50:707–10. ArticlePubMed
- 2. Mercer DW, Buckman RF Jr, Sood R, Kerr TM, Gelman J. Anatomic considerations in penetrating gluteal wounds. Arch Surg 1992;127:407–10. ArticlePubMed
- 3. Gilroy D, Saadia R, Hide G, Demetriades D. Penetrating injury to the gluteal region. J Trauma 1992;32:294–7. ArticlePubMed
- 4. Lesperance K, Martin MJ, Beekley AC, Steele SR. The significance of penetrating gluteal injuries: an analysis of the Operation Iraqi Freedom experience. J Surg Educ 2008;65:61–6. ArticlePubMed
- 5. Susmallian S, Ezri T, Elis M, Dayan K, Charuzi I, Muggia-Sullam M. Gluteal stab wound is a frequent and potentially dangerous injury. Injury 2005;36:148–50. ArticlePubMed
- 6. Salim A, Velmahos GC. When to operate on abdominal gunshot wounds. Scand J Surg 2002;91:62–6. ArticlePubMedPDF
- 7. Rasmussen TE. Commentary on “Isolated penetrating gluteal injuries: a potentially life-threatening trauma”. Perspect Vasc Surg Endovasc Ther 2009;21:257–8. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Blunt abdominal trauma resulting in pancreatic injury in a pediatric patient in Australia: a case report
- Penetrating gallbladder injury in a pediatric patient: a case report
- Endovascular treatment of traumatic iliac venous injury combined with phlegmasia cerulea dolens in Korea: a case report
- Penetrating liver injury caused by a metal fragment from a blast accident in a factory: a case report
- Endovascular treatment of penetrating nail gun injury of the cervical spine and vertebral artery: a case report
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite




