Articles
- Page Path
- HOME > J Korean Soc Traumatol > Early view > Article
-
Case Report
An unstable patient with a large sucking chest wound managed with gauze packing for preventing tension and bleeding control before surgery in Korea: a case report -
Chang-Sin Lee, MD
 , Min-Jeong Cho, MD
, Min-Jeong Cho, MD , Tae-Wook Noh, MD
, Tae-Wook Noh, MD , Nak-Jun Choi, MD
, Nak-Jun Choi, MD , Jun-Min Cho, MD
, Jun-Min Cho, MD
-
DOI: https://doi.org/10.20408/jti.2023.0066
Published online: February 23, 2024
- 338 Views
- 7 Download
Department of Acute Care Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- Correspondence to Chang-Sin Lee, MD Department of Acute Care Surgery, Korea University Guro Hospital, Guro Hospital, Korea University College of Medicine, 148 Gurodong-ro, Guro-gu, Seoul 08308, Korea Tel: +82-2-2626-1114 Email: viano0420@naver.com
© 2024 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- This case report describes the management of a 51-year-old female patient who arrived at the emergency room with a stab wound to the upper right chest. Immediate medical interventions were undertaken, including blood transfusions and endotracheal intubation. To prevent tension and control bleeding, gauze packing was applied directly through the large open wound. Further surgical exploration identified a laceration in the lung, necessitating a right upper lobe resection. Postoperatively, the patient's vital signs stabilized, and she was subsequently discharged without complications. This case highlights the decision-making process in selecting between an emergency department thoracotomy and an operating room thoracotomy for patients with penetrating chest trauma. It also illustrates the role of gauze packing in managing tension and hemorrhage. In summary, gauze packing can be an effective interim measure for stabilizing patients with traumatic injuries, unstable vital signs, and large open chest wounds, particularly when a chest tube is already in place, to prevent tension and facilitate bleeding control prior to surgical intervention.
- Chest trauma is associated with a significant mortality rate, which ranges from 25% to 50% across all age groups. Although the majority of patients with chest trauma respond well to volume resuscitation and respiratory support, approximately 10% to 15% require surgical intervention. Surgical intervention in cases of chest trauma is indicated for patients with hemorrhage exceeding 1.5 L, significant impairment of mechanical ventilation, injury to the tracheobronchial tree, and injuries to the heart or large vessels that result in blood loss or peripheral tamponade. The decision between performing an emergency department thoracotomy (EDT) and a thoracotomy in the operating room is a critical one, with various strategies being applied in the management of such cases. This choice continues to be a topic of debate regarding clinical decision-making [1,2].
- This case report describes the complex clinical management of a 51-year-old female patient who presented to the emergency room with a stab wound to the upper right chest. The patient's initial hemodynamic instability necessitated immediate medical interventions, including blood transfusions and endotracheal intubation. The decision-making process regarding the choice of surgical intervention and whether to perform an EDT or a thoracotomy in the operating room played a pivotal role in the patient's subsequent clinical course.
- Furthermore, this report discusses the use of gauze packing as part of the bleeding control strategy and as a way to prevent tension. Through this case, we aim to share insights into the decision-making process and clinical considerations when managing penetrating chest trauma, with particular attention to the judicious application of gauze packing as a potentially effective method for managing bleeding and preventing tension .
INTRODUCTION
- A 51-year-old woman presented to the emergency room with a stab wound to the upper right chest (Fig. 1). The wound, which had been inflicted by a knife, was covered with gauze and the patient was transported by emergency medical services. On arrival, her heart rate was 101 beats/min and her systolic blood pressure was 40 mmHg. A HemoCath catheter (12F, HemoCath Ltd) was immediately inserted into the right femoral vein, and she received 500 mL of crystalloid solution and 2 U of universal-type red blood cells (RBCs) via a rapid infusion system. An arterial line and a chest tube were then placed. The initial drainage from the chest tube was 980 mL, and a significant hematoma was noted on a subsequent chest x-ray. Endotracheal intubation was performed, during which a considerable amount of hematoma was evacuated from the stab wound. Post-intubation arterial blood gas analysis revealed severe metabolic acidosis with a pH of 7.20, a CO2 level of 31 mmHg, an O2 level of 321 mmHg, an HCO3– level of 12.1 mEq/L, a hemoglobin level of 9.4 g/dL, and a lactic acid level of 9.7 mmol/L. The patient went into cardiac arrest while being transferred to the operating room, 54 minutes after her arrival at the emergency room. By that time, a total of 2 L of hemothorax had been drained via the chest tube, and she had received 15 U of RBCs, 15 U of fresh frozen plasma, and 6 U of cryoprecipitate. After 6 minutes of cardiopulmonary resuscitation, spontaneous circulation was successfully restored. Before another attempt to transfer her to the operating room, a bedside wound exploration was performed, during which gauze packing was used. This led to the decision to use 30 x-ray-detectable gauze pieces, each measuring 10 cm×10 cm, as part of the strategy to control bleeding (Fig. 2). The patient was then taken to the operating room, and just before the induction of anesthesia, her systolic blood pressure had increased to 110 mmHg without the need for vasopressors. Surgery commenced 75 minutes after her initial hospital admission.
- In the operating room, removal of the gauze packing exposed a laceration with active bleeding in the right upper lobe. An approximately 10-cm laceration and disruption were identified on the upper lobe of the lung. There was no damage to the bronchus or hilum; however, bleeding continued within the lung parenchyma. Primary repair proved inadequate for hemostasis, necessitating a right upper lobe resection.
- The patient's vital signs remained stable after the surgery. Vasopressor support was discontinued on postoperative day (POD) 2. Extubation was successfully performed on POD 3, and by POD 7, the patient had been transferred to a general ward. On POD 16, the patient underwent tenorrhaphy to repair a finger laceration. She was ultimately discharged on POD 20.
- Ethics statement
- The patient provided written informed consent for publication of the research details and clinical images.
CASE REPORT
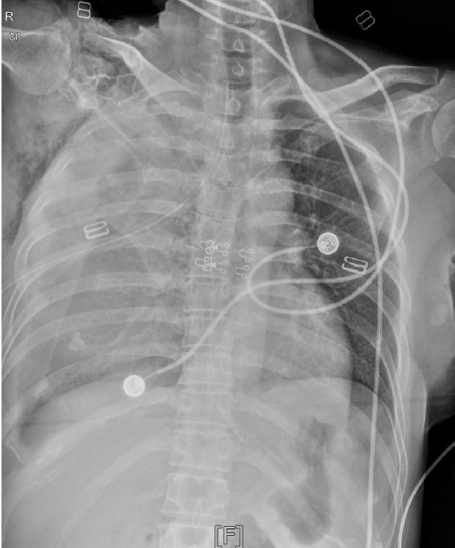
- The patient was successfully discharged after surgery, but several important aspects of the treatment process warrant discussion. First, we discuss the choice between an EDT and a thoracotomy performed in the operating room. This surgical intervention can take place at various stages of the resuscitation process, depending on the patient's physiological status. In this context, three critical issues regarding EDT need to be addressed: (1) why it should be performed; (2) where it should be performed; and (3) when it is appropriate to perform it [1]. The potential causes of the patient's cardiac arrest include tension pneumothorax, tension hemothorax, and hypovolemic shock. Despite the large open wound being successfully sealed and effective drainage through the chest tube, the chest x-ray (Fig. 3) revealed an additional 1 L of hemothorax had been drained. Moreover, the onset of cardiac arrest 40 minutes after arrival suggests that hypovolemic shock due to bleeding, rather than tension hemothorax, was the most likely cause. Consequently, the primary goal of EDT in this patient would be to control bleeding in the right upper lobe. Given the damage to the right upper lobe, hilar control—either through a pulmonary hilar clamp or a pulmonary hilar twist—may have been necessary if EDT was undertaken. This would be likely to lead to a clamshell thoracotomy eventually. According to Simms et al. [3], the clamshell incision is the superior approach for definitive access and control of thoracic structures during EDT.
- However, the mortality rates for patients undergoing EDT have been reported to be as high as 94% in cases of hypovolemic shock and 33% in patients with cardiac tamponade [4]. This marked disparity in mortality rates between EDT for tamponade and EDT for hemorrhage control highlights the critical importance of reevaluating surgical goals prior to intervention, emphasizing the necessity for well-defined surgical objectives in these scenarios.
- In this case, a thorough assessment of the risks and benefits associated with performing bleeding control through a lobectomy via clamshell incision in EDT was conducted. Ultimately, the decision to opt for an operating room thoracotomy as the preferred approach was made, considering various factors such as the patient's condition and the complexity of the procedure in an emergency room setting.
- Fortunately, this patient underwent surgery just 75 minutes after arriving at the emergency room and was successfully discharged. However, it is generally recommended that patients with penetrating injuries who have lost vital signs for no more than 15 minutes undergo resuscitative thoracotomy [5].
- The second point concerns the management of large open, sucking chest wounds. In the case of this patient, a three-sided occlusive dressing was not used to prevent tension pneumothorax due to the open wound. Instead, the wound was sealed with gauze, and a chest tube was inserted. According to the Tactical Combat Casualty Care Guidelines [6], a three-sided occlusive dressing is recommended to prevent tension pneumothorax in the event of a penetrating chest wound. However, the effectiveness of this method has been consistently questioned. The decision to use a wound-sealing dressing instead of a three-sided occlusive dressing was influenced by the clavicle's contour, which created negative pressure and interfered with the dressing's application. Furthermore, the open wound was bleeding profusely, which compromised the adhesive capability necessary for a three-sided occlusive dressing. Consequently, gauze packing was performed within the chest cavity before sealing the wound, and chest tube drainage was successfully carried out without complications. Therefore, it is unlikely that the gauze packing increased the risk of tension pneumothorax, although it may have caused a slight increase in intrathoracic pressure.
- The third point relates to the risks and benefits of gauze packing. Gauze packing provides the benefit of applying direct pressure to control bleeding. However, there is concern about the potential for increased pressure in the pleural space, which could lead to thoracic compartment syndrome. Despite these concerns, studies on thorax damage control surgery have shown that complications such as cardiac tamponade, decreased venous return, and reduced cardiac output are relatively rare, occurring in only about 2.3% of cases when chest pressure is elevated [7]. Additionally, the incidence of other complications, including acute renal failure, bacteremia, pneumonia, and adult respiratory distress syndrome, did not show a significant increase [8]. In the present case, the patient experienced no complications from gauze packing, including cardiac tamponade. The gauze packing allowed the patient to remain stable until she could be transferred to the operating room without any further complications.
- In conclusion, when managing trauma in patients who present with unstable vital signs and a significant sucking chest wound, where a chest tube has already been inserted, it is feasible to attempt gauze packing. This intervention serves not only to prevent tension, but also to control bleeding prior to surgical intervention.
DISCUSSION
-
Author contributions
Conceptualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION
- 1. Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma: a review. Injury 2006;37:1–19. ArticlePubMed
- 2. ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS): the ninth edition. J Trauma Acute Care Surg 2013;74:1363–6.
- 3. Simms ER, Flaris AN, Franchino X, Thomas MS, Caillot JL, Voiglio EJ. Bilateral anterior thoracotomy (clamshell incision) is the ideal emergency thoracotomy incision: an anatomic study. World J Surg 2013;37:1277–85. ArticlePubMedPDF
- 4. von Oppell UO, Bautz P, De Groot M. Penetrating thoracic injuries: what we have learnt. Thorac Cardiovasc Surg 2000;48:55–61. ArticlePubMed
- 5. Kirkpatrick AW, Ball CG, D’Amours SK, Zygun D. Acute resuscitation of the unstable adult trauma patient: bedside diagnosis and therapy. Can J Surg 2008;51:57–69. PubMedPMC
- 6. Butler FK Jr, DuBose JJ, Otten EJ, et al. Management of open pneumothorax in tactical combat casualty care: TCCC guidelines change 13-02. J Spec Oper Med 2013;13:81–6. ArticlePubMed
- 7. O’Connor JV, DuBose JJ, Scalea TM. Damage-control thoracic surgery: management and outcomes. J Trauma Acute Care Surg 2014;77:660–5. PubMed
- 8. Lang JL, Gonzalez RP, Aldy KN, et al. Does temporary chest wall closure with or without chest packing improve survival for trauma patients in shock after emergent thoracotomy? J Trauma 2011;70:705–9. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST



 PubReader
PubReader ePub Link
ePub Link Cite
Cite




