Articles
- Page Path
- HOME > J Trauma Inj > Volume 37(1); 2024 > Article
-
Case Report
Treatment of a penetrating inferior vena cava injury using doctor-helicopter emergency medical service and direct-to-operating room resuscitation in Korea: a case report -
Dongmin Seo, MD1,2
 , Jieun Kim, MD1,2
, Jieun Kim, MD1,2 , Jiwon Kim, MD1,2
, Jiwon Kim, MD1,2 , Inhae Heo, MD1,2
, Inhae Heo, MD1,2 , Jonghwan Moon, MD1,2
, Jonghwan Moon, MD1,2 , Kyoungwon Jung, MD1,2
, Kyoungwon Jung, MD1,2 , Hohyung Jung, MD1,2
, Hohyung Jung, MD1,2
-
Journal of Trauma and Injury 2024;37(1):74-78.
DOI: https://doi.org/10.20408/jti.2023.0055
Published online: January 12, 2024
- 795 Views
- 19 Download
1Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
2Regional Trauma Center of Southern Gyeonggi Province, Ajou University School of Medicine, Suwon, Korea
- Correspondence to Hohyung Jung, MD Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, 206 World cup-ro, Yeongtong-gu, Suwon 16499, Korea Tel: +82-31-219-7483 Email: jhh21228@aumc.ac.kr
© 2024 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Inferior vena cava (IVC) injuries can have fatal outcomes and are associated with high mortality rates. Patients with IVC injuries require multiple procedures, including prehospital care, surgical techniques, and postoperative care. We present the case of a 67-year-old woman who stabbed herself in the abdomen with a knife, resulting in an infrarenal IVC injury. We shortened the transfer time by transporting the patient using a helicopter and decided to perform direct-to-operating room resuscitation by a trauma physician in the helicopter. The patient underwent laparotomy with IVC ligation for damage control during the first operation. The second- and third-look operations, including previous suture removal, IVC reconstruction, and IVC thrombectomy, were performed by a trauma surgeon specializing in cardiovascular diseases. The patient was discharged without major complications on the 19th postoperative day with rivaroxaban as an anticoagulant medication. Computed tomography angiography at the outpatient clinic showed that thrombi in the IVC and both iliac veins had been completely removed. Patients with IVC injuries can be effectively treated using a trauma system that includes fast transportation by helicopter, damage control for rapid hemostasis, and expert treatment of IVC injuries.
- The mortality rate from inferior vena cava (IVC) injuries is estimated to be approximately 20% to 66%; more than one-third of patients do not survive to reach a hospital, and another third die within 24 hours of treatment [1]. Despite advances in prehospital care and surgical techniques, the mortality rates associated with penetrating IVC injuries have not improved [2]. Survival after an IVC injury can be predicted by the severity and anatomic accessibility [3]. The suprahepatic segment (100%) has the highest mortality rate, followed by the retrohepatic (78%), juxtarenal (50%), suprarenal (33%), and infrarenal (33%) segments [4]. Patients with IVC injuries require treatment using multiple resources, including blood products, anesthetic care, intensive care units, and appropriate operations. Additionally, these patients require management at a dedicated trauma center that follows early damage control principles [5]. In this case report, we review the role of trauma surgeons in a well-structured trauma system for rapidly treating a patient with an IVC injury using helicopter transportation, appropriate surgical methods, and postoperative care.
INTRODUCTION
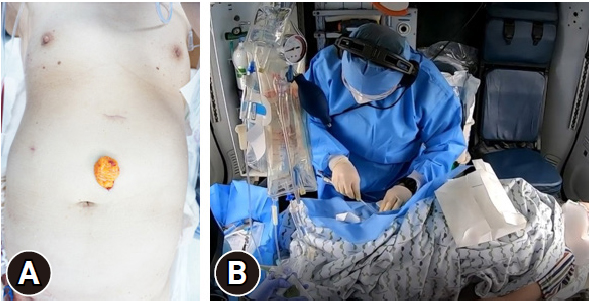
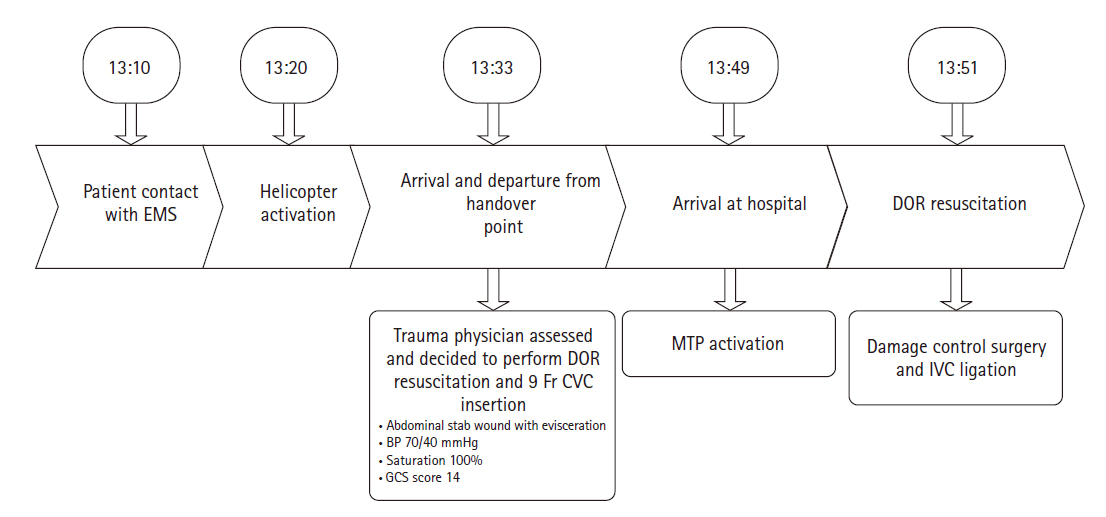
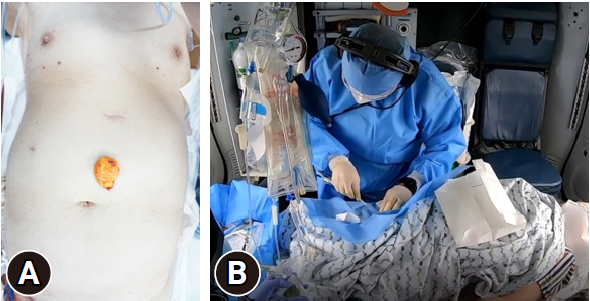
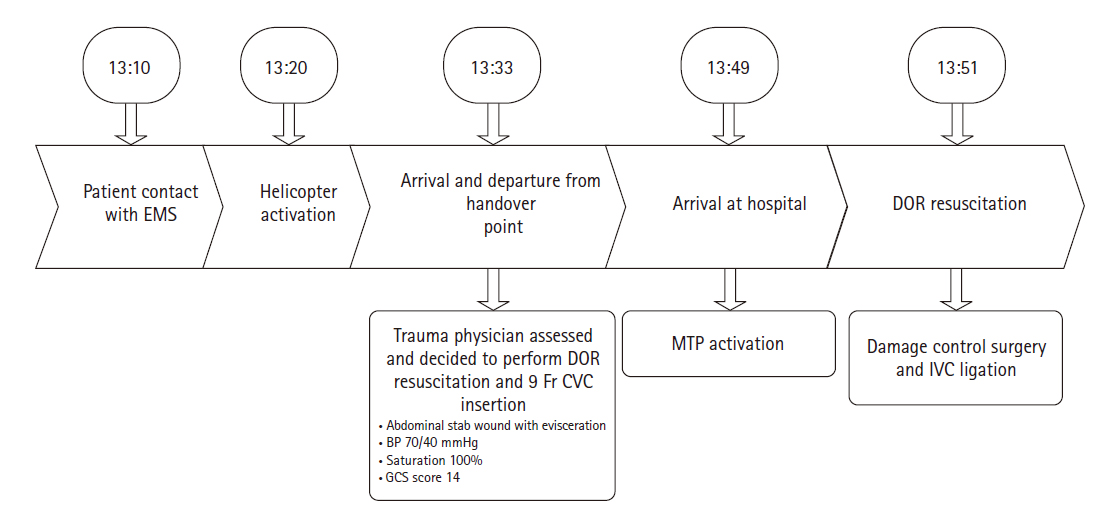
- A 67-year-old woman with depression stabbed herself in the abdomen using a knife. According to the patient information received through emergency medical services, the center of the abdomen was injured, and her systolic blood pressure was 70 mmHg (Fig. 1A). The accident site was approximately 20 km from the hospital and transporting the patient by car would have taken 40 to 50 minutes. Therefore, the patient was transferred using a helicopter to Regional Trauma Center of Southern Gyeonggi Province (Suwon, Korea), and a trauma physician was directly dispatched to the scene in the helicopter. After examining the patient, the trauma physician decided to use direct-to-operating room (DOR) resuscitation and performed femoral vein catheterization in the helicopter (Fig. 1B). Upon arrival, the patient was transported to the operation room and a massive transfusion protocol was activated. Trauma and anesthesiologist teams were on standby in the operating room. The details of the treatments by time are described in Fig. 2.
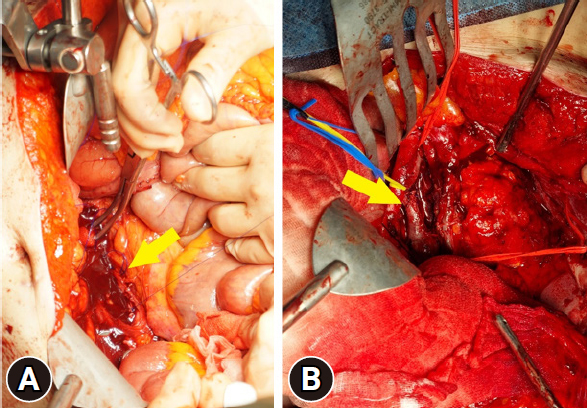
- Laparotomy was performed, and massive hemoperitoneum with a midline inframesocolic retroperitoneal injury was noted. Right-sided medial visceral rotation was performed, and an infrarenal IVC injury was observed. Both the anterior and posterior walls of the IVC were torn, resulting in massive bleeding. Temporary control was achieved by compressing the IVC against the spine, both above and below the injury, using tightly rolled laparotomy pads secured with ringed clamps. We encountered difficulties in executing a simple lateral repair. Due to the patient's risk of exsanguination and poor visibility from the extensive bleeding, we opted to perform a suture ligation using a large needle to create a gross hemostatic stitch (Fig. 3A). Damage to the small-bowel mesentery was also repaired. The estimated blood loss amounted to 6,300 mL. On the same day, the patient received transfusions of 24 U of red blood cells, fresh frozen plasma, 1 U of plateletpheresis, and 10 U of cryoprecipitate. We concluded with a temporary abdominal closure.
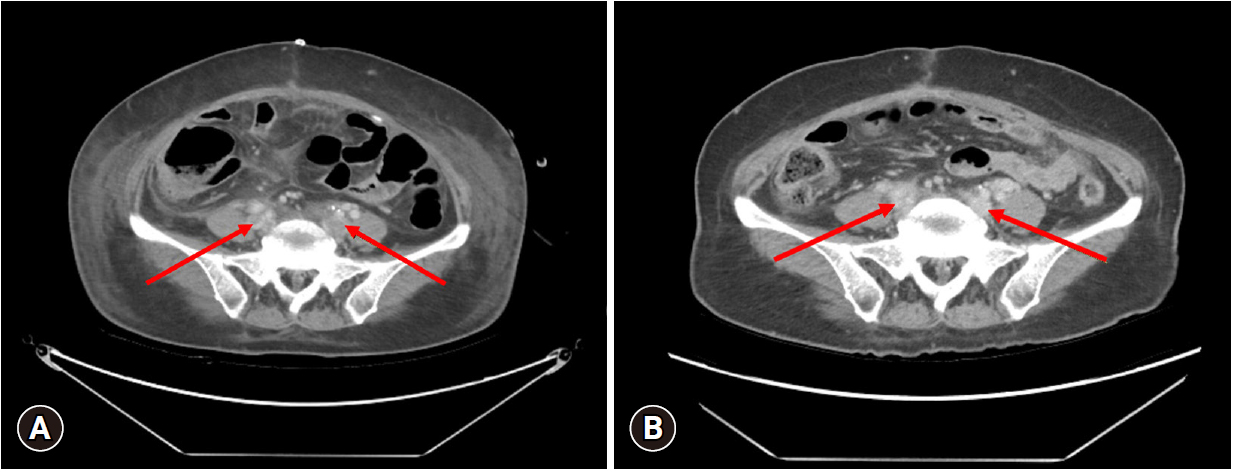
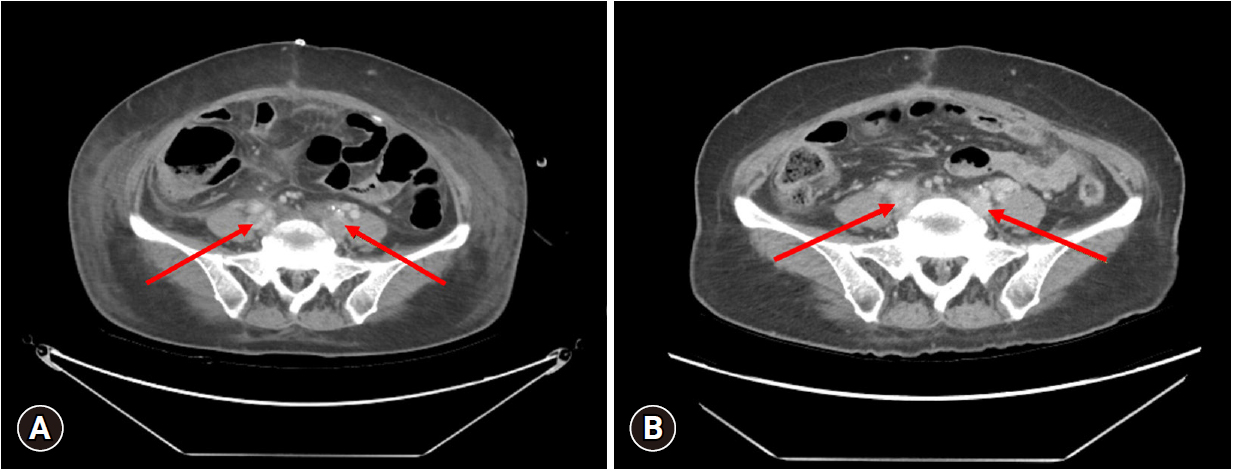
- We conducted a second-look operation the next day. The surgery was performed by a trauma surgeon specializing in cardiovascular diseases. As the IVC was completely occluded; we removed the previous suture and meticulously repaired the IVC. The posterior wall of the IVC was sutured from the inside to the damaged anterior wall. We utilized a Doppler ultrasound to observe the blood flow in the IVC, which appeared to be weak. Consequently, we executed a temporary abdominal closure and identified thrombi in the IVC and both iliac veins using computed tomography angiography (CTA). For our third-look operation, we performed an IVC thrombectomy (Fig. 3B). Ultimately, we closed the abdominal wall. The patient continued her postoperative regimen of rivaroxaban as an anticoagulant. Despite experiencing swelling in both legs and a rectal ulcer with bleeding, she was discharged without significant complications on the 19th postoperative day. A month after discharge, the patient was evaluated at an outpatient clinic. The thrombi in the IVC and both iliac veins were completely removed, as confirmed by CTA (Fig. 4).
- Ethics statement
- This study was reviewed and approved by the Institutional Review Board of Ajou University Hospital and Human Research Protection Center of Ajou University Hospital (No. AJOUIRB-EX-2023-387). The requirement for informed consent was waived, as all data were de-identified to protect the patient’s right to privacy.
CASE REPORT
- The patient was transported by helicopter. The trauma physician’s rapid vascular access and decision to start DOR resuscitation from the moment the patient was boarded onto the helicopter enabled rapid hemostasis. Damage control surgery was initially performed according to the principle of rapid hemostasis. When the patient improved, we collaborated with a cardiovascular trauma surgeon for the second-look surgery, which yielded optimal results.
- Trauma care emphasizes the importance of treating patients promptly. Helicopters have become an alternative for transporting patients when ground transportation is considered less effective or unfeasible. Helicopters offer clear advantages such as faster transport time and a more experienced medical crew [6]. Helicopter transport significantly improves the survival rate of patients with trauma [7].
- Hemorrhage control is time-critical because delays in bleeding control in patients with significant abdominal injuries are associated with high mortality [8]. For patients requiring immediate surgery, the goal of the trauma system is to minimize delays to the operating room and initiate surgical interventions. One of the methods proposed to achieve this goal is DOR resuscitation, which identifies patients requiring surgery and has been found to lead to improved survival [9]. Since the establishment of the regional trauma center in 2016, our center has been implementing the DOR protocol based on the following indications: (1) a penetrating injury accompanied by low blood pressure; (2) a witnessed cardiac arrest; (3) prehospital low blood pressure (i.e., systolic blood pressure below 90 mmHg); (4) uncontrolled major external bleeding (such as from a knee or proximal elbow amputation); and (5) trauma to the neck region that could potentially cause severe airway damage. If the dispatched doctor decides to implement the DOR protocol, this decision must be made at least 5 minutes prior to arrival at the center. The waiting team then prepares blood products in advance to immediately implement mass blood transfusion protocols, and contacts the anesthesiology department to prepare an operating room. During the transfer process, if feasible, vascular access (intraosseous, large-bore peripheral line, preferred multilumen access catheter at the subclavian vein, femoral vein) should be attempted and a blood sample should be obtained before arriving at the hospital.
- However, the surgical management for IVC injuries remains a matter of debate. As primary repair may not always be possible, IVC ligation can be performed simply and quickly. Ligation of the IVC is preferable as part of damage control surgery in critically ill patients. However, a previous study has reported that the incidence of compartment syndrome (odds ratio [OR], 5.23), pneumonia (OR, 1.76), deep venous thrombosis (OR, 2.83), and pulmonary embolism (OR, 3.63) were significantly higher in patients who underwent IVC ligation [10].
- Although few studies have been conducted on the surgical treatment of IVC thrombosis in patients with trauma, several have been conducted on patients with renal cell carcinoma. IVC thrombectomy is a complex procedure that necessitates a multidisciplinary team and skilled surgeons. For patients who have undergone thrombectomy, postoperative anticoagulation therapy is recommended and should be continued for a period of 4 weeks. Those with residual thrombi should receive therapeutic anticoagulation for a duration of 6 months [11].
- Developments in trauma services such as prehospital triage, enhanced hospital procedures, and in-hospital specialized trauma care teams have contributed to the implementation of trauma systems. The management of patients with trauma in a well-established trauma system is associated with decreased mortality [12]. Trauma systems provide an inclusive, integrated structure for providing optimal care to patients with trauma.
- As described in this case report, a critically ill patient with an IVC injury was effectively treated using an advanced trauma system. Fast transport using a helicopter, damage control for rapid hemostasis, and expert treatment for IVC injuries were coordinated proficiently and harmoniously in our trauma system.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Author contributions
Conceptualization: all authors; Methodology: all authors; Investigation: all authors; Writing–original draft: DS; Writing–review & editing: HJ. All authors read and approved the final manuscript.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION
- 1. Navsaria PH, de Bruyn P, Nicol AJ. Penetrating abdominal vena cava injuries. Eur J Vasc Endovasc Surg 2005;30:499–503. ArticlePubMed
- 2. Branco BC, Musonza T, Long MA, et al. Survival trends after inferior vena cava and aortic injuries in the United States. J Vasc Surg 2018;68:1880–8. ArticlePubMed
- 3. Kuehne J, Frankhouse J, Modrall G, et al. Determinants of survival after inferior vena cava trauma. Am Surg 1999;65:976–81. ArticlePubMedPDF
- 4. Rosengart MR, Smith DR, Melton SM, May AK, Rue LW 3rd. Prognostic factors in patients with inferior vena cava injuries. Am Surg 1999;65:849–56. ArticlePubMedPDF
- 5. Hampton M, Bew D, Edu S, Nicol A, Naidoo N, Navsaria P. An urban trauma centre experience with abdominal vena cava injuries. S Afr J Surg 2016;54:36–41.
- 6. Michaels D, Pham H, Puckett Y, Dissanaike S. Helicopter versus ground ambulance: review of national database for outcomes in survival in transferred trauma patients in the USA. Trauma Surg Acute Care Open 2019;4:e000211ArticlePubMedPMC
- 7. Schneider AM, Ewing JA, Cull JD. Helicopter transport of trauma patients improves survival irrespective of transport time. Am Surg 2021;87:538–42. ArticlePubMedPDF
- 8. Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma 2002;52:420–5. ArticlePubMed
- 9. Martin M, Izenberg S, Cole F, Bergstrom S, Long W. A decade of experience with a selective policy for direct to operating room trauma resuscitations. Am J Surg 2012;204:187–92. ArticlePubMed
- 10. Matsumoto S, Jung K, Smith A, Coimbra R. Management of IVC injury: repair or ligation? A propensity score matching analysis using the National Trauma Data Bank. J Am Coll Surg 2018;226:752–9. ArticlePubMed
- 11. Ghoreifi A, Djaladat H. Surgical tips for inferior vena cava thrombectomy. Curr Urol Rep 2020;21:51. ArticlePubMedPDF
- 12. Alharbi RJ, Shrestha S, Lewis V, Miller C. The effectiveness of trauma care systems at different stages of development in reducing mortality: a systematic review and meta-analysis. World J Emerg Surg 2021;16:38. ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite