Articles
- Page Path
- HOME > J Trauma Inj > Volume 37(1); 2024 > Article
-
Case Report
Conservative treatment of corpus callosum hemorrhage due to a falling coconut in Indonesia: a case report -
Hanan Anwar Rusidi, MD
 , Ferry Wijanarko, MD
, Ferry Wijanarko, MD
-
Journal of Trauma and Injury 2024;37(1):79-82.
DOI: https://doi.org/10.20408/jti.2023.0052
Published online: January 12, 2024
- 476 Views
- 14 Download
Department of Neurosurgery, PKU Muhammadiyah Hospital, Surakarta, Indonesia
- Correspondence to Hanan Anwar Rusidi, MD Department of Neurosurgery, PKU Muhammadiyah Hospital, Ronggowarsito Street 130, Surakarta 57131, Indonesia Tel: +62-271-714578 Email: drhanan.ar@gmail.com
© 2024 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- The potential for traumatic brain injury resulting from falling coconuts is frequently overlooked. These incidents can cause focal lesions in the form of brain hemorrhage. Corpus callosum hemorrhage due to blunt trauma from a falling object is rare and typically associated with poor prognosis. The purpose of this report is to detail a case of corpus callosum hemorrhage caused by a coconut fall and to discuss the conservative management approach employed. We report the case of a 54-year-old woman who was admitted to the hospital with symptoms of unconsciousness, headache, and expressive aphasia after being struck by a falling coconut. Notably, hemorrhage was detected within the body of the corpus callosum, as revealed by imaging findings. The patient received intensive monitoring and treatment in the intensive care unit, including oxygen therapy, saline infusion, an osmotic diuretic, analgesics, and medication to prevent stress ulcers. The patient demonstrated marked clinical improvement while undergoing conservative treatment. Despite the typically unfavorable prognosis of these rare injuries, our patient exhibited meaningful clinical improvement with conservative treatment. Timely diagnosis and appropriate interventions were crucial in managing the patient’s condition. This report emphasizes the importance of considering traumatic brain injury caused by falling coconuts and highlights the need for further research and awareness in this area.
- Traumatic brain injury (TBI) remains a major cause of morbidity and mortality around the world. Falls and road traffic accidents (RTAs) are the most common causes of TBI [1]. These injuries can also be triggered by object strikes, including impacts by coconuts falling from trees. Data indicate that in the Pacific Islands, TBIs from coconut falls constitute 15% of all surgical department visits [2]. Another study reported that coconut-related injuries accounted for 2.5% of admissions to a hospital in Papua New Guinea [3]. However, it is challenging to find recent epidemiological reports on TBI caused by falling coconuts, as this issue is frequently overlooked and underreported. To date, no globally recognized research is available specifically addressing TBI resulting from falling coconuts.
- Head trauma can lead to focal lesions, manifesting as hemorrhages within the brain. Hemorrhages occurring in the corpus callosum (CC) are rare [4–6]. Such hemorrhages may result from TBI, hemorrhagic brain tumors, encephalitis, arteriovenous malformations, and subarachnoid hemorrhage (SAH) due to ruptured aneurysms in the pericallosal or anterior cerebral arteries [5–7]. Although infrequent in cases of TBI, hemorrhages in the CC can be associated with poor prognosis [6,8].
- In this report, we present a case of head trauma resulting from a coconut fall, which led to a hemorrhagic lesion on the CC. This case is noteworthy because it illustrates a rare and often overlooked type of TBI, caused by falling coconuts and specifically causing hemorrhage in the CC. Our report enriches the scientific literature by offering detailed insights into the clinical presentation, imaging findings, and conservative management of this injury. The unexpected clinical improvement observed during conservative treatment, which ultimately deferred the need for the initially planned surgical procedure, underscores the potential effectiveness of non-surgical interventions in similar cases. Documentation of this case provides valuable information to healthcare professionals and researchers, promoting awareness of TBI caused by falling coconuts and encouraging further investigation into conservative management approaches for such injuries.
INTRODUCTION
- A 54-year-old woman was transferred from a rural hospital to PKU Muhammadiyah Hospital (Surakarta, Indonesia). She reported that she had been struck on the head by a coconut while at a coconut plantation. The patient’s family indicated that she had been unconscious for a period following the coconut strike.
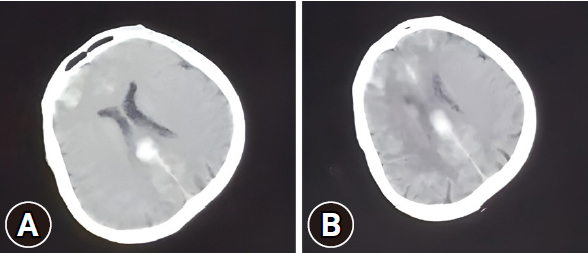
- Upon arrival at the hospital, the patient was experiencing vomiting and epistaxis. No seizures were reported to have occurred during transport to the hospital. In the emergency department, the patient was conscious but displayed expressive aphasia. The patient’s Glasgow Coma Scale (GCS) score was 10. She reported having a headache during the medical history interview. The history also indicated that the patient had not been taking any medications associated with systemic diseases. A physical examination revealed isochoric pupils of 2 mm each, and a right superior palpebral hematoma was observed. Head computed tomography (CT) showed CC hemorrhage, interhemispheric SAH, and both intracerebral hemorrhage (ICH) and SAH in the frontal lobe (Fig. 1).
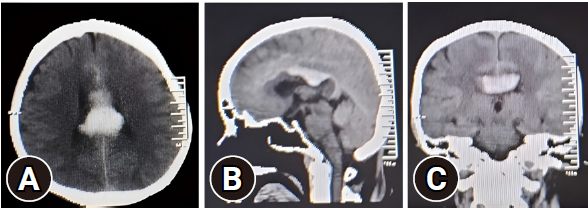
- In the intensive care unit, the patient received a treatment regimen that included oxygen therapy via nasal cannula, infusion of 0.9% sodium chloride, metamizole for pain management, and intravenous omeprazole as an inhibitor of stress ulcers. Additionally, the patient was treated with osmotic diuresis using 100 mL of 20% mannitol, administered three times on the 1st day and twice on the 2nd day of treatment. On the 2nd day, a repeat CT scan revealed an increase in the volume of hemorrhage to approximately double that of the initial scan, now measuring 3.5 cm×1.0 cm×1.5 cm (Fig. 2). The patient continued to exhibit expressive aphasia and a decline in consciousness, as evidenced by a GCS score of 9. The diagnostic conclusion was that, in addition to the CC hemorrhage, the patient had sustained other intracranial lesions, including ICH and SAH. The deterioration in GCS score was suspected to result from elevated intracranial pressure. Despite these findings, no indications for surgical intervention were noted; therefore, the treatment plan remained unchanged, and the patient was kept under close observation.
- On the 3rd day of treatment, the patient exhibited an unexpected improvement, regaining full consciousness (with a corresponding GCS score of 15), displaying clear communication, and exhibiting improved limb motor strength, although her condition was not yet normal. We hypothesized that this improvement was due to the absorption of the hemorrhage and the reduction of cerebral edema following the administration of an osmotic diuretic agent. Consequently, we began to gradually reduce the mannitol therapy while providing intermittent oxygenation. Throughout the treatment period, the patient’s hemodynamic profile remained within the normal range.
- The patient’s condition gradually improved. By the 4th day, she was fully conscious, well-oriented, and able to communicate effectively with a clear voice. She reported a reduction in headache intensity, but continued to experience feelings of weakness and still required assistance to sit up. Consequently, a series of rehabilitation programs were scheduled. The patient was discharged on the following day, with a follow-up appointment set for a specified time.
- Ethics statement
- This study was carried out in accordance with the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from the patient for the publication of the research details and clinical images.
CASE REPORT
- This report demonstrates that a falling coconut can result in TBI with focal lesions, an event seldom reported in the literature. This case suggests the potential for similar lesions in TBI cases with more common causes, such as RTAs and falls.
- TBI caused by a falling coconut can lead to the same types of injuries as other mechanisms and may even prove fatal. The coconut fruit (weighing approximately 2 to 4 kg), combined with the typical height of a coconut tree (about 24 to 30 m), has a substantial potential for impact to the head when the coconut descends, accelerated by gravity. The force of impact can be equivalent to a mass of 1,000 kg [3]. This mechanism involves blunt trauma, wherein a strong translational force is applied to the head. The kinetic energy of the falling coconut, coupled with angular rotation, can result in a shift and shock that stretches and damages axons [4]. Consequently, severe TBI can indeed be caused by a falling coconut fruit. Previous studies have indicated that injuries from falling coconuts can lead to intracranial lesions, as well as fractures of the upper extremities and skull. Fatalities from such incidents have also been reported [2,3]. Additionally, research has shown that a similar fruit, the Brazil nut, has been implicated in causing various types of hemorrhages, including epidural hematoma (EDH), subdural hematoma (SDH), ICH, and SAH [9].
- The present case involved a hemorrhage within the CC, which is rare among cases of head trauma [5,6]. The CC represents the largest white matter structure in the brain, serving to integrate communication pathways between the right and left hemispheres [7]. Anatomically, the CC is composed of the genu, body, splenium, and rostrum [7]. Lesions within the CC can lead to a range of neurological symptoms as a result of the disruption of interhemispheric information transfer.
- Our patient exhibited periods of decreased consciousness, expressive aphasia, and headache upon physical examination. The literature indicates that a range of clinical manifestations may arise from injury to the CC, including headaches, dizziness, seizures, gait disturbances, aphasia, alexia, apraxia, anomia, alien hand syndrome, paraparesis, and (in severe cases) a persistent vegetative state [5–7,10]. Anatomically, the posterior body and splenium of the CC are especially susceptible to involvement in traumatic injuries due to their attachment to the superior dura, which can lead to torsional injuries [11]. In contrast, hemorrhages in the CC resulting from aneurysm rupture typically predominate in the ventral region of the anterior part of the CC [5,12]. In the present case, the hemorrhage was found in the body of the CC. Potential mechanisms for lesions in the CC include shear strain and adhesion between the CC and the falx cerebri. The falx is rigid and sharp-edged, allowing shear forces to create lesions in the interhemispheric area that involve the CC [4,5]. These mechanisms are consistent with the observation of interhemispheric SAH in the present case. Several studies have noted that injuries to the CC often co-occur with interhemispheric, septum pellucidum, and intraventricular hemorrhage [5,13]. The hemorrhage in the body of the CC observed in this case corroborates findings reported in the existing literature. The symptoms presented align with the spectrum of symptoms typically associated with CC hemorrhage [2,3].
- CC injury is associated with high-impact trauma, and it can serve as a predictor of severe TBI with poor prognosis [8,13]. Furthermore, Mata-Mbemba et al. [14] identified the presence of interhemispheric SAH as a risk factor for severe diffuse axonal injury (DAI). However, wide variation means that not every patient with CC injury will experience a poor outcome [8]. In the case of our patient, we noted a marked improvement in overall condition, which led us to opt for conservative treatment. Additionally, surgical intervention in the CC is fraught with risk, as many callosal fibers are in jeopardy of being damaged during hematoma evacuation with a transcallosal interhemispheric approach [5,15]. Potential neurological deficits resulting from such procedures include cognitive, memory, and behavioral impairments, as well as language disorders [15].
- The prognosis for patients with CC injuries is affected by several factors, including age, the level of consciousness upon admission, the extent of the CC lesion, the volume of bleeding, and the presence or absence of DAI, vascular malformation, and/or aneurysm rupture [4–6,8]. Our patient presented with a good baseline GCS score upon admission, was younger than 60 years, exhibited only localized (body) CC involvement without intraventricular hemorrhage, and showed no evidence of vascular abnormalities. The effectiveness of the therapeutic interventions and the progression of bleeding resolution are expected to improve the patient’s clinical condition, allowing for conservative management and regular monitoring.
- This case report emphasizes the importance of TBI resulting from falling coconuts and leading to CC hemorrhage. Although such injuries are uncommon and typically associated with poor prognosis, our patient demonstrated considerable clinical improvement following conservative treatment. Timely diagnosis and appropriate interventions were pivotal in managing the patient’s condition. This report underscores the necessity of recognizing TBI cases caused by falling coconuts and highlights the need for additional research and awareness in this area.
DISCUSSION
-
Author contributions
Conceptualization: all authors; Investigation: all authors; Methodology: all authors; Project administration: all authors; Visualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION

- 1. Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 2017;16:987–1048. ArticlePubMedPDF
- 2. Mulford JS, Oberli H, Tovosia S. Coconut palm-related injuries in the Pacific Islands. ANZ J Surg 2001;71:32–4. ArticlePubMed
- 3. Barss P. Injuries due to falling coconuts. J Trauma 1984;24:990–1. ArticlePubMedPMC
- 4. Du Y, Han Z, Zheng S, Wu T, Yin W. Delayed massive traumatic hematoma in the corpus callosum: two case reports with literature review. NMC Case Rep J 2014;1:37–41. ArticlePubMed
- 5. Elsayed A, Elgamal E, Elsayed AA, Wasserberg J, Kuncz A. Non-surgical treatment of massive traumatic corpus callosum hematoma after blunt head injury: a case report. Neurol Neurochir Pol 2016;50:309–12. Article
- 6. Aji YK, Apriawan T, Bajamal AH. Conservative treatment of corpus callosum hemorrhage in severe traumatic brain injury: a case report. Bali Med J 2017;3:S97–9. ArticlePubMed
- 7. Filippi CG, Cauley KA. Lesions of the corpus callosum and other commissural fibers: diffusion tensor studies. Semin Ultrasound CT MR 2014;35:445–58. ArticlePubMedPDF
- 8. Cicuendez M, Castano-Leon A, Ramos A, Hilario A, Gomez PA, Lagares A. Prognostic value of corpus callosum injuries in severe head trauma. Acta Neurochir (Wien) 2017;159:25–32. ArticlePubMedPMC
- 9. Ideta MM, Oliveira LM, de Castro GL, et al. Traumatic brain injury caused by Brazil-nut fruit in the Amazon: a case series. Surg Neurol Int 2021;12:399. ArticlePubMed
- 10. Kim DS, Choi HJ, Yang JS, Cho YJ, Kang SH. Radiologic determination of corpus callosum injury in patients with mild traumatic brain injury and associated clinical characteristics. J Korean Neurosurg Soc 2015;58:131–6. ArticlePubMedPMC
- 11. Ho J, Zhou Z, Li X, Kleiven S. The peculiar properties of the falx and tentorium in brain injury biomechanics. J Biomech 2017;60:243–7. ArticlePubMed
- 12. Erbaş G, Oner AY, Akpek S, Tokgoz N. Corpus callosum hematoma secondary to isolated inferior sagittal sinus thrombosis. Acta Radiol 2006;47:1085–8. ArticlePubMedPDF
- 13. Matsukawa H, Shinoda M, Fujii M, et al. Intraventricular hemorrhage on computed tomography and corpus callosum injury on magnetic resonance imaging in patients with isolated blunt traumatic brain injury. J Neurosurg 2012;117:334–9. ArticlePubMed
- 14. Mata-Mbemba D, Mugikura S, Nakagawa A, et al. Traumatic midline subarachnoid hemorrhage on initial computed tomography as a marker of severe diffuse axonal injury. J Neurosurg 2018;129:1317–24. ArticlePubMed
- 15. Peltier J, Roussel M, Gerard Y, et al. Functional consequences of a section of the anterior part of the body of the corpus callosum: evidence from an interhemispheric transcallosal approach. J Neurol 2012;259:1860–7. ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite