Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Case Report
Various injury patterns due to combustion (typical but unfamiliar to physicians and easy to miss) in Korea: a case report -
Hyung Il Kim, MD

-
Journal of Trauma and Injury 2023;36(4):393-398.
DOI: https://doi.org/10.20408/jti.2023.0060
Published online: November 30, 2023
- 357 Views
- 16 Download
Department of Emergency Medicine, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- Correspondence to Hyung il Kim, MD Department of Emergency Medicine, Dankook University Hospital, Dankook University College of Medicine, 201 Manghyang-ro, Dongnam-gu, Cheonan 31116, Korea Tel: +81-41-550-6840 Email: hilovesjj@naver.com
• Received: September 6, 2023 • Accepted: September 17, 2023
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Patients transported from fire sites may exhibit various injury patterns. Major trauma, skin burn, inhalation burn, and carbon monoxide poisoning are typical injuries. However, most physicians may be unfamiliar that cyanide poisoning can frequently occur due to combustion. Cyanide poisoning is highly significant owing to high mortality and the existence of antidotes. I present a 35-year-old man who was transported from a burning building and suffered severe metabolic acidosis despite no major bleeding as well as mild carbon monoxide poisoning. I suspected cyanide poisoning and administered the antidote; subsequently, the patient showed improvement. The next day, sudden airway obstruction developed, and emergency endotracheal intubation was performed. The inhalation damage was detected only in the lower airway tract and not in the upper airway. Physicians should be aware of cyanide poisoning and inhalation burn to avoid missing treatment opportunities.
- Patients transported from fire sites may exhibit various injury patterns. Among them, major trauma and skin burns are easy to be detected initially and are familiar to physicians. Carbon monoxide (CO) poisoning and inhalation burns from smoke are relatively less familiar owing to fewer opportunities for treating these types of patients in general hospitals than those in burn centers being specialty hospitals that intensively treat patients with major burns.
- However, most physicians may be unfamiliar that cyanide poisoning can occur at the fire site. Cyanide poisoning is highly significant owing to its high mortality and the existence of antidotes. Although the antidote must be immediately administered, it is stored in some dedicated toxicology centers.
- Here, I present a case of a patient with cyanide poisoning who was transferred from a burning building and was treated with an antidote. Despite no major bleeding and mild CO poisoning, severe metabolic acidosis was initially shown. Subsequently, the symptoms improved following antidote administration. Airway obstruction and pneumonia occurred following hospitalization and were treated with endotracheal intubation, antibiotics, and steroids. Patients at fire sites can be transferred to regional emergency medical centers, regional trauma centers, burn centers, toxicology centers, hyperbaric oxygen chamber centers, and local emergency department (ED). At the prehospital stage, determining the kind of injuries the patient suffered and which damage is the most dangerous is challenging; therefore, the patient can be transferred to any of those hospitals. Therefore, to avoid missing treatment opportunities, physicians must be aware of cyanide poisoning.
INTRODUCTION
- A 35-year-old man with no previous medical history was rescued from a burning building and transferred to our ED at Dankook University Hospital (Cheonan, Korea) by the emergency medical service. At the time of arrival, the paramedics reported that he was suspended from the fourth floor of the building (approximately 10 m) and fell to the ground; therefore, he was brought to the trauma center. Upon initial assessment, the following were his vital signs: blood pressure, 130/70 mmHg; heart rate, 135 beats/min (sinus tachycardia); respiratory rate, 30 beats/min; body temperature, 36 °C; and oxygen saturation, 99%. He was alert but mildly agitated. Second-degree burns of 25% of the total body surface area on both arms and legs and first-degree burns on his face were noted (Fig. 1). Inhalation burn was suspected owing to the soot around his mouth; however, his breathing sound was normal. No external bleeding was observed. Oxygen was supplied, and fentanyl was administered intravenously during the primary survey. Ultrasonography and whole-body computed tomography (CT) scans revealed no bleeding. Arterial blood gas analysis (ABGA) showed severe metabolic acidosis and a high lactate concentration with the following results: pH, 7.099; PaO2, 241 mmHg; PaCO2, 29.3 mmHg; HCO3−, 12.6 mmol/L; base excess, −14.3 mmol/L; and lactate, 12.4 mmol/L. The carboxyhemoglobin (COHb) level was 14.1%, which was not too high to perform hyperbaric oxygen therapy. The results were similar to the initial findings at the serial follow-up ABGA approximately 20 minutes later (Table 1).
- Approximately 30 minutes following the patient’s arrival, the paramedics who rescued the patient came to the hospital and provided corrected information. The patient was found in his bathroom and did not experience a fall; therefore, major trauma could be excluded. While considering the causes of severe metabolic acidosis, major bleeding and severe carbon monoxide poisoning were excluded; however, the patient was suspected of cyanide poisoning due to combustion. Therefore, the antidote (cyanokit, Serb Pharmaceuticals) was administered. ABGA 30 minutes following antidote administration showed an improvement; moreover, follow-up ABGA showed an improvement pattern.
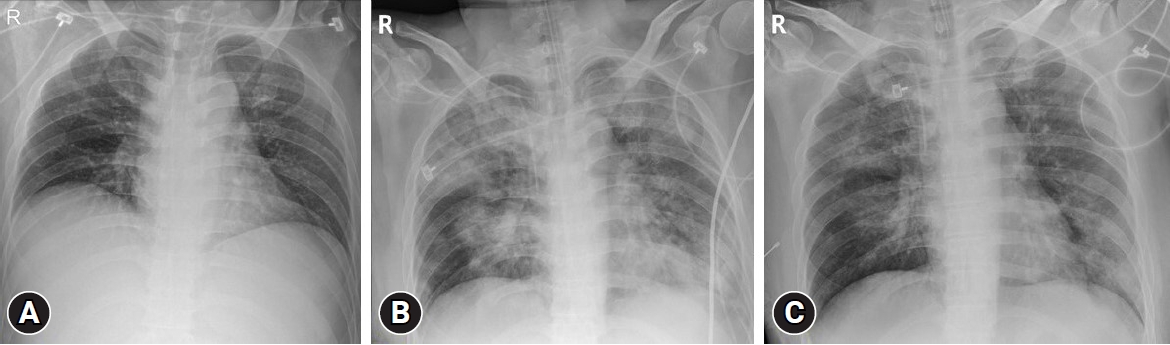
- To confirm airway injury due to inhalation burn, following antidote administration, an otolaryngologist performed upper airway bronchoscopy; however, no specific injury findings were observed. However, owing to the possibility of pneumonia or airway obstruction, he was admitted to the intensive care unit (ICU) and prescribed steroids and antibiotics. The next day, he complained of sudden hoarseness of voice and difficulty in breathing, and stridor was heard on auscultation; therefore, emergency tracheal intubation was performed. Immediately following intubation, upper airway bronchoscopy was performed again; however, no signs of airway injury were revealed. Additionally, fever (above 39 °C) and pneumonia developed (Fig. 2). On the 4th hospitalization day (HD), a pulmonologist performed bronchoscopy, and inhalation injury grade 2 (moderate injury) was discovered (Fig. 3). Pneumonia worsened until the 9th HD; however, it showed improvement from the 10th HD. The patient and his guardians opted for the other treatments to be performed at the hospital nearby his hometown; therefore, he was transferred. Afterward, it was confirmed that he was discharged from that hospital 2 weeks later without complications.
- Ethics statement
- Informed consent was not obtained from the patient because I could not get in touch with him following his discharge from our hospital. However, the Institutional Review Board of Dankook University Hospital approved the study with a waiver of informed consent (No. DKUH 2023-08-029-001).
CASE REPORT
- Major trauma, skin burn, inhalation burn, CO poisoning due to fire smoke, and cyanide poisoning are typical injuries caused by combustion. If the accident is an explosion at an industrial company, exposure to toxic materials depending on the type of compound used is possible. Recently, several burn centers are specializing in treating patients with major burns. Conversely, most other hospitals have become very used to providing only initial resuscitation and subsequently transferring patients to burn centers. Consequently, it is possible that various injuries cannot be considered. Although major trauma and skin burns can be easily identified through gross findings and whole-body CT, CO poisoning can be identified relatively simply by checking the COHb level. However, inhalation burn is not readily identified, and it is easy to overlook cyanide poisoning. This case provides us with the following three lessons.
- Cyanide poisoning
- Cyanide compounds are commonly known as chungsangari in Korea. Cyanide has very high mortality and is quickly absorbed in the body that it has been used as a suicide pill (or spy pill) in the past. In the United States, the gas form of cyanide was used until the 2000s as a means of execution. Even if patients survive, it is known to cause neurological sequelae by leaving serious hypoxic brain damage [1,2]. Cyanide can be produced during combustion, plating, and mining and is also detected in plum pulps, cigarettes, bamboo shoots, cassava, and medicines, including laetrile and nitroprusside [3–6]. The most common situation of cyanide poisoning is during a domestic fire [7]. Tests on survivors of an airplane explosion at the Manchester Airport in 1985 confirmed a significant CO level in approximately 20% of survivors, whereas a significant cyanide level was detected in 90% [8]. Consequently, cyanide poisoning, which is highly dangerous, is known to occur frequently; however, physicians often do not recognize it because it is difficult to confirm it through direct blood tests, and toxidromes are nonspecific. A high suspicion index is required in diagnosis, and only high anion gap metabolic acidosis and high lactate concentration are the available ancillary laboratory tests [9]. Another significant reason of cyanide poisoning is the existence of antidotes. In Korea, the following two types of antidotes are available: Cyanokit and cyanide antidote kit. Cyanokit contains hydroxocobalamin, a precursor to vitamin B12, and is the treatment of choice for cyanide poisoning (Fig. 4) [10,11]. This antidote should be immediately administered owing to rapid cyanide absorption. The problem is that the Cyanokit is classified as an orphan drug; therefore, it is deployed only in 10 dedicated toxicology centers in Korea, and the holding amount is insufficient (an average of three packs per toxicology center), and it is very expensive [12]. The price per pack is ₩2.3 million (US $1,800). Fortunately, no cost is borne by the patient; however, it may have to be moved to a long-distance hospital depending on the location of the fire, and it cannot be supplied to everyone in the event of a large number of patients. Particularly, when hydroxocobalamin was used in the prehospital setting, 41.7% of survival was reported in patients with cardiac arrest [13], which is a significantly higher result than 3% to 10% of survival of cardiac arrest from other causes [14]. Therefore, physicians should be more aware of cyanide poisoning from fire situations. A previous study [11] reported that most burn centers did not administer the proper antidote, and antidotes were unavailable at burn centers in Korea. Is it appropriate to transfer a patient to a burn center following initial resuscitation? In this case, when the patient first visited our ED, it was considered that the cause of metabolic acidosis was bleeding or CO poisoning and not cyanide poisoning. I was convinced of cyanide poisoning only after observing ABGA improvement following Cyanokit administration.
- Typical progression of inhalation burns
- The second significant point is the typical progression of inhalation burns, as shown in this case. In the ED, the patient’s breathing sound was normal, and chest x-ray did not reveal any pathologic findings; however, airway obstruction developed in the ICU the following day, and emergency intubation was required. Moreover, pneumonia developed on the 3rd HD. Recently, inhalation burns are also becoming unfamiliar for most physicians; therefore, it is possible that the patient may be mistaken for being stable only with initial findings in the ED [15,16]. Physicians should be well aware of the possibility of airway obstruction and bacterial pneumonia after several days following the injury. Preemptive endotracheal intubation may often be required [10,17].
- The limitation of upper airway examination on inhalation burns
- Third, of note, bronchoscopy, which can observe only the upper airway in patients with inhalation burns, has limitations. This patient underwent upper airway bronchoscopy twice, and no pathologic findings were revealed. However, grade 2 injury (moderate injury) was noted at the lower airway tract. Grades 2 to 4 have higher mortality than grades 0 to 1 injuries [18]. In the case of an inhalation burn, lower airway evaluation is required. Very high temperature air usually damages the structures above the carina, and chemical injury is usually likely to occur in the lower part [19,20]. Furthermore, airway injury appears after several days rather than immediately following combustion, and overall better outcomes are reported in groups that underwent bronchoscopy; therefore, it is necessary to consider during the hospitalization [21–23].
- Conclusions
- In Korea, there are several types of specialty hospitals, including regional emergency medical centers, regional trauma centers (level I trauma centers), toxicology centers, burn centers, and hyperbaric chamber centers. When transferring the patient, which among the centers is the most appropriate to visit? This is not easy to answer as determining which damage is the most serious at the prehospital stage is very difficult, and these centers separately exist in Korea. It is necessary to improve the healthcare system. However, along with the improvement of the system, it is essential to raise physicians’ awareness of these types of injuries. Cyanokit, an orphan drug, can be sent to another hospital by the parcel service following physicians’ request even if it is not a dedicated toxicology center (Fig. 5). The problem is that most physicians are unaware of this process, and certain antidotes should be immediately administered but the time delay is considerable; therefore, it may not be practical or effective. Moreover, if primary physicians are unaware, they may decide on a simple transfer to a burn center without antidotes following initial stabilization although additional treatment may be required. A fire situation can frequently be classified as a disaster, and there may be different rescuers and transferrers in a disaster situation. Therefore, caution is needed as this may lead to initial incorrect information, as in the present case. Patients from fire sites can present at least five types of injuries, and they can be transferred to any ED depending on their severity and location. Therefore, trauma surgeons, emergency physicians, ED doctors, and burn center workers must be familiar with these injuries.
DISCUSSION
-
Conflicts of interest
The author has no conflicts of interest to declare.
-
Funding
The author received no any financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION
Fig. 1.Second-degree skin burns of the arms and legs. Twenty-five percent of the total body surface area is noted. (A) Right arm. (B) Right leg.


Fig. 2.Chest x-ray images of the patient. (A) Initial chest x-ray. No pathological lesion is observed. (B) Chest x-ray on the 9th hospitalization day. Pneumonia is observed in both lungs. (C) Chest x-ray on the 10th hospitalization day. Improved status of pneumonia.
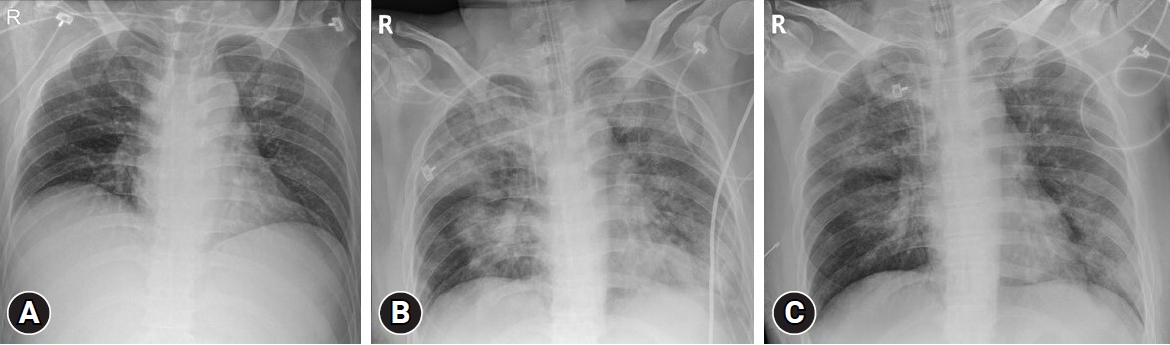
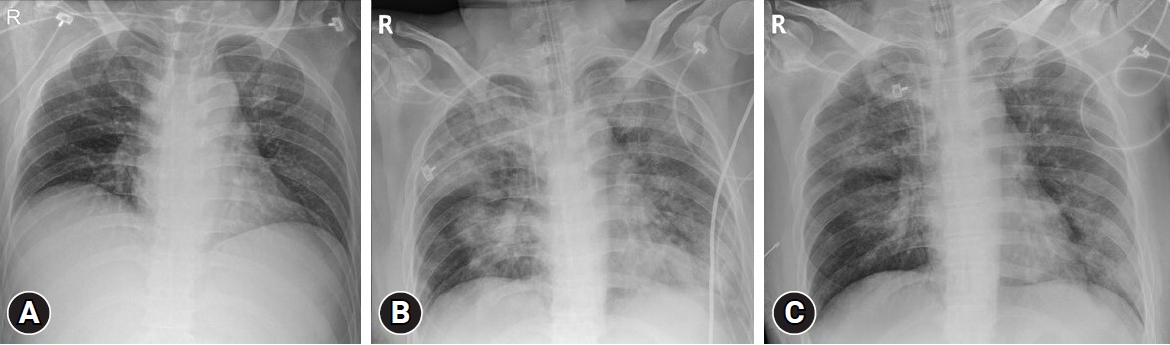
Fig. 3.Bronchoscopic findings. Moderate edema and congestion as well as carbon soot deposition are noted. (A) Carina. (B) Left main bronchus.
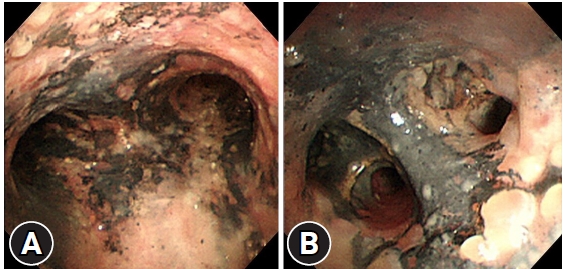
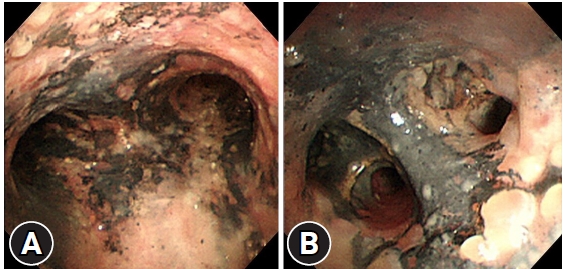
Fig. 4.Images of Cyanokit (Serb Pharmaceuticals). (A) Cyanokit pack, the antidote for cyanide poisoning. (B, C) It is infused after mixing 200 mL of normal saline.


Fig. 5.The text message captured from the author’s phone. Fomepizole is an antidote for methanol poisoning and is also an orphan drug. Another hospital physician requested this drug using the antidote request system. After receiving the request text message at 18:23, it took 45 minutes to send the drug to that hospital. Furthermore, it took another 1 hour in estimate for the transport. This orphan drug can be used in other hospitals; however, it takes time.
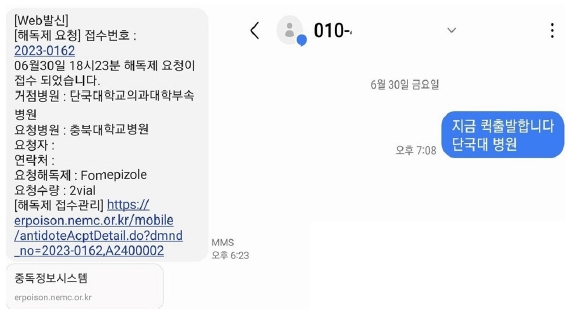
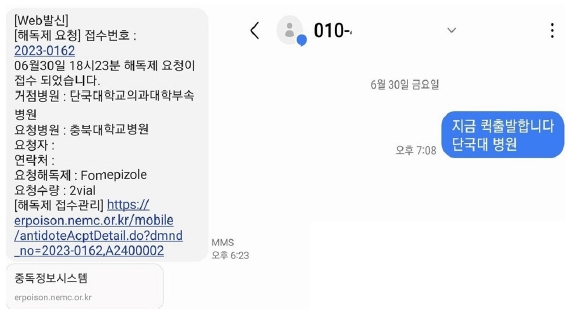
Table 1.Values of serial arterial blood gas analyses
- 1. Tursky T, Sajter V. The influence of potassium cyanide poisoning on the gamma-aminobutyric acid level in rat brain. J Neurochem 1962;9:519–23. PubMed
- 2. Mohan A, Lee T, Sachdev P. Surviving acute cyanide poisoning: a longitudinal neuropsychological investigation with interval MRI. BMJ Case Rep 2014;2014:bcr2013203025. ArticlePubMedPMC
- 3. Cummings TF. The treatment of cyanide poisoning. Occup Med (Lond) 2004;54:82–5. ArticlePubMed
- 4. Hall AH, Linden CH, Kulig KW, Rumack BH. Cyanide poisoning from laetrile ingestion: role of nitrite therapy. Pediatrics 1986;78:269–72. ArticlePubMedPDF
- 5. O’Brien B, Quigg C, Leong T. Severe cyanide toxicity from ‘vitamin supplements’. Eur J Emerg Med 2005;12:257–8. ArticlePubMed
- 6. Huzar TF, George T, Cross JM. Carbon monoxide and cyanide toxicity: etiology, pathophysiology and treatment in inhalation injury. Expert Rev Respir Med 2013;7:159–70. ArticlePubMed
- 7. Megarbane B, Delahaye A, Goldgran-Toledano D, Baud FJ. Antidotal treatment of cyanide poisoning. J Chin Med Assoc 2003;66:193–203. PubMed
- 8. Walsh DW, Eckstein M. Hydrogen cyanide in fire smoke: an underappreciated threat. Emerg Med Serv 2004;33:160–3. PubMed
- 9. Baud FJ, Barriot P, Toffis V, et al. Elevated blood cyanide concentrations in victims of smoke inhalation. N Engl J Med 1991;325:1761–6. ArticlePubMed
- 10. Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med 2013;21:31. ArticlePubMedPMCPDF
- 11. Dumestre D, Nickerson D. Use of cyanide antidotes in burn patients with suspected inhalation injuries in North America: a cross-sectional survey. J Burn Care Res 2014;35:e112–7. PubMed
- 12. National Emergency Medical Center. Intoxication information system [Internet]. National Medical Center of Korea; [cited 2023 Aug 10]. Available from: https://erpoison.nemc.or.kr/introduction/poisIntrdct.do.
- 13. Fortin JL, Giocanti JP, Ruttimann M, Kowalski JJ. Prehospital administration of hydroxocobalamin for smoke inhalation-associated cyanide poisoning: 8 years of experience in the Paris Fire Brigade. Clin Toxicol (Phila) 2006;44 Suppl 1:37–44. ArticlePubMed
- 14. Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008;300:1423–31. ArticlePubMedPMC
- 15. McCall JE, Cahill TJ. Respiratory care of the burn patient. J Burn Care Rehabil 2005;26:200–6. PubMed
- 16. Pruitt BA Jr, Flemma RJ, DiVincenti FC, Foley FD, Mason AD Jr, Young WG Jr. Pulmonary complications in burn patients: a comparative study of 697 patients. J Thorac Cardiovasc Surg 1970;59:7–20. PubMed
- 17. Endorf FW, Dries DJ. Noninvasive ventilation in the burned patient. J Burn Care Res 2010;31:217–28. ArticlePubMed
- 18. Endorf FW, Gamelli RL. Inhalation injury, pulmonary perturbations, and fluid resuscitation. J Burn Care Res 2007;28:80–3. ArticlePubMed
- 19. Fein A, Leff A, Hopewell PC. Pathophysiology and management of the complications resulting from fire and the inhaled products of combustion: review of the literature. Crit Care Med 1980;8:94–8. PubMed
- 20. Herndon DN, Thompson PB, Traber DL. Pulmonary injury in burned patients. Crit Care Clin 1985;1:79–96. ArticlePubMed
- 21. Carr JA, Phillips BD, Bowling WM. The utility of bronchoscopy after inhalation injury complicated by pneumonia in burn patients: results from the National Burn Repository. J Burn Care Res 2009;30:967–74. ArticlePubMed
- 22. Arakawa A, Fukamizu H, Hashizume I, et al. Macroscopic and histological findings in the healing process of inhalation injury. Burns 2007;33:855–9. ArticlePubMed
- 23. Mosier MJ, Gamelli RL, Halerz MM, Silver G. Microbial contamination in burn patients undergoing urgent intubation as part of their early airway management. J Burn Care Res 2008;29:304–10. ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite