Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Case Report
Rare complication of skin necrosis after endoscopic debridement and cutaneo-fascial suture for a massive Morel-Lavallée lesion in Korea: a case report -
Youngmin Kim, MD1
 , Jayun Cho, MD1
, Jayun Cho, MD1 , Myung Jin Jang, MS2
, Myung Jin Jang, MS2 , Kang Kook Choi, MD1,2
, Kang Kook Choi, MD1,2
-
Journal of Trauma and Injury 2023;36(3):304-309.
DOI: https://doi.org/10.20408/jti.2023.0007
Published online: August 25, 2023
- 668 Views
- 19 Download
1Department of Trauma Surgery, Gachon University Gil Medical Center, Incheon, Korea
2Department of Traumatology, Gachon University College of Medicine, Incheon, Korea
- Correspondence to Kang Kook Choi, MD Department of Traumatology, Gil Medical Center, Gachon University College of Medicine, 21 Namdong-daero 774beon-gil, Namdong-gu, Incheon 21565, Korea Tel: +82-32-460-3010 Email: choikangkook@gilhospital.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- A Morel-Lavallée lesion (MLL) is a pathologic fluid collection within an abnormally formed space, resulting from an internal degloving injury between the muscle fascia and subcutaneous fat layer. Due to its resistance to conservative treatments such as drainage or compression dressing, various therapeutic methods have been developed for MLL. However, no standardized guidelines currently exist. Recently, endoscopic debridement and cutaneo-fascial suture (EDCS) has been introduced for the treatment of MLL, particularly for large lesions resistant to conservative approaches. While this procedure is known to be effective, limited reports are available on potential complications. The authors present a case of skin necrosis following EDCS for a massive MLL.
- A Morel-Lavallée lesion (MLL) is a pathologic fluid collection within an abnormally formed space, resulting from an internal degloving injury between the muscle fascia and subcutaneous fat layer [1]. Due to its resistance to conservative treatments such as drainage or compression dressing, various therapeutic methods have been developed for MLL [2,3]. However, no standardized guidelines currently exist. Recently, endoscopic debridement and cutaneo-fascial suture (EDCS) has been introduced for the treatment of MLL [4–8]. This procedure is known to be effective for large MLLs that are resistant to conservative treatments. However, limited reports are available on potential complications. The authors present a case of skin necrosis following EDCS for a massive MLL.
INTRODUCTION
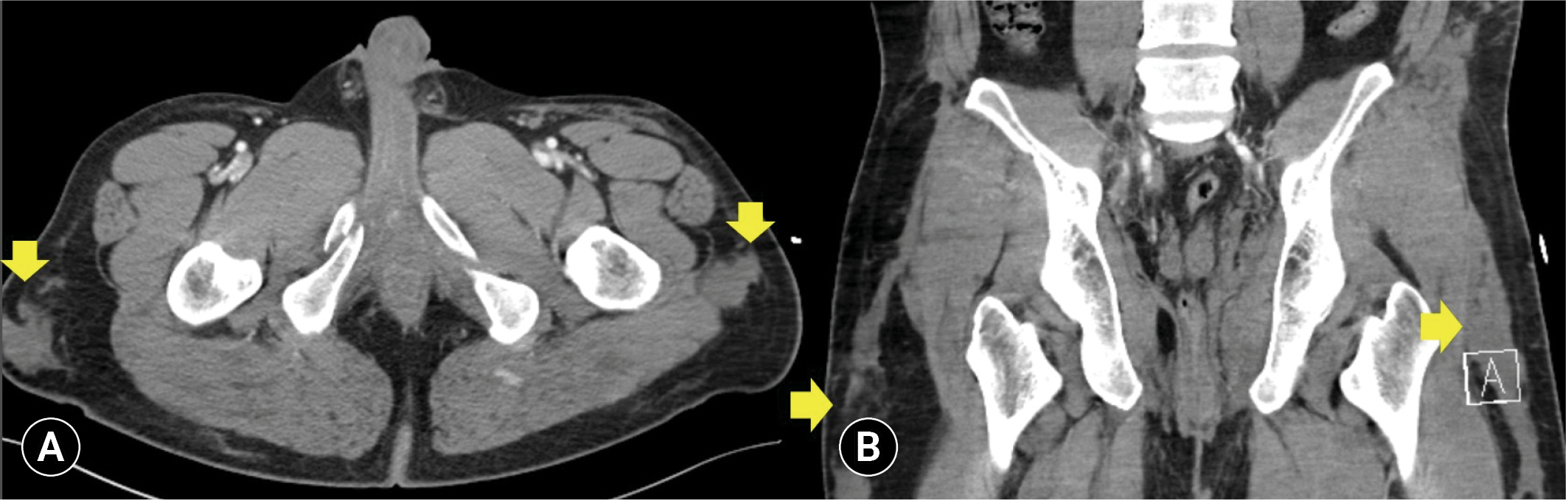
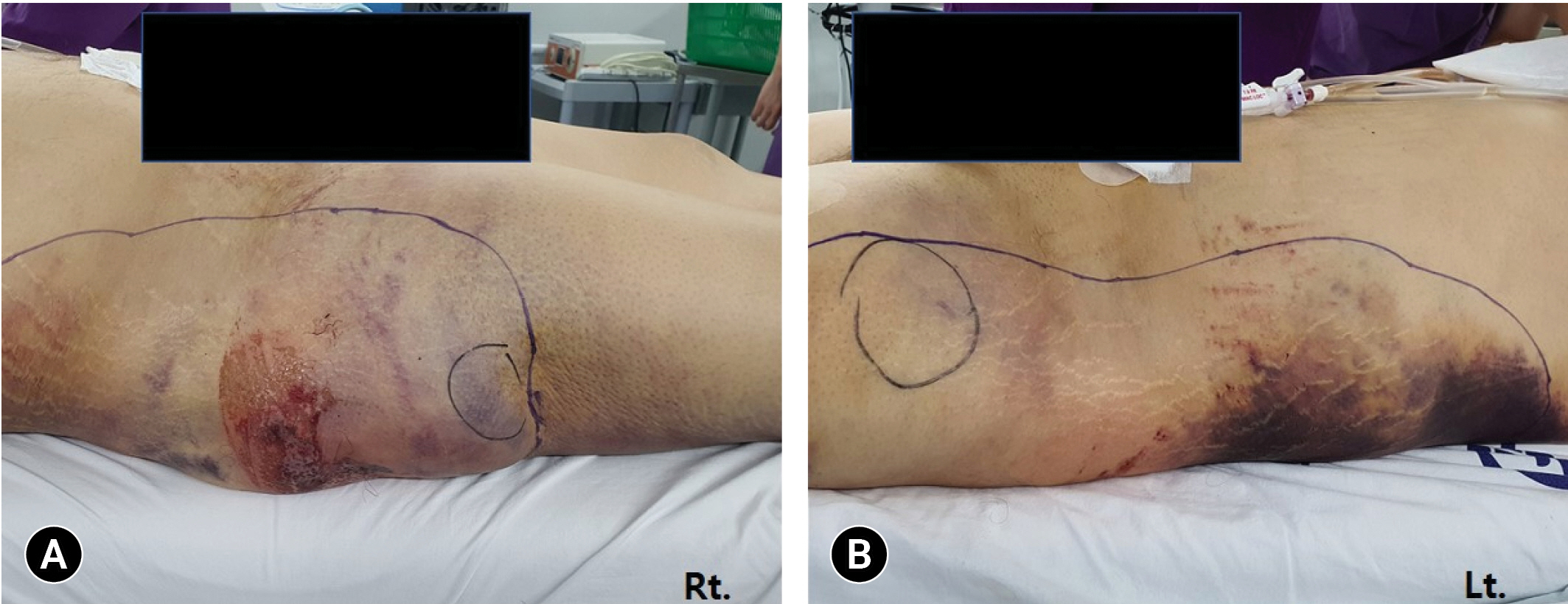
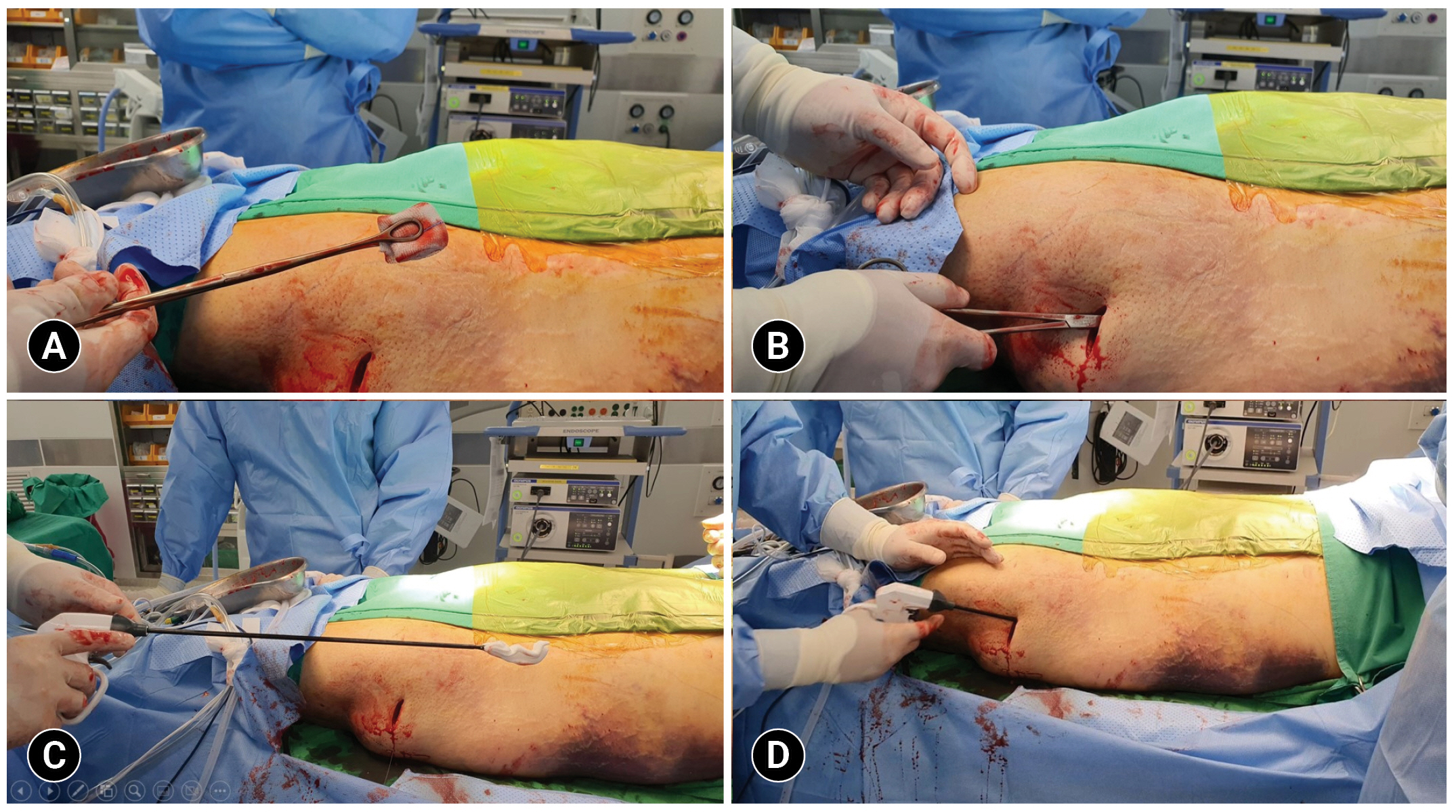
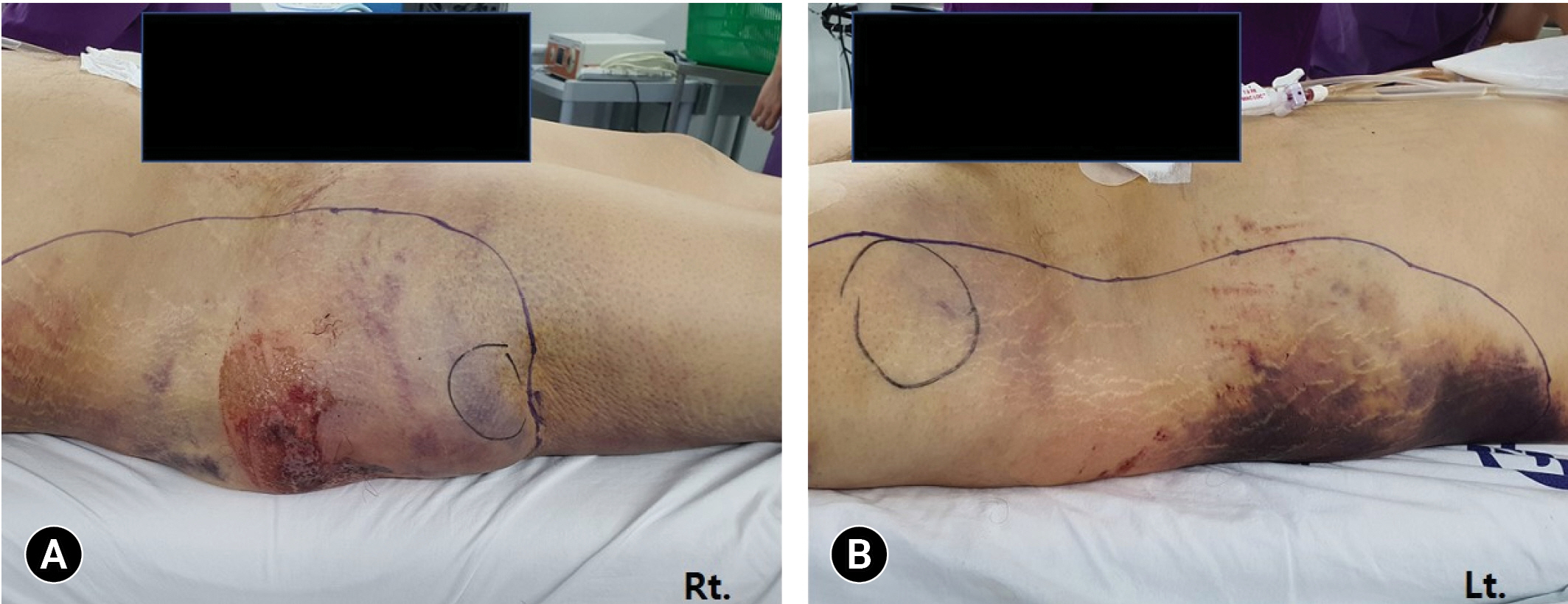
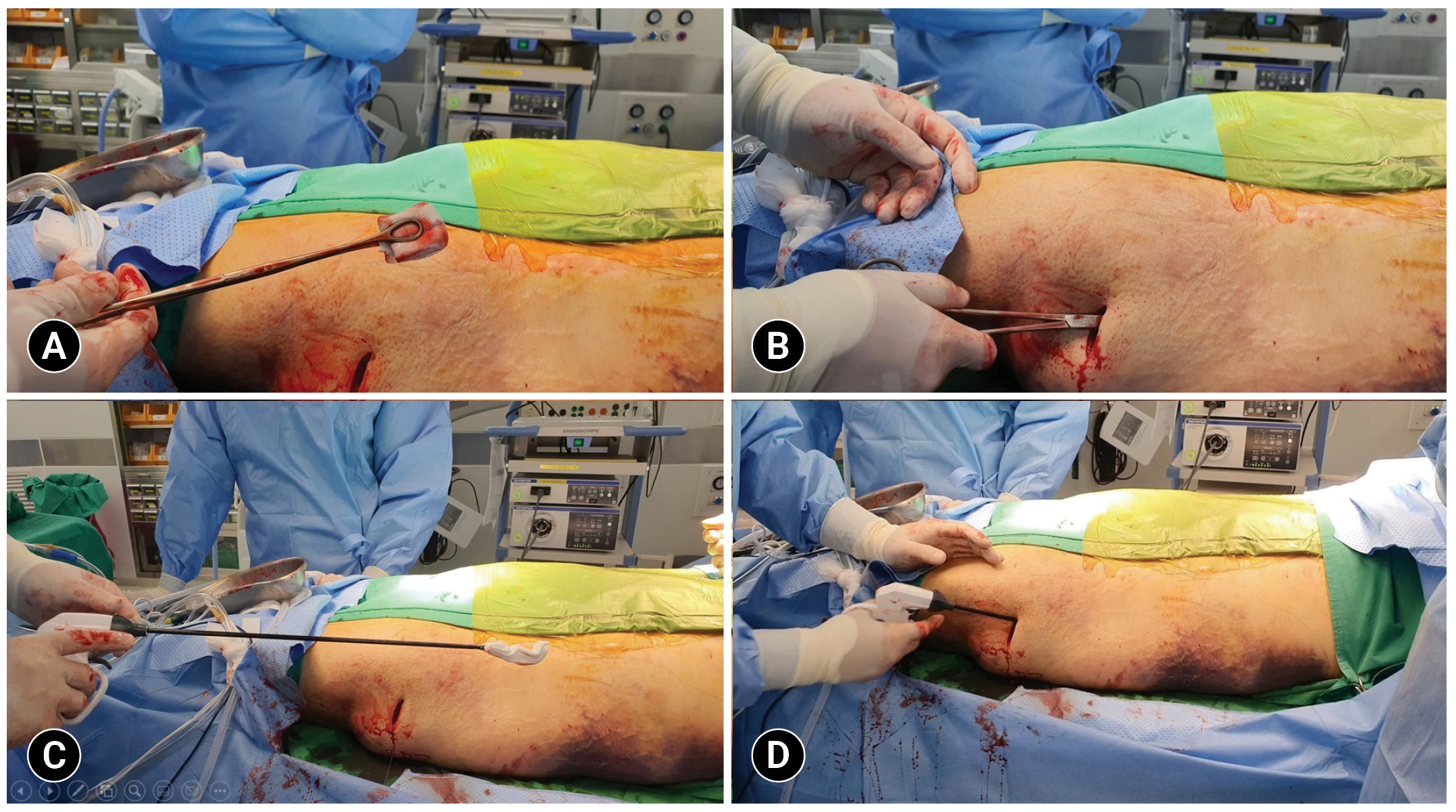
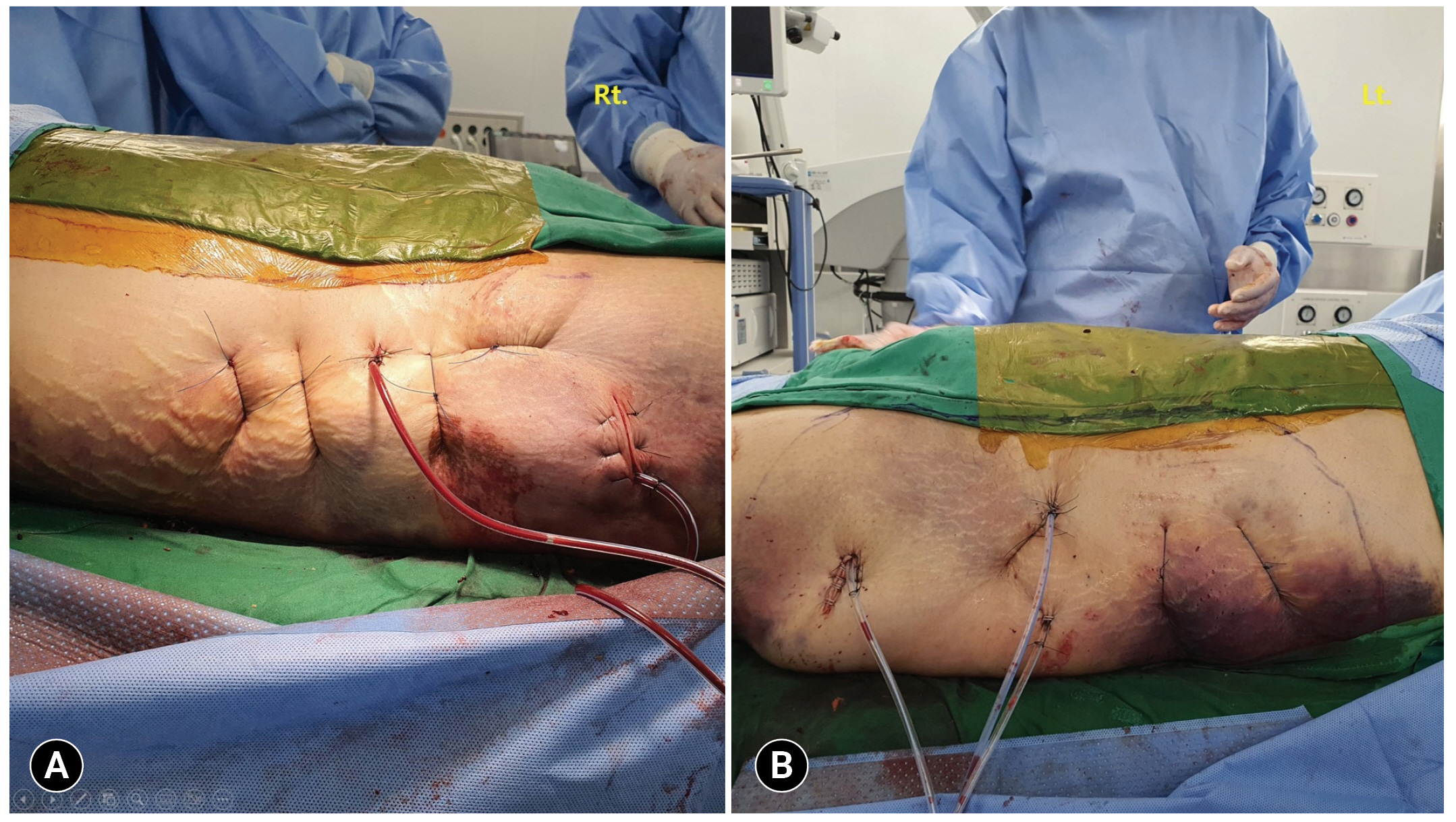
- A 43-year-old man was transferred to Gachon University Gil Medical Center (Incheon, Korea) following a pedestrian traffic accident. His hemodynamic status was stable. A computed tomography (CT) scan revealed multiple pelvic fractures and contrast extravasation in the pelvic cavity. The patient underwent angioembolization to address the pelvic bleeding. Hemorrhage from the bilateral internal iliac arteries was observed and embolized. The CT scan showed hematomas in the bilateral hips (Fig. 1). On day 5 of hospitalization, the patient reported pain and fluctuation in both hips. Based on the CT scan findings and physical examination, the authors diagnosed the fluctuation as an MLL. EDCS was planned for the lesion, and the operation was performed on the same day. In the operating room, MLL was noted on the right (40×50 cm) and left (40×60 cm) hip/flank (Fig. 2). A 2-cm skin incision was made for the scope trocar, and two additional skin incisions were made for the working ports. Initially, debridement was performed using a sponge stick (Fig. 3). After debridement, saline irrigation was conducted through the skin incision (Fig. 4). Following debridement and irrigation, trocars were placed, and CO2 gas inflation was performed. The gas-inflated pressure was approximately 10 mmHg, and it did not interfere with visibility or worsen the wound. Under videoscopy, additional debridement and hemostasis were performed (Fig. 5). The subcutaneous fat layer was attached to the fascia with an endoscopic suture using absorbable suture material, and video-assisted cutaneo-fascial suturing from the skin to fascia was performed using 1-0 nylon (Fig. 6). Two drains were placed in the cavity. The cutaneo-fascial sutures were removed sequentially over 2 weeks. After the stitch removal, necrosis of the skin (5 cm in diameter) was found on the right hip (Fig. 7). The lesion was debrided, and negative-pressure wound therapy was applied. The patient was discharged on day 32 of the hospital stay after improvement of the skin defect.
- Ethics statement
- This study was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GDIRB2023-052). Written informed consent for publication of the research details and clinical images was obtained from the patient.
CASE REPORT
- MLL arises due to shearing injury and typically affects the greater trochanter, flank, and buttock [9]. Early treatment of MLL is crucial, as untreated cases may progress to further tissue necrosis and encapsulation, ultimately leading to serious infection [8,10,11].
- The treatment options for MLL can be categorized into conservative (or nonsurgical therapy) and surgical intervention. Initially, conservative therapy involves external compression and percutaneous drainage [12–14]. While this approach is simple and minimally invasive, it is considered less effective than surgery and requires a longer treatment period for advanced MLL cases [5,7].
- Surgical treatment should be considered for advanced or large MLLs. These often involve substantial amounts of necrotic debris, unabsorbed turbid exudate, and organized capsules. Nickerson et al. [15] demonstrated that the volume of fluid aspirated from an MLL is associated with its resolution rate. In their study, 83% of patients with more than 50 mL of fluid aspirated from the MLL experienced recurrence following percutaneous drainage.
- Open debridement and primary closure is the traditional surgical approach for managing MLL. However, the long skin incision and subsequent pain are drawbacks of this method. EDCS has been developed to address these disadvantages associated with open debridement [4–8]. As previously reported, the EDCS technique shares similar components with open debridement, including drainage of all fluid collections, endoscopic removal of necrotic tissue, endoscopic or endoscopy-assisted suturing, and compression dressing [4–8]. Regarding endoscopic or endoscopy-assisted suture, a suture between the subcutaneous fat layer and fascia within the cavity is preferable to a cutaneo-fascial suture. However, these authors had to employ both methods due to the friable and thin nature of the subcutaneous fat layer. While previous reports have described the use of numerous cutaneo-fascial sutures [4–8], we placed only 3 or 4 similarly-sized cutaneo-fascial sutures in the MLLs, as this was sufficient for approximation between the subcutaneous fat layer and the fascia. An excessive cutaneo-fascial suture may lead to complications such as pain, scarring, infection, and skin necrosis. The larger the MLL, the more advantageous EDCS becomes.
- Unlike conventional laparoscopic surgery, no standard trocar insertion position exists for EDCS in the treatment of MLL. However, the following approach may be optimal. After closing the small skin incision from a previous debridement, the authors inserted three trocars along the long axis of the MLL to accommodate a scope and two working ports. Multiple endoscopic sutures were placed using a scope, which was inserted through the three trocars in a rotating manner. For MLLs larger than this, additional trocars might be required.
- In this patient, a serious complication developed in the form of skin necrosis on the right hip, although this was relatively small compared to the total MLL (40×50 cm). Several possible causes existed for the skin necrosis, which may have occurred due to a combination of factors. First, the location of the necrotic lesion was the most friable site of the wound, situated in the central portion of the MLL. As a result, this area would have received less blood supply than other parts of the lesion. Based on this hypothesis, employing a minimally invasive endoscopic procedure in this case may have reduced the extent of skin necrosis. Second, the lesion was located on the greater trochanter of the femur, which is the most prominent portion anatomically. The skin and subcutaneous fat layers on the greater trochanter of the femur are thinnest in the hip area, making it particularly susceptible to necrosis. Other potential causes could relate to the surgical procedure. The cutaneo-fascial suture may have been too tight, leading to skin ischemia. Additionally, the debridement might have been too excessive, causing injury to the affected area. Given these concerns, practitioners must carefully consider these factors when implementing the EDCS technique to prevent skin necrosis. Proper attention to the tension of cutaneo-fascial sutures and the extent of debridement can help minimize potential complications and ensure a more successful outcome. Fortunately, the wound in the present case improved after using negative-pressure wound therapy alone without the need for a skin graft.
- This study describes the successful management of a very large MLL using EDCS. Skin necrosis is a potential complication following the procedure. Surgeons must exercise caution when performing EDCS on vulnerable MLL lesions.
DISCUSSION
-
Author contributions
Conceptualization: KKC; Data curation: KKC, JC, MJJ; Formal analysis: KKC; Methodology: YK, KKC, MJJ; Project administration: KKC; Visualization: YK, KKC; Writing–original draft: YK, KKC; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
Jayun Cho and Kang Kook Choi serve on the Editorial Board of the Journal of Trauma and Injury, but were not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION

- 1. Agrawal U, Tiwari V. Morel Lavallee lesion. StatPearls; 2023.
- 2. Seo BF, Kang IS, Jeong YJ, Moon SH. A huge Morel-Lavallée lesion treated using a quilting suture method: a case report and review of the literature. Int J Low Extrem Wounds 2014;13:147–51. PubMed
- 3. Molina BJ, Ghazoul EN, Janis JE. Practical review of the comprehensive management of Morel-Lavallee lesions. Plast Reconstr Surg Glob Open 2021;9:e3850PubMedPMC
- 4. Kim S. Endoscopic treatment of Morel-Lavallee lesion. Injury 2016;47:1064–6. ArticlePubMed
- 5. Koc BB, Somorjai N, Kiesouw EP, et al. Endoscopic debridement and fibrin glue injection of a chronic Morel-Lavallée lesion of the knee in a professional soccer player: a case report and literature review. Knee 2017;24:144–8. ArticlePubMed
- 6. Walls A, McMahon SE, MacDonald J, Bunn J. Endoscopic surgical management of a large Morel-Lavallee lesion. BMJ Case Rep 2017;2017:bcr2017221343. PubMedPMC
- 7. Liu M, Liu L, Zhou X, et al. A novel surgical technique for treatment of Morel-Lavallée lesion: endoscopic debridement combined with percutaneous cutaneo-fascial suture. Injury 2018;49:1630–3. ArticlePubMed
- 8. Chan YL, Lui TH. Endoscopic resection of chronic Morel-Lavallée lesion of the knee. Arthrosc Tech 2021;10:e1915–9. ArticlePubMedPMC
- 9. Anakwenze OA, Trivedi V, Goodman AM, Ganley TJ. Concealed degloving injury (the Morel-Lavallée lesion) in childhood sports: a case report. J Bone Joint Surg Am 2011;93:e148. PubMed
- 10. Cruz N, Jimenez R. Morel-Lavallée lesion diagnosed 25 years after blunt trauma. Int J Surg Case Rep 2021;81:105733. PubMedPMC
- 11. Huang W, Luo Y, Yang E. Application of channel screw combined with skin-stretching technique in treatment of pelvic fracture with severe Morel-Lavallée lesion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2021;35:973–7. PubMedPMC
- 12. Demirel M, Dereboy F, Ozturk A, Turhan E, Yazar T. Morel-Lavallee lesion: results of surgical drainage with the use of synthetic glue. Saudi Med J 2007;28:65–7. PubMed
- 13. Seo BF, Jung SN, Sohn WI, Kwon H. Lymph node compression of the lesser occipital nerve: a cause of migraine. J Plast Reconstr Aesthet Surg 2011;64:1657–60. ArticlePubMed
- 14. Wei D, Wang Y, Yuan J, et al. One-stage operation for pelvis and acetabular fractures combined with Morel-Lavallee injury by internal fixation associated with vacuum sealing drainage. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014;28:38–42. PubMed
- 15. Nickerson TP, Zielinski MD, Jenkins DH, Schiller HJ. The Mayo Clinic experience with Morel-Lavallée lesions: establishment of a practice management guideline. J Trauma Acute Care Surg 2014;76:493–7. PubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST




 PubReader
PubReader ePub Link
ePub Link Cite
Cite