Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Case Report
Successful minimally invasive management using transcatheter arterial embolization in a hemodynamically stable elderly patient with mesenteric vascular injury in a hybrid emergency room system in Korea: a case report -
So Ra Ahn, MD1
 , Joo Hyun Lee, MD2
, Joo Hyun Lee, MD2 , Sang Hyun Seo, MD3
, Sang Hyun Seo, MD3 , Chan Yong Park, MD4
, Chan Yong Park, MD4
-
Journal of Trauma and Injury 2023;36(4):435-440.
DOI: https://doi.org/10.20408/jti.2023.0018
Published online: July 25, 2023
- 1,796 Views
- 20 Download
1Department of Trauma Surgery, Wonkwang University School of Medicine, Iksan, Korea
2Department of Surgery, Wonkwang University School of Medicine, Iksan, Korea
3Department of Radiology, Wonkwang University School of Medicine, Iksan, Korea
4Division of Trauma Surgery, Department of Surgery, Seoul National University Hospital, Seoul, Korea
- Correspondence to Chan Yong Park, MD Division of Trauma Surgery, Department of Surgery, Seoul National University Hospital, 101 Daehak-ro, Jongno-gu, Seoul 03080, Korea Tel: +82-2-2072-2817 Email: trauma-park@naver.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Mesenteric injury occurs rarely in cases associated with blunt abdominal trauma. Despite its low incidence, mesenteric injury can lead to fatal outcomes such as hypovolemic shock due to hemoperitoneum or sepsis due to intestinal ischemia, or perforation-related peritonitis. For mesenteric injuries, especially those involving massive bleeding, intestinal ischemia, and perforation, the standard treatment is surgery. However, in the case of operative management, it should be borne in mind that there is a possibility of complications and mortality during and after surgery. The usefulness of transcatheter arterial embolization (TAE) is well known in solid organs but is controversial for mesenteric injury. We present a 75-year-old man with mesenteric injury due to blunt abdominal trauma. Initial abdominal computed tomography showed no hemoperitoneum, but a mesenteric contusion and pseudoaneurysm with a diameter of 17 mm were observed near the origin of the superior mesenteric artery. Since there were no findings requiring emergency surgery such as free air or intestinal ischemia, it was decided to perform nonoperative management with TAE using microcoils in hybrid emergency room system. TAE was performed successfully, and there were no complications such as bleeding, bowel ischemia, or delayed bowel perforation. He was discharged on the 23rd day after admission with percutaneous catheter drainage for drainage of mesenteric hematoma. The authors believe that treatment with TAE for highly selected elderly patients with mesenteric injuries has the positive aspect of minimally invasive management, considering the burden of general anesthesia and the various avoidable intraoperative and postoperative complications.
- Mesenteric injuries caused by blunt trauma occur infrequently, appearing in about 1% to 5% [1–3]. However, it can cause life-threatening hemorrhage, bowel ischemia, and perforation, and is of great clinical importance [4,5]. Surgery is the standard of treatment for mesenteric injuries, particularly those involving massive bleeding, bowel ischemia, and perforation. [6,7]. However, in the case of operative management, it should be borne in mind that there is a possibility of complications and mortality during and after surgery [8]. The usefulness of transcatheter arterial embolization (TAE) is well known in solid organ injuries such as liver, spleen, and kidney, but less attention has been paid to mesenteric injuries [9]. The authors are to report a case of successful nonoperative management with TAE for a 75-year-old male patient with mesenteric injury with pseudoaneurysm due to blunt trauma. According to the medical history, the patient underwent open abdominal surgery for gastric cancer, and is taking antiplatelet drugs after stent insertion due to myocardial infarction.
INTRODUCTION
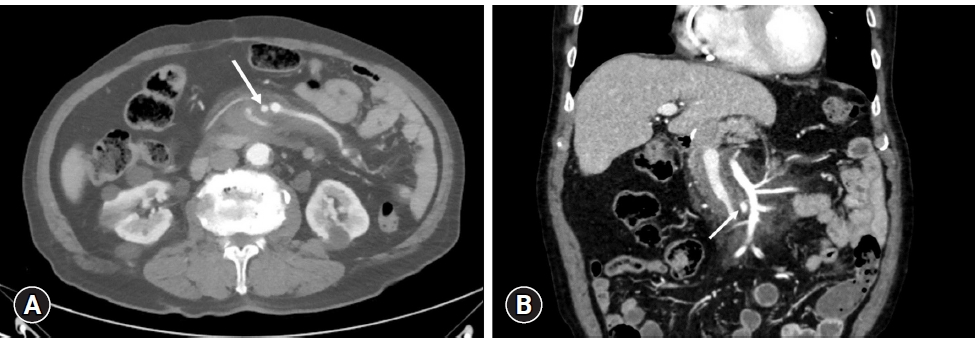
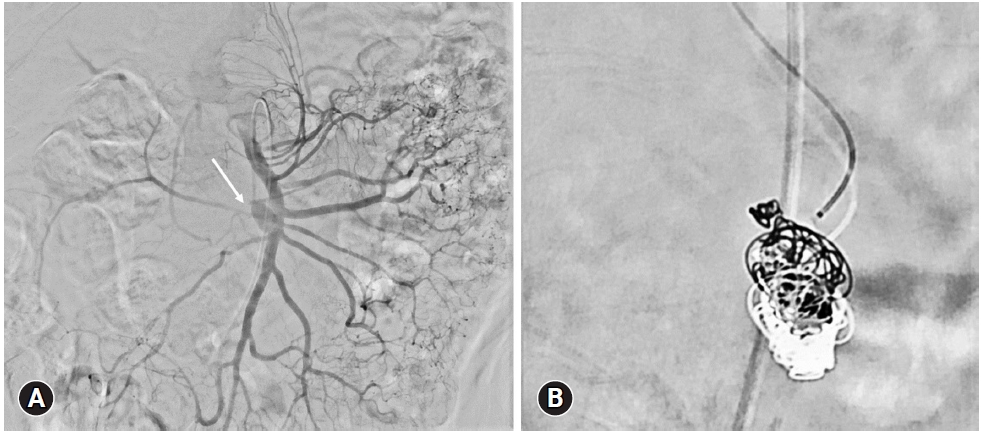
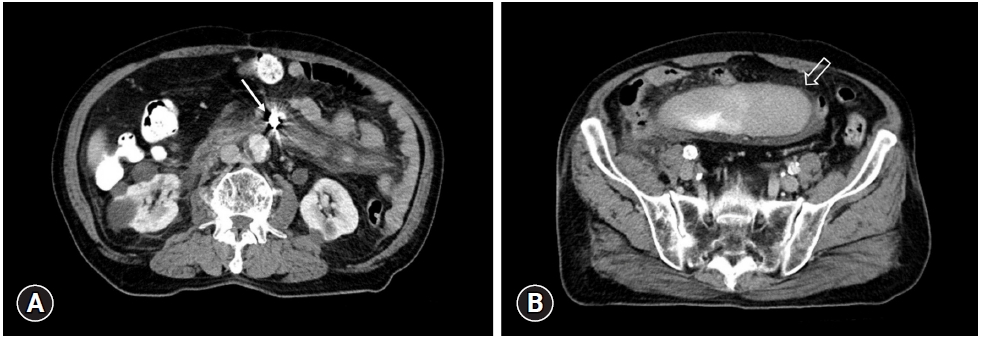
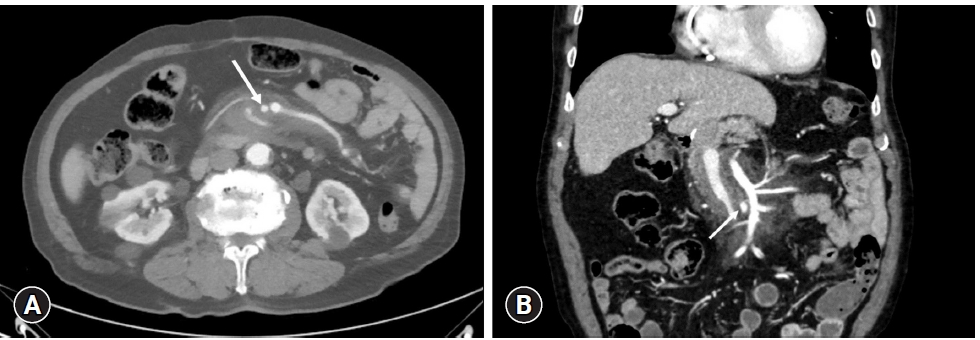
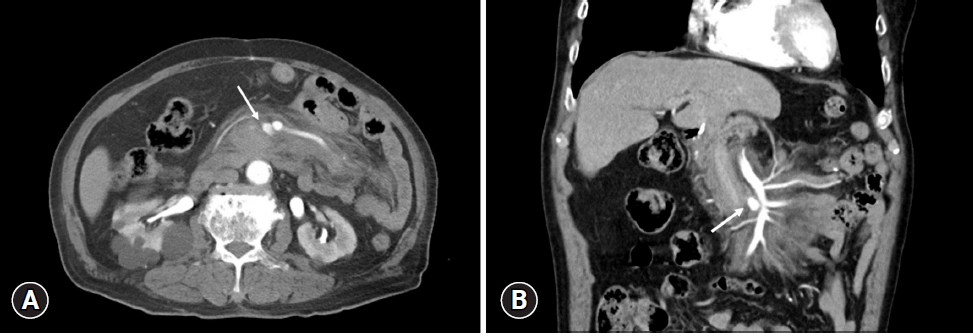
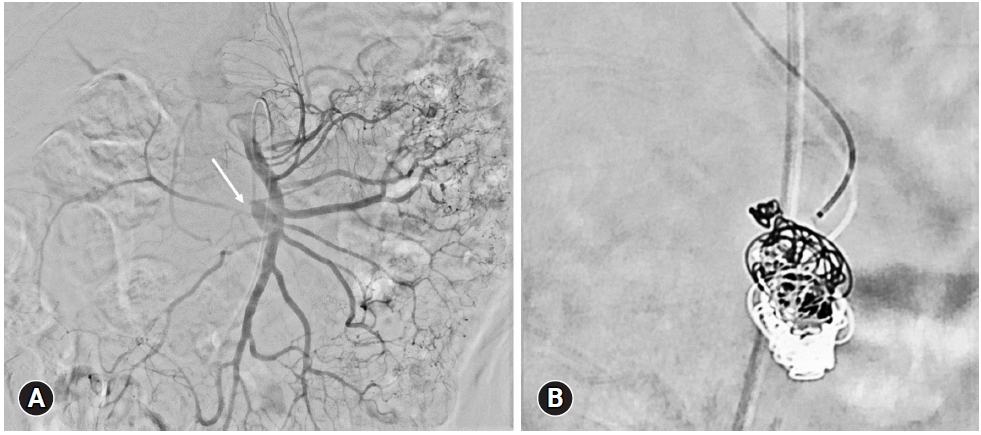
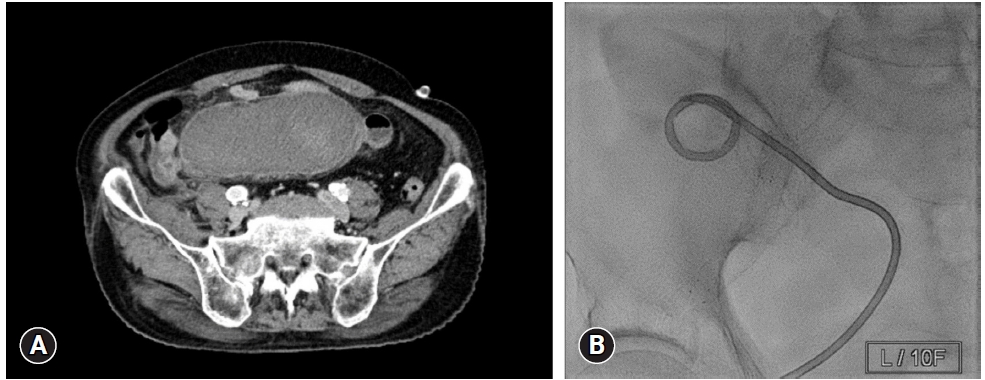
- A 75-year-old man complained of abdominal pain as a result of a traffic accident while driving. The patient was diagnosed with mesenteric vascular injury on abdominal computed tomography (CT) performed at the previous hospital and was transferred to Wonkwang University Hospital Regional Trauma Center (Iksan, Korea) for surgical treatment. The patient was immediately admitted to hybrid emergency room system (HERS) and treated by a trauma team including an interventional radiologist. The patient's Glasgow Coma Scale was 15 and initial vital signs were stable (blood pressure 148/84 mmHg and pulse 69 beats/min). The initial hemoglobin level was 11.5 g/dL, and 1 U of universal O+ packed red blood cells were transfused immediately after admission. His medical history revealed that he underwent open surgery for gastric cancer and was taking an antiplatelet drug (clopidogrel) after a coronary artery stent was inserted due to myocardial infarction. Abdominal CT performed at the previous hospital did not show a hemoperitoneum, and a mesenteric contusion and pseudoaneurysm with a diameter of 17 mm were found near the origin of the superior mesenteric artery (SMA) (Fig. 1). There were no findings requiring emergency surgery such as free air or intestinal ischemia. Without the need to move the patient to another room, CT was performed at HERS to check for injuries to other body regions, and then a treatment plan was decided. Injury to other body regions was not observed, but the size of the pseudoaneurysm increased to about 20 mm (Fig. 2). The patient was hemodynamically stable and there were no findings suggestive of bowel ischemia or perforation, so it was decided to perform TAE in HERS. Angiography revealed a pseudoaneurysm of about 20 mm in size, which occurred in the injured area of the SMA wall, about 100 mm from the SMA root, and embolization using detachable coils (Interlock, Boston Scientific; Concerto, Medtronic) was performed for a pseudoaneurysm. Also feeding artery was embolized by two Interlocks (Fig. 3).
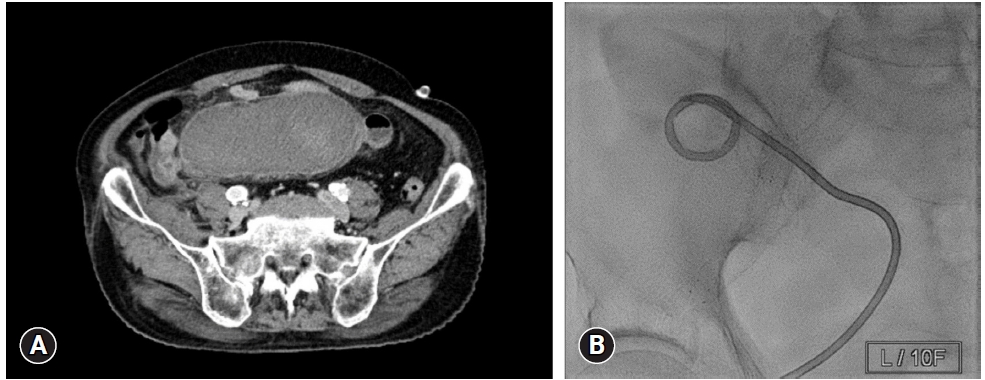
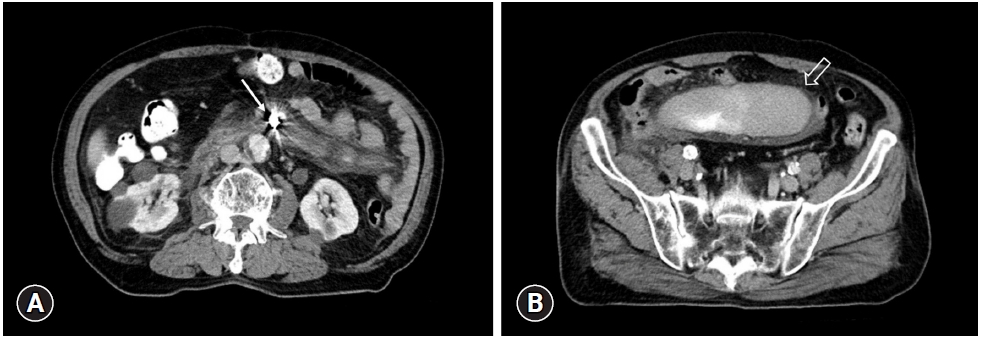
- Abdominal CT on the 4th day of admission showed no active bleeding or pseudoaneurysm-related problems. An increase in hematoma was observed in the mesentery (Fig. 4), but the patient's vital signs were stable and there was no decrease in hemoglobin. Also, no findings such as free air or intestinal ischemia were observed, and findings such as free air or bowel ischemia were not observed. The patient's condition was closely monitored, including periodic abdominal physical examinations. The patient complained of abdominal discomfort despite the absence of fever and leukocytosis, so an abdominal CT was performed on the 13th day of admission. Local fluid collection inside the mesentery was observed on CT, and percutaneous catheter drainage (PCD) was performed (Fig. 5). The patient was discharged on the 23rd day after admission without any complications. Abdominal CT performed at an outpatient department at 3 weeks after PCD showed a significant decrease in fluid, and PCD was removed (Fig. 6).
- Ethics statement
- This study was approved by the Institutional Review Board of Wonkwang University Hospital (No. WKUH 2022-03-028). Written informed consent for publication of the research details and clinical images were obtained from the patient.
CASE REPORT
- Mesenteric injury rarely occurs in blunt abdominal trauma from a traffic accident [1–3]. Despite its low incidence, mesenteric injury can lead to lethal outcomes related to hypovolemic shock due to hemoperitoneum, sepsis due to bowel ischemia, or peritonitis due to perforation [4,5,10]. Therefore, abdominal injury caused by high-energy trauma requires timely diagnosis and treatment. However, delayed diagnosis sometimes occurs because such patients are often accompanied by multiorgan injury or decreased or loss of consciousness due to traumatic brain injury or sedation. In particular, accurate diagnosis may be difficult for patients with unstable vital signs [4,11].
- In this case, we considered the possibility of adhesion around the site of injury in the abdominal cavity because the patient had undergone open abdominal surgery for gastric cancer a year and a half ago. Since the damage is in the proximal part of the SMA, if the adhesions are severe, it is difficult to quickly access the bleeding focus during open surgery, and blood loss may increase. In addition, the patient was taking an antiplatelet drug (clopidogrel) after coronary artery stent insertion due to myocardial infarction. Therefore, additional difficulties related to bleeding control and cardiac complications due to general anesthesia must be considered. Because this patient was hemodynamically stable and showed no CT findings suggestive of bowel ischemia or perforation, it was decided to perform TAE instead of operative management. Successful bleeding control using TAE contributed to reduce the risk of complications associated with general anesthesia and surgery. However, surgery is known as the standard treatment for mesenteric injury, and the implementation of TAE is controversial [9]. In particular, surgery was the only treatment option for cases with intestinal ischemia and perforation or massive bleeding leading to hypovolemic shock [3,6,7,10]. Usually, OM for mesenteric injuries offers the advantage of providing rapid and definitive treatment. However, in the case of patients with a history of open surgery, access to the surgical site may be difficult due to adhesions. In addition, in the case of the elderly, the risk of general anesthesia due to medical history and intraoperative and postoperative side effects due to anticoagulants administration have become problems [8]. Therefore, radiological intervention can be considered as an alternative to surgery for hemorrhage control only in highly selected cases [10,12].
- In addition to HERS, we have a 24/7 radiological intervention team (interventional radiologists and technologists). Therefore, for patients with mesenteric injury who are hemodynamically stable and have no evidence of peritonitis, including bowel ischemia and perforation, nonoperative management with immediate TAE can be performed at HERS instead of moving to the operating room for OM. In HERS, CT scan, interpretation, and angiography can be performed immediately without the need to move the patient. Therefore, it is possible to control bleeding using TAE in highly selected patients, and even if there is a finding that requires surgery, it can act as a bridge through hemostasis during the preparation of the operating room [7,12]. It is difficult to define the indications for NOM or predict the success of NOM for mesenteric injury using CT findings alone, and there are very few case reports of NOM performed for mesenteric injury with active bleeding worldwide [9,13–15]. However, in patients who are hemodynamically stable and have bleeding from the mesenteric artery but no serious bowel injury, as in this case, TAE can be attempted cautiously. Also, even in this case, it is necessary to prepare for surgical treatment in preparation for the possibility of TAE failure. In addition, physical examination, hemodynamic monitoring, and follow-up imaging tests should be repeated after TAE to detect and resolve complications such as rebleeding, bowel ischemia, delayed bowel perforation, and fluid collection [3,9,12]. Above all, careful observation should be performed with the possibility of bowel ischemia always in mind. TAE for SMA may be safer than for inferior mesenteric artery because of the development of collateral vessels. However, TAE for SMA also has the potential to cause ischemia [10,13]. Therefore, close monitoring, physical examination and short-term follow-up CT is needed to confirm bowel ischemia. In our trauma center, the follow-up CT is taken the next day of TAE if bowel ischemia suspected. If air bubbles are observed in the intestinal wall or free air is found on CT, it can be evidence of bowel infarction, so surgical treatment should be performed. Considering the burden of general anesthesia and various intraoperative and postoperative complications, NOM using TAE for mesenteric injury is positive in terms of minimally invasive management. If more cases are accumulated in the future, it is expected that indications for NOM using TAE for mesenteric injury will be established.
DISCUSSION
-
Author contributions
Conceptualization: CYP; Methodology: CYP, SRA, JHL; Project administration: CYP; Visualization: CYP, SRA, SHS; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
Chan Yong Park is an Editorial Board member of the Journal of Trauma and Injury, but was not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
-
Additional information
This study was presented at the 9th Pan-Pacific Trauma Congress in June 2022 in Gyeongju, Korea.
ARTICLE INFORMATION

- 1. Evans S, Talbot E, Hellenthal N, Monie D, Campbell P, Cooper S. Mesenteric vascular injury in trauma: an NTDB Study. Ann Vasc Surg 2021;70:542–8. ArticlePubMed
- 2. Matsushima K, Mangel PS, Schaefer EW, Frankel HL. Blunt hollow viscus and mesenteric injury: still underrecognized. World J Surg 2013;37:759–65. ArticlePubMedPDF
- 3. Bertelli R, Fugazzola P, Zaghi C, et al. Transcatheter arterial embolization in abdominal blunt trauma with active mesenteric bleeding: case series and review of literature. Emerg Radiol 2021;28:55–63. ArticlePubMedPDF
- 4. Durrant E, Abu Mughli R, O’Neill SB, Jiminez-Juan L, Berger FH, Ezra O’Keeffe M. Evaluation of bowel and mesentery in abdominal trauma. Can Assoc Radiol J 2020;71:362–70. ArticlePubMedPDF
- 5. Tilden W, Griffiths M, Cross S. Vascular bowel and mesenteric injury in blunt abdominal trauma: a single centre experience. Clin Radiol 2021;76:213–23. ArticlePubMed
- 6. Okishio Y, Ueda K, Nasu T, Kawashima S, Kunitatsu K, Kato S. Surgical intervention for blunt bowel and mesenteric injury: indications and time intervals. Eur J Trauma Emerg Surg 2021;47:1739–44. ArticlePubMedPDF
- 7. Kakizawa H, Toyota N, Hieda M, et al. Traumatic mesenteric bleeding managed solely with transcatheter embolization. Radiat Med 2007;25:295–8. ArticlePubMedPDF
- 8. Harris M, Chung F. Complications of general anesthesia. Clin Plast Surg 2013;40:503–13. ArticlePubMed
- 9. Bege T, Brunet C, Berdah SV. Hollow viscus injury due to blunt trauma: a review. J Visc Surg 2016;153(4 Suppl):61–8. ArticlePubMed
- 10. Ghelfi J, Frandon J, Barbois S, et al. Arterial embolization in the management of mesenteric bleeding secondary to blunt abdominal trauma. Cardiovasc Intervent Radiol 2016;39:683–9. ArticlePubMedPDF
- 11. Choi Y, Kim S, Ko J, et al. A study on trauma mechanisms and injury sites in patients with blunt abdominal trauma. Emerg Med Int 2022;2022:2160766. ArticlePubMedPMCPDF
- 12. Nakama R, Izawa Y, Kujirai D, et al. Transcatheter arterial embolization for initial hemostasis in a hemodynamically unstable patient with mesenteric hemorrhage: a case report. Radiol Case Rep 2018;14:251–4. ArticlePubMedPMC
- 13. Extrat C, Grange S, Chevalier C, et al. Safety and efficacy of emergency transarterial embolization for mesenteric bleeding. CVIR Endovasc 2022;5:5. ArticlePubMedPMCPDF
- 14. Shin JS, Shin JH, Ko HK, Kim JW, Yoon HK. Transcatheter arterial embolization for traumatic mesenteric bleeding: a 15-year, single-center experience. Diagn Interv Radiol 2016;22:385–9. ArticlePubMedPMC
- 15. Kwon H, Kim CW, Jeon CH, Yeo KH, Noh D, Lee CK. Percutaneous transhepatic embolization for isolated pancreaticoduodenal vein rupture in blunt abdominal trauma: a case report. J Korean Soc Radiol 2017;77:313–6. ArticlePDF
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite