Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Case Report
Three-column reconstruction through the posterior approach alone for the treatment of a severe lumbar burst fracture: a case report -
Woo Seok Kim, MD
 , Tae Seok Jeong, MD
, Tae Seok Jeong, MD , Woo Kyung Kim, MD
, Woo Kyung Kim, MD
-
Journal of Trauma and Injury 2023;36(3):290-294.
DOI: https://doi.org/10.20408/jti.2022.0075
Published online: June 9, 2023
- 743 Views
- 24 Download
Department of Traumatology, Gachon University Gil Medical Center, Incheon, Korea
- Correspondence to Woo Seok Kim, MD Department of Traumatology, Gachon University Gil Medical Center, 21 Namdong-daero 774beon-gil, Namdong-gu, Incheon 21565, Korea Tel: +82-32-460-3010 Email: nskws0603@gilhospital.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Generally, patients with severe burst fractures, instability, or neurological deficits require surgical treatment. In most cases, circumferential reconstruction is performed. Surgical methods for three-column reconstruction include anterior, lateral, and posterior approaches. In cases involving an anterior or lateral approach, collaboration with general or thoracic surgeons may be necessary because the adjacent anatomical structures are unfamiliar to spinal surgeons. Risks include vascular or lumbar plexus injuries and cage displacement, and in most cases, additional posterior fusion surgery is required. However, the posterior approach is the most common and anatomically familiar approach for surgeons performing spinal surgery. We present a case in which three-column reconstruction was performed using only the posterior approach to treat a patient with a severe lumbar burst fracture.
- Burst fractures of the thoracolumbar spine are usually caused by high-energy traumas, such as traffic accidents and falls [1,2]. These fractures may result in severe neurological deficits or spinal instabilities. Regardless of their neurological effects, unstable burst fractures require surgical intervention. Spinal surgeons have a variety of surgical options, including the posterior, anterior, and lateral approaches [1–6]. Because each approach has its advantages and disadvantages, there is no consensus regarding the ideal method. To select an appropriate approach, the surgeon must consider the degree of deformity, any neurological damage, and the surrounding anatomy. We describe a case in which three-column reconstruction was performed by inserting an expandable cage and transpedicular screw fixation after corpectomy through a single posterior approach in a patient with a burst fracture of the third lumbar vertebra and severe bodily deformity.
INTRODUCTION
- A 55-year-old man was admitted to Gachon University Gil Medical Center for pain in both lower extremities and the lower back, that occurred after he had fallen from the 10th story of a building. He was on medication for diabetes mellitus and major depressive disorder and had a history of surgery for a left femur fracture. Because the patient presented with right femoral subtrochanteric, left femoral shaft, and left proximal fibula fractures with accompanying damage, it was difficult to evaluate the lower extremity motor score accurately during a physical examination, but the sensory function was intact. However, sensation around the perineum was somewhat reduced, and anal tone was diminished. A severe burst fracture of the third lumbar vertebra was confirmed on whole-body computed tomography (CT) performed in the emergency department. Other injuries included a Jefferson fracture, a compression fracture of the fifth thoracic vertebra, multiple transverse process fractures, multiple spinous process fractures, right radioulnar midshaft fractures, a right proximal humerus fracture, a right scapula glenoid fracture, a left first metacarpal base fracture, and liver injuries.
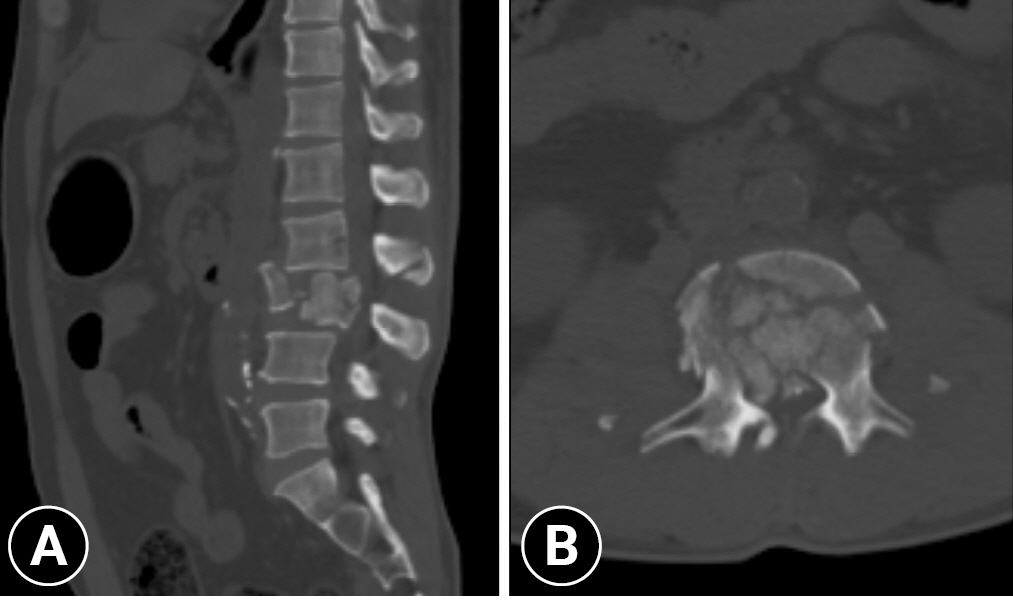
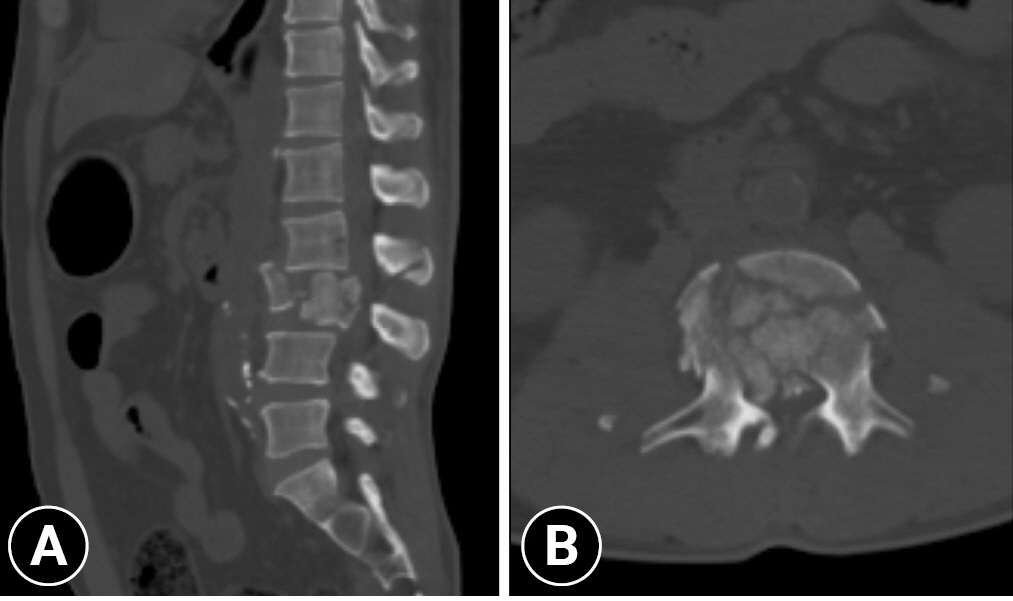
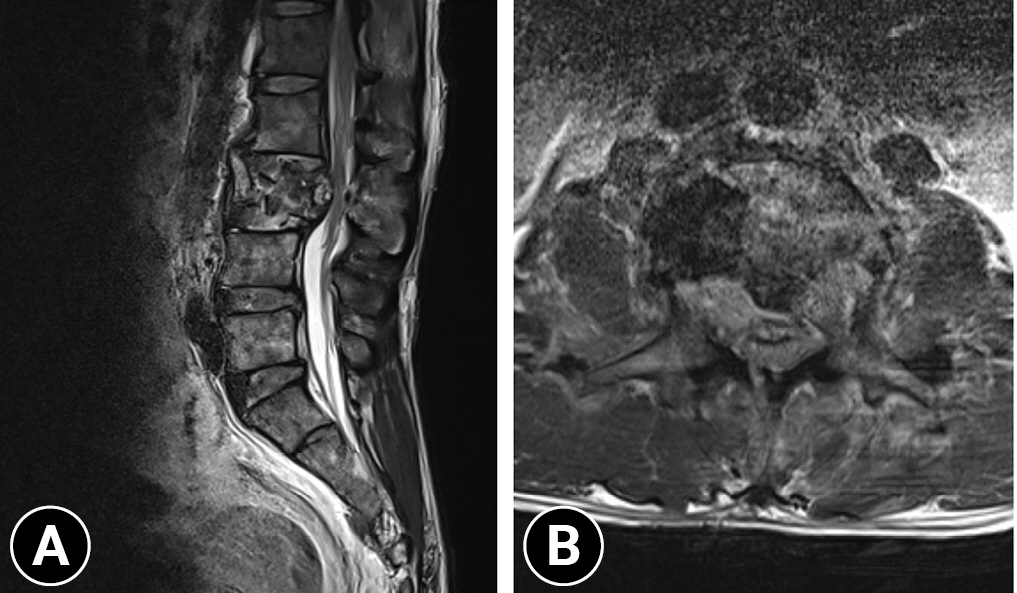
- Abdominopelvic CT findings showed that the burst fracture of the third lumbar vertebra was very severe, resulting in severe dural sac compression. In addition, a posterior ligament complex injury was suspected because it was accompanied by a fracture of the second lumbar spinous process (Fig. 1). Active bleeding due to liver injury was observed; therefore, hepatic artery embolization was performed. Next, bilateral traction procedures were performed for both femur fractures by orthopedic surgeons in the intensive care unit. After stabilization of the vital signs, spinal magnetic resonance imaging (MRI) was performed on the sixth day of hospitalization. Findings similar to those observed on CT were confirmed by the lumbar spine MRI (Fig. 2), and surgery was performed the following day. We selected the posterior surgical approach for the following reasons. First, the operator felt concerned because he had little experience with the lateral approach. Second, we concluded that it would be difficult to maintain a lateral position due to the traction pins applied to both proximal tibias to stabilize the bilateral femoral fractures. Third, the Jefferson fracture was an anterior arch fracture without ligament injury. In addition, the general surgery department confirmed that it would be possible to perform surgery in the prone position despite the patient’s liver injury.
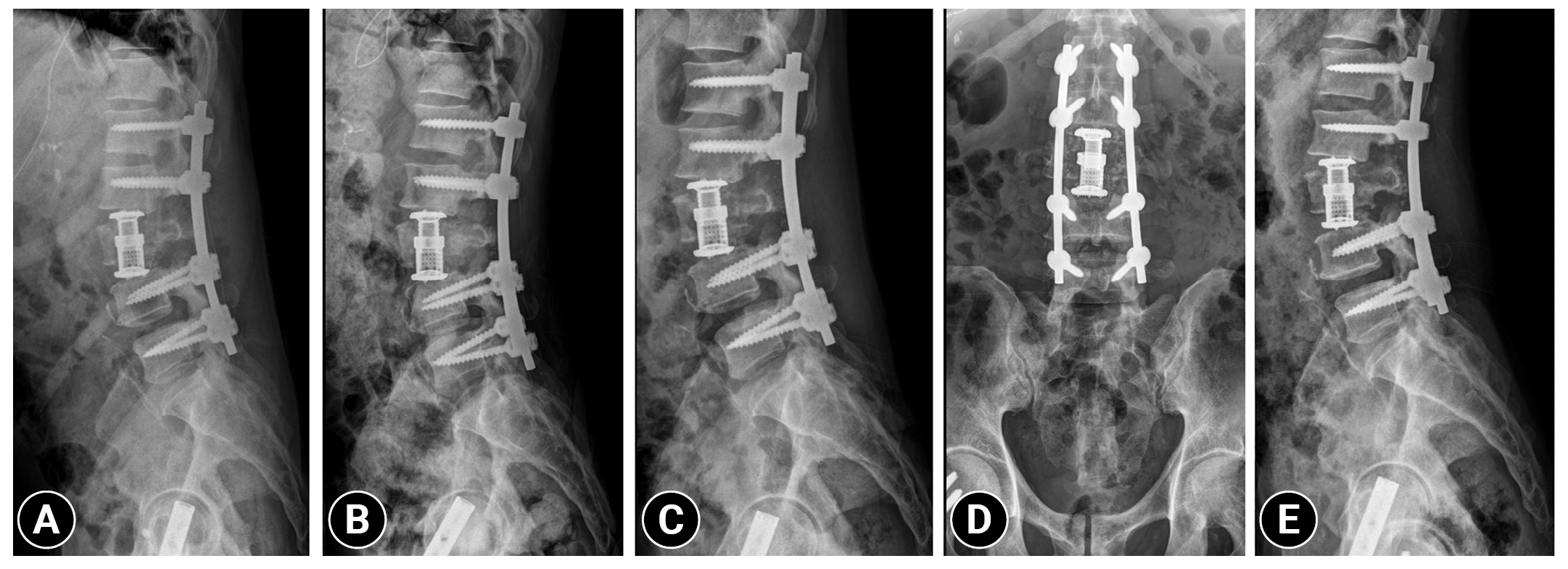
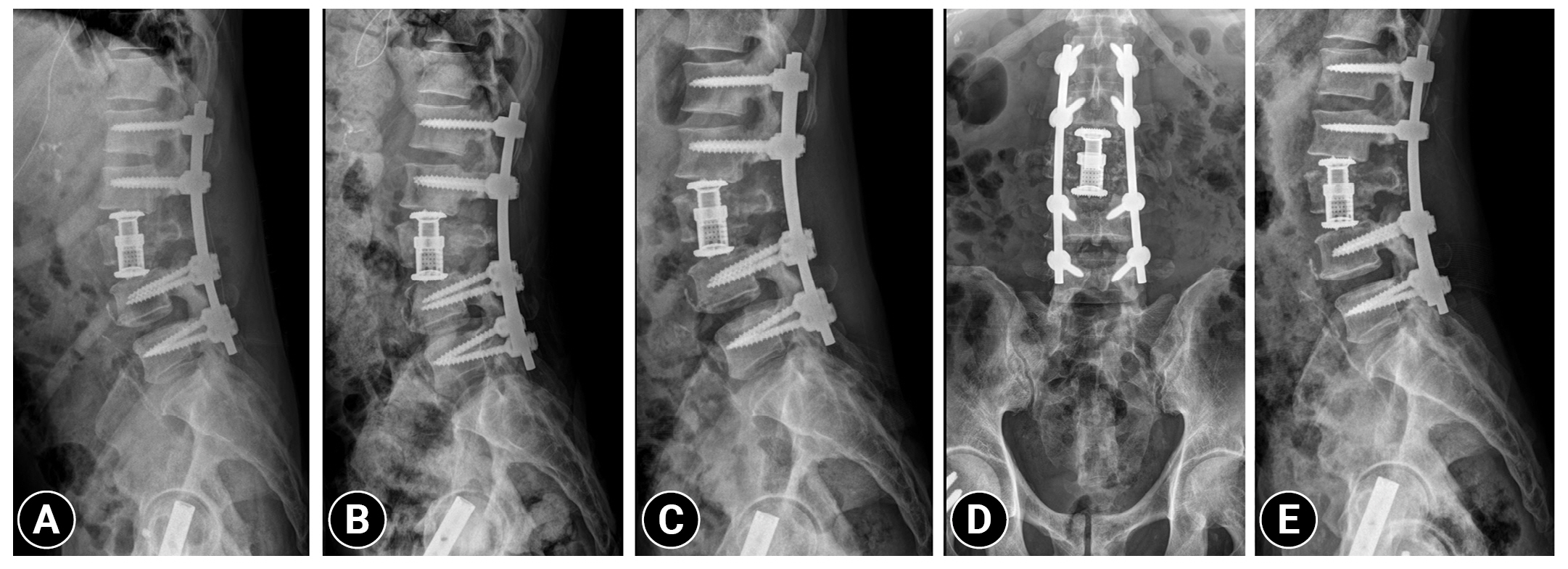
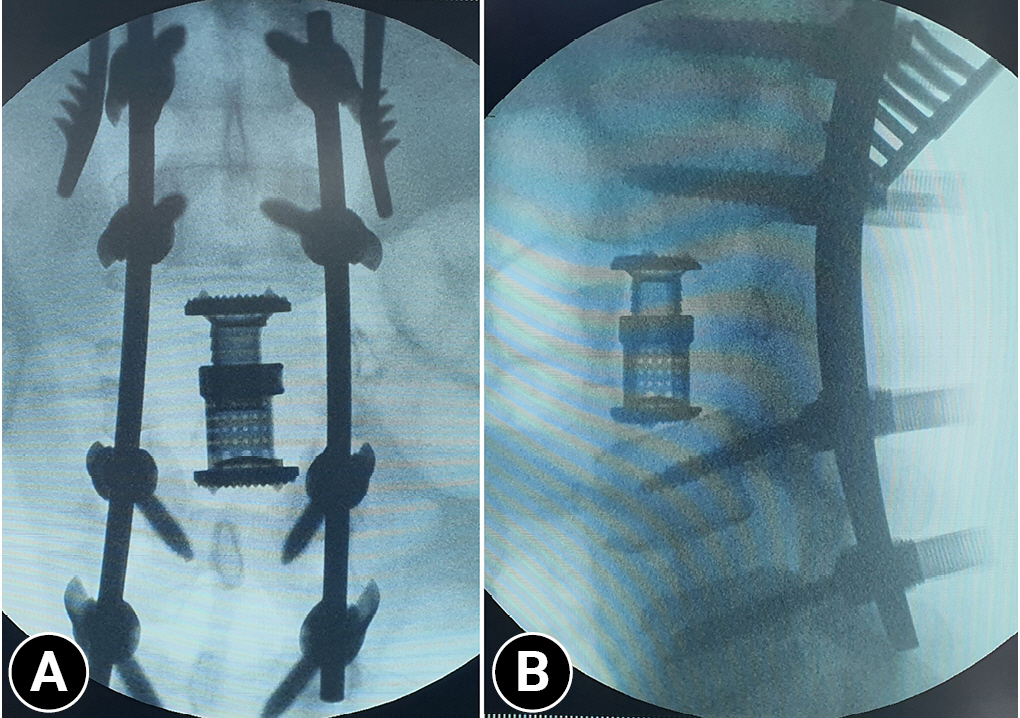
- In the preoperative neurological examination, movements of both hip and knee joints were difficult to examine due to traction. The motion scores of both ankle dorsiflexors, long toe extensors, and ankle plantar flexors were all poor. Sensation in both lower extremities was intact except around the perineum. Surgery was performed under general anesthesia. A midline skin incision was made in the prone position, and periosteal dissection was performed to expose the lamina from the 11th thoracic to the first sacral vertebra. Pedicle screws were inserted into the first, second, fourth, and fifth lumbar vertebrae under fluoroscopic guidance. After screw insertion, total laminectomy of the third lumbar vertebral and partial laminectomy of the second lumbar vertebra were performed using a high-speed drill and laminectomy punch. Thereafter, both pedicles of the third lumbar vertebra were removed to ensure sufficient space for the corpectomy and cage insertion. Both spinal nerves of the third lumbar vertebra passing through the intervertebral foramen were subsequently exposed. Removal of both pedicles and exposure of both spinal nerves provided an adequate field of view and space to perform the corpectomy. Total disc resections were performed between the second and third lumbar vertebrae, and between the third and fourth lumbar vertebrae. While close attention was paid to the spinal nerves, the vertebral body was removed using a drill, pituitary rongeurs, and a laminectomy punch. During surgery, we dissected the spinal nerves using a nerve hook and curettes and checked for sufficient decompression. To prevent the cage from being displaced anteriorly, an additional corpectomy was performed, leaving the anterior longitudinal ligament and anterior portion of the vertebral body. When corpectomy had been performed to accommodate the cage, the expandable cage was carefully inserted and expanded while we protected the spinal nerves and dural sac. Subsequently, the rods were bent to create a lordotic curve and the space between the second and fourth lumbar vertebrae was compressed and fixed. Then, meticulous bleeding control was performed, drainage tubes were inserted, and surgery was completed using layer-by-layer sutures (Fig. 3). The findings of the neurological examination performed immediately after surgery were not significantly different from the findings of the examination performed preoperatively.
- The patient received appropriate treatment for the accompanying injuries, was transferred to a rehabilitation hospital on the 61st day of admission and had subsequent follow-up on an outpatient basis. After being transferred, the patient did not receive appropriate rehabilitation because he was confirmed to be positive for carbapenemase-producing Enterobacteriaceae at the hospital and was isolated. When the patient visited the outpatient clinic 6 months after spine surgery, he was able to stand unassisted, but his ambulation was limited because of bilateral foot drop. In both legs, the foot drops were due to peroneal nerve injury, and the patient was receiving orthopedic follow-up. Both hip flexors were assessed as fair. Both knee extensors, ankle dorsiflexors, long toe extensors, and ankle plantar flexors were assessed as poor. The patient complained of hypoesthesia along the sensory distribution of both peroneal nerves, especially on the left side. In addition, he still had difficulty voiding. Lumbar spine radiographs taken immediately after surgery, 1 month, 3 months, and 6 months after surgery showed that the expandable cage and screws were well maintained without instability (Fig. 4).
- Ethics statement
- This study was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GDIRB2022-190). Written informed consent for publication of the research details and clinical images were obtained from the patient.
CASE REPORT
- Circumferential reconstruction of the thoracolumbar spine can be achieved by combining anterior and posterior approaches, or lateral and posterior approaches. These anterior and lateral approaches show high fusion rates and can correct sagittal deformities [1,5]. They allow direct corpectomy, facilitate cage placement, and allow plating to be performed [7]. Despite these advantages, the anterior and lateral approaches have several disadvantages. The most important point to consider in the anterior approach is the possibility of damage to blood vessels (2%–15%); large blood vessels such as the aorta, common iliac artery, and inferior vena cava may be damaged during the process of exposing the vertebral body [8–10]. In addition, complications such as ureteral injury, hypogastric plexus injury, and incisional hernia may occur [11]. In the lateral approach, the lumbar and sympathetic plexuses may be injured during traction of the psoas muscle and exposure of the vertebral body. Intraoperative monitoring devices are needed to avoid these risks [8,12]. In the lower lumbar level, access via lateral approach is sometimes challenging because of the iliac crest [11]. Additional posterior support is required in the anterior and lateral approaches, as there is a risk of displacement of the inserted cage [8].
- The single-stage posterior approach has been successfully used for circumferential decompression and reconstruction of thoracolumbar tumors [13]. However, it has several limitations. First, long-segment fixation is required to provide adequate stability [14]. There is also a risk of lower fusion rates owing to the inability to insert a larger cage, unlike the anterior and lateral approaches [6]. Meanwhile, the single-stage posterior approach also has several advantages. First, it is the most widely used technique because it is anatomically familiar to surgeons performing spinal surgery [8]. Second, it eliminates the risks of vascular or lumbar plexus injury [8–10,12]. In addition, since only one approach is used, it can promote anterior and posterior fixation, and it has the advantage of preventing cage displacement by preserving the anterior longitudinal ligament and the anterior part of the vertebral body [8,13].
- As mentioned above, there are various surgical approaches for the treatment of burst fractures of the thoracolumbar spine. This case demonstrates that the posterior approach alone is sufficient for corpectomy and fusion. In a variety of cases, such as when collaboration with general or thoracic surgeons is not feasible or when equipment such as an intraoperative monitoring device is not available, the single-stage posterior approach may be an excellent option.
DISCUSSION
-
Author contributions
Conceptualization: TSJ, WKK; Data curation: WSK; Formal analysis: WSK; Investigation: WSK; Methodology: WSK; Project administration: WSK; Supervision: TSJ, WKK; Visualization: TSJ, WKK; Writing–original draft: WSK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION
- 1. Dai LY, Jiang LS, Jiang SD. Anterior-only stabilization using plating with bone structural autograft versus titanium mesh cages for two- or three-column thoracolumbar burst fractures: a prospective randomized study. Spine (Phila Pa 1976) 2009;34:1429–35. PubMed
- 2. Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J 2014;14:145–64. ArticlePubMed
- 3. Adkins DE, Sandhu FA, Voyadzis JM. Minimally invasive lateral approach to the thoracolumbar junction for corpectomy. J Clin Neurosci 2013;20:1289–94. ArticlePubMed
- 4. Heary RF, Kumar S. Decision-making in burst fractures of the thoracolumbar and lumbar spine. Indian J Orthop 2007;41:268–76. ArticlePubMedPMC
- 5. McDonough PW, Davis R, Tribus C, Zdeblick TA. The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine (Phila Pa 1976) 2004;29:1901–9. ArticlePubMed
- 6. Heary RF, Kheterpal A, Mammis A, Kumar S. Stackable carbon fiber cages for thoracolumbar interbody fusion after corpectomy: long-term outcome analysis. Neurosurgery 2011;68:810–9. ArticlePubMedPDF
- 7. Schnake KJ, Stavridis SI, Krampe S, Kandziora F. Additional anterior plating enhances fusion in anteroposteriorly stabilized thoracolumbar fractures. Injury 2014;45:792–8. ArticlePubMed
- 8. Ayberk G, Ozveren MF, Altundal N, et al. Three column stabilization through posterior approach alone: transpedicular placement of distractable cage with transpedicular screw fixation. Neurol Med Chir (Tokyo) 2008;48:8–14. ArticlePubMed
- 9. Brau SA, Delamarter RB, Schiffman ML, Williams LA, Watkins RG. Vascular injury during anterior lumbar surgery. Spine J 2004;4:409–12. PubMed
- 10. Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr. Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine (Phila Pa 1976) 2007;32:2751–8. PubMed
- 11. Talia AJ, Wong ML, Lau HC, Kaye AH. Comparison of the different surgical approaches for lumbar interbody fusion. J Clin Neurosci 2015;22:243–51. ArticlePubMed
- 12. Alluri R, Mok JK, Vaishnav A, et al. Intraoperative neuromonitoring during lateral lumbar interbody fusion. Neurospine 2021;18:430–6. ArticlePubMedPMCPDF
- 13. Metcalfe S, Gbejuade H, Patel NR. The posterior transpedicular approach for circumferential decompression and instrumented stabilization with titanium cage vertebrectomy reconstruction for spinal tumors: consecutive case series of 50 patients. Spine (Phila Pa 1976) 2012;37:1375–83. PubMed
- 14. Peters T, Chinthakunta SR, Hussain M, Khalil S. Pedicle screw configuration for thoracolumbar burst fracture treatment: short versus long posterior fixation constructs with and without anterior column augmentation. Asian Spine J 2014;8:35–43. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite