Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(1); 2022 > Article
-
Case Report
Delayed bladder perforation due to screw loosening after pelvic ring injury surgery: a case report -
Hyun-Chul Shon, MD1
 , Ho-Won Kang, MD2
, Ho-Won Kang, MD2 , Eic-Ju Lim, MD1
, Eic-Ju Lim, MD1 , Jae-Young Yang, MD1
, Jae-Young Yang, MD1
-
Journal of Trauma and Injury 2022;35(1):51-55.
DOI: https://doi.org/10.20408/jti.2021.0054
Published online: December 22, 2021
- 2,400 Views
- 85 Download
1Department of Orthopaedic Surgery, Chungbuk National University Hospital, Cheongju, Korea
2Department of Urology, Chungbuk National University Hospital, Cheongju, Korea
- Correspondence to Jae-Young Yang, MD Department of Orthopaedic Surgery, Chungbuk National University Hospital, 776 1sunhwan-ro, Seowon-gu, Cheongju 28644, Korea Tel: +82-43-269-7852 E-mail: hahayourdead@naver.com
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Pelvic ring injuries have high mortality and morbidity rates, and they are difficult to treat because accompanying injuries to the pelvic organs, genitourinary organs, and neurovascular tissues are common. Genitourinary injuries are common comorbid injuries that have been reported to occur in 5% to 6% of all pelvic ring injuries. However, these injuries usually occur simultaneously with the pelvic ring injury, whereas relatively little research has dealt with genitourinary injuries that occur after treatment of a pelvic ring injury. To the best of our knowledge, only three cases of delayed bladder perforation due to screw loosening after symphyseal plate fixation in anterior pelvic ring injury have been reported worldwide, and no such cases have yet been reported in Korea. Since the authors experienced this very rare complication after pelvic ring surgery, we report this case along with a literature review.
- Concomitant bladder injuries have been reported to occur in 5% to 6% of pelvic ring injuries [1]; these two injuries usually occur simultaneously. However, relatively little research has investigated delayed genitourinary complications that occur late after surgery. A symphyseal plate is commonly used as a fixation method for anterior pelvic ring injuries. Because it is fixed across the joint, micro-movement occurs, and metal plate breakage or screw loosening is common. To the best of our knowledge, only three cases of bladder perforation due to screw loosening have been reported worldwide [2-4]. Moreover, delayed bladder perforation due to screw loosening after fixation of the symphyseal plate has not been reported in Korea. In this study, we report a case of delayed bladder perforation due to screw loosening after anterior pelvic ring surgery using a symphyseal plate along with a literature review.
INTRODUCTION
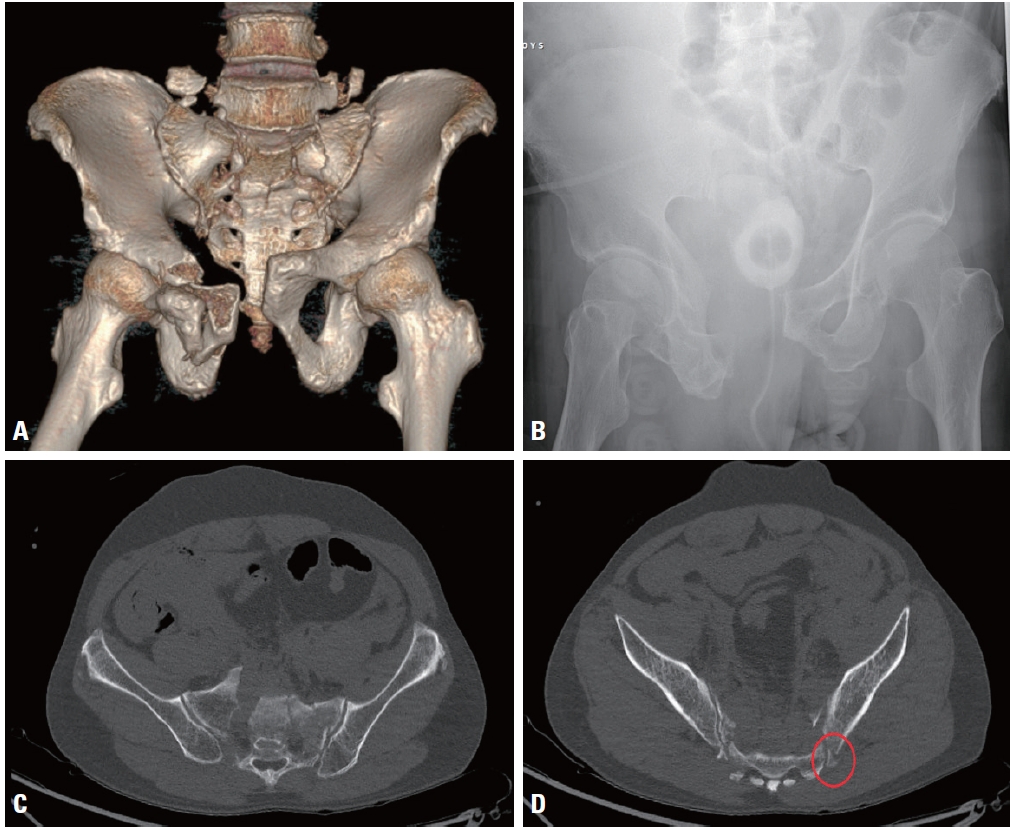
- A 64-year-old male patient was presented to the emergency room after a motorcycle accident. Abdominal pelvic computed tomography showed symphysis pubis diastasis, right superior and inferior ramus fractures, and bilateral anterior and posterior sacroiliac joint injuries (Fig. 1), which corresponded to an anterior posterior compression type III pelvic ring injury. In addition, there was extravasation of the right internal iliac artery branch with hypotension; therefore, emergency angioembolization was performed. Immediately after embolization, orthopedic damage control surgery (supracetabular external fixation) was performed. A Schanz screw was inserted into the supra-acetabular area. The right sacrum, which was more displaced than the left, was reduced using a Schanz screw as a joystick, and a sacroiliac screw was inserted. An external fixation device was then connected.
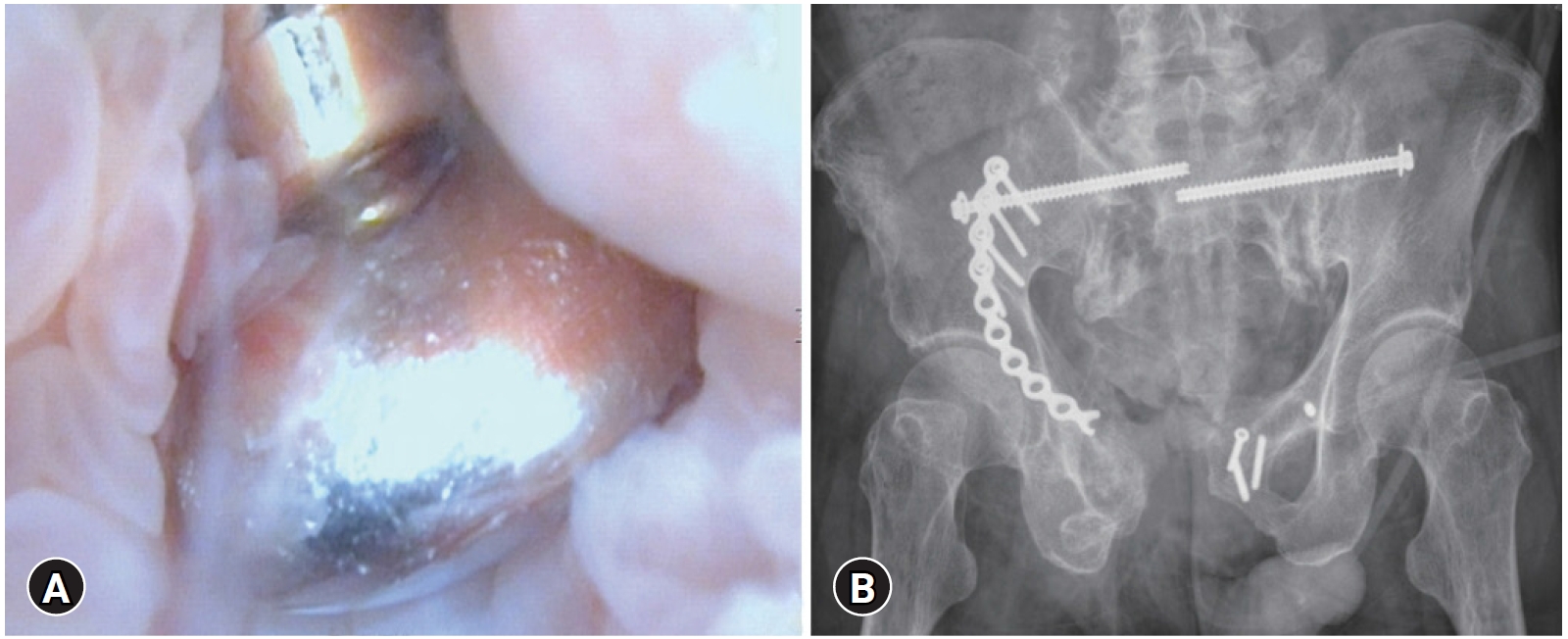
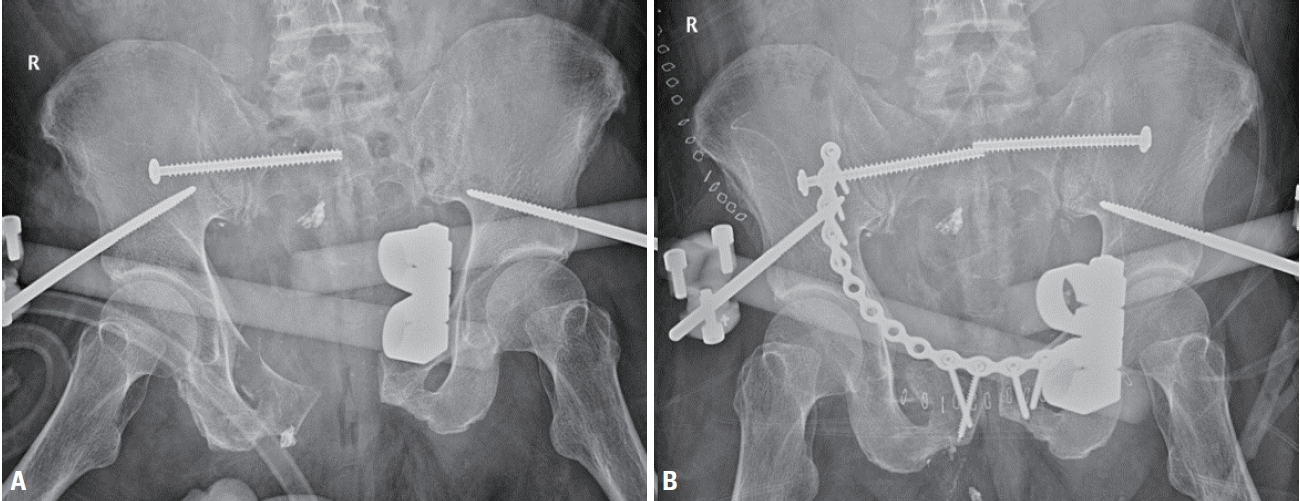
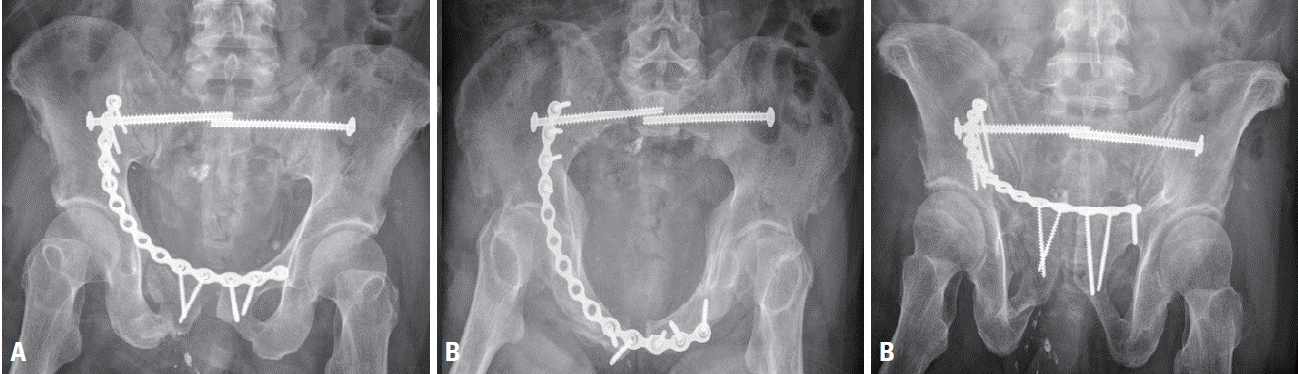
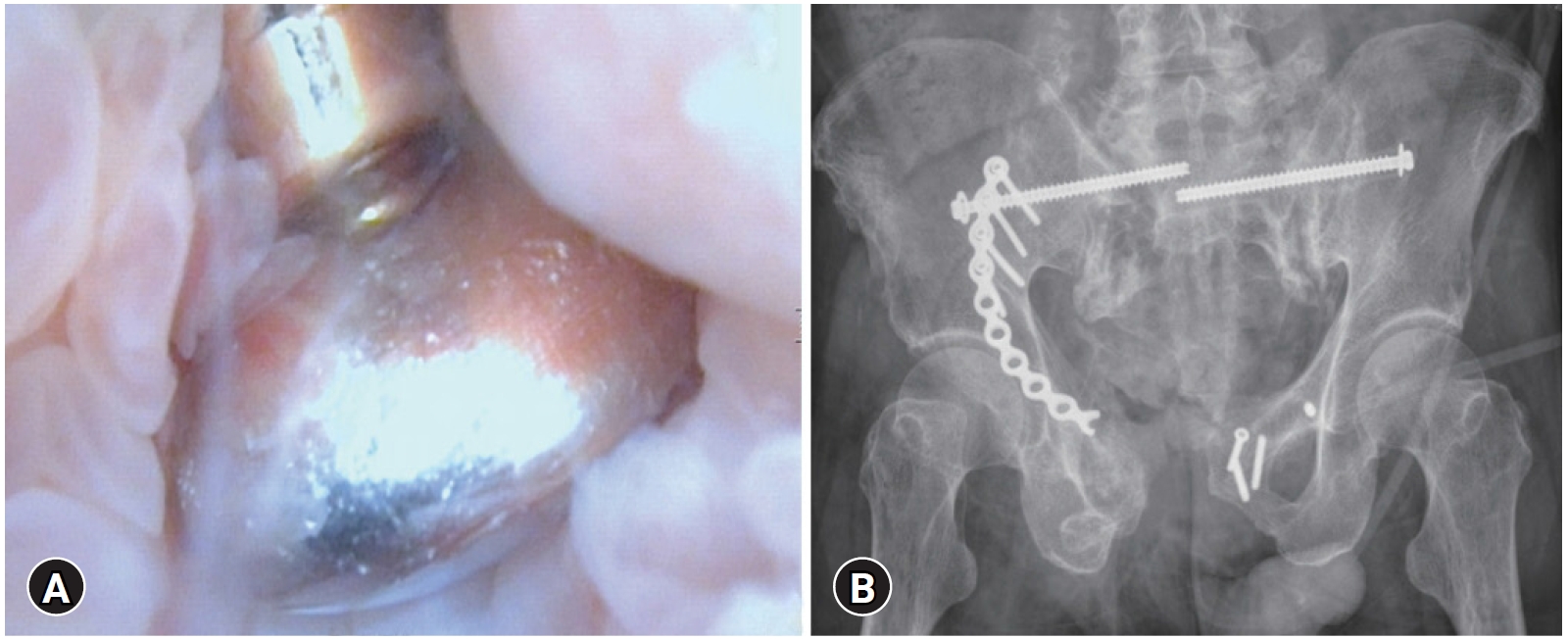
- The patient was hemodynamically stabilized, and definitive orthopedic surgery was performed on the 8th day after the injury. Under general anesthesia, the patient was placed in a supine position on a radiolucent table. A sacroiliac screw (7.3 mm cannulated cancellous screw; DePuy Synthes, Raynham, MA, USA) was inserted into the left sacrum. The fracture site was exposed using a modified Stoppa approach. The pubic diastasis was reduced using a bone clamp, and the ramus fracture was naturally reduced due to ligamentotaxis. Fixation was then performed using a symphyseal plate (Matta pelvic plate; Stryker, San Jose, CA, USA). Although there is no significant difference between a conventional plate and a locking plate [5], a conventional plate was used because we assumed that plate breakage was more likely to occur with a locking plate due to the micro-motion of the symphysis pubis. As pubic symphysis diastasis accompanied the ramus fracture, it was fixed with a 14-hole symphyseal plate to obtain sufficient fixation force. The proximal screws were fixed to the ilium through the lateral window (Fig. 2). The external fixator was removed 6 weeks after surgery (Fig. 3) and partial weight-bearing using a walker was started. Loosening of the screw was observed 6 months after surgery, screw breakage and additional loosening were observed 8 months after surgery, and plate breakage was observed 1 year and 5 months after surgery (Fig. 4), but the patient did not complain of any discomfort and was able to walk independently. Hematuria and dysuria occurred 1 year and 10 months after surgery, and the patient visited the urology department. Cystoscopy revealed a screw head. Therefore, after 1 week, under general anesthesia, implant removal and partial cystectomy were performed by an orthopedic surgeon and urology surgeon (Fig. 5). During the procedure, it was found that the symphysis pubis and the bladder were adhered, and an inflammatory reaction was observed. After surgery, hematuria improved, and the patient was able to walk independently.
CASE REPORT
- To the best of our knowledge, only three cases of delayed bladder perforation due to orthopedic implants after pelvic ring injury have been reported worldwide, and this is the first reported case in Korea.
- Fridman et al. [2] previously reported a patient with spontaneous voiding of an implant after fixation of the pubic symphysis, which was similar to our case. In the case of Peled et al. [4], there was a bladder injury at the time of injury; therefore, the possibility that the screw entered the injured area could not be excluded. Hosseini et al. [3] also reported a case of delayed bladder perforation due to screw loosening 7 weeks after pelvic surgery, which was treated with cystoscopic screw removal. Unlike the above cases, our case was accompanied by breakage of the symphyseal plate and loosening of the screw, and the presence of a screw in the bladder was confirmed by a cystoscope. Using the previous incision, the broken plate and screws were removed, and the bladder was repaired.
- The pubic symphysis is a fibrous joint that connects the pubis, and micromotion occurs during walking. Therefore, when a symphyseal plate is fixed to the anterior pelvic ring, screw loosening, screw breakage, and plate breakage are common [6]. In addition, in this case, a long plate was used because of the diastasis and pubic ramus fracture that caused the unbalanced fixation and likely promoted screw loosening and breakage of the plate. Therefore, we suggest using a 2- or 4-hole-longer plate on the left side to balance the fixation and a dual plate or a ramus screw to increase the strength of fixation.
- Although clear timing and indications for symphyseal plate removal have not been established [7], in our case, it is thought that bladder perforation could have been avoided if the plate had been removed at an early stage when screw loosening was observed.
- According to the European Association of Urology guidelines [8], hematuria, dysuria, and recurrent urinary tract infections (UTIs) have been suggested as symptoms of unrecognized bladder injury. Kaldenbach and Roth [9] reported hematuria and pain as the main symptoms of delayed bladder injury, which are similar to the symptoms of lower UTIs. The patients in the present case and those in the three cases described above complained of hematuria and dysuria. Therefore, if urinary symptoms appear after orthopedic pelvic surgery, it is necessary to pay close attention to the diagnosis rather than dismiss it as a simple lower UTI.
- We report the rare complication of delayed bladder perforation after pelvic ring surgery using a symphyseal plate and suggest that if screw loosening is observed, attention should be paid to urinary symptoms.
DISCUSSION
-
Ethical statement
Informed consent was obtained from the patient.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: HYS; Project administration: JYY; Data curation: JYY, HWK, EJL; Investigation: HYS, JYY, HWK, EJL; Supervision: HYS, JYY, HWK, EJL; Validation : HYS, JYY, HWK, EJL; Writing–original draft: JYY; Writing–review&editing: HYS, JYY, HWK, EJL.
All authors read and approved the final copy of the manuscript.
ARTICLE INFORMATION


- 1. Eid AM. Early urinary complications of fractures of the pelvis. Arch Orthop Trauma Surg 1982;100:99–106. ArticlePubMed
- 2. Fridman M, Glass AM, Noronha JA, Carvalhal EF, Martini RK. Spontaneous urinary voiding of a metallic implant after operative fixation of the pubic symphysis: a case report. J Bone Joint Surg Am 2003;85:1129–32. PubMed
- 3. Hosseini SR, Rezaei H, Mohseni MG, Ganjali H, Behtash N, Arzani M. Screw as a bladder foreign body. Urol Case Rep 2017;11:69–70. ArticlePubMedPMC
- 4. Peled E, Norman D, Kakiashvili D, Henley MB. Recurrent episodes of micturition with expulsion of symphyseal plate screws following pelvic ring fixation: case report. BMC Musculoskelet Disord 2015;16:127. ArticlePubMedPMC
- 5. Grimshaw CS, Bledsoe JG, Moed BR. Locked versus standard unlocked plating of the pubic symphysis: a cadaver biomechanical study. J Orthop Trauma 2012;26:402–6. PubMed
- 6. Eastman JG, Krieg JC, Routt ML Jr. Early failure of symphysis pubis plating. Injury 2016;47:1707–12. ArticlePubMed
- 7. Giannoudis PV, Chalidis BE, Roberts CS. Internal fixation of traumatic diastasis of pubic symphysis: is plate removal essential? Arch Orthop Trauma Surg 2008;128:325–31. ArticlePubMed
- 8. Summerton DJ, Kitrey ND, Lumen N, Serafetinidis E, Djakovic N, European Association of Urology. EAU guidelines on iatrogenic trauma. Eur Urol 2012;62:628–39. ArticlePubMed
- 9. Kaldenbach U, Roth S. Bladder wall injury consequent to total hip replacement: delayed presentation. Int J Urol 2006;13:1003–4. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite