Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(1); 2022 > Article
-
Case Report
Dual repair of traumatic flank hernia using laparoscopic and open approaches: a case report -
Yoonjung Heo, MD1,2
 , Dong Hun Kim, MD2
, Dong Hun Kim, MD2
-
Journal of Trauma and Injury 2022;35(1):46-50.
DOI: https://doi.org/10.20408/jti.2021.0008
Published online: October 25, 2021
- 4,306 Views
- 98 Download
1Department of Medicine, Dankook University Graduate School, Cheonan, Korea
2Department of Trauma Surgery, Trauma Center, Dankook University Hospital, Cheonan, Korea
- Correspondence to Dong Hun Kim, MD Department of Trauma Surgery, Trauma Center, Dankook University Hospital, 201 Manghyang-ro, Dongnam-gu, Cheonan 31116, Korea Tel: +82-41-550-3042 E-mail: saint7331@gmail.com
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Traumatic flank hernia (TFH) is rare and prone to recurrence, which makes appropriate treatment challenging. No current guidelines define the optimal timing and method of repair. Meanwhile, recent advances in laparoscopic techniques are reshaping the options for the treatment of TFH. A dual approach that utilizes both laparoscopic and open methods has not previously been reported. Herein, we present the successful treatment of TFH after blunt trauma. A 46-year-old male patient underwent elective herniorrhaphy on hospital day 3, in which laparoscopic implantation of a sublay mesh and extracorporeal implantation of an onlay mesh were performed. Such techniques may be appropriate and result in feasible outcomes in hemodynamically stable patients with large TFH who are strongly suspected of having bowel herniation or concomitant intraperitoneal injuries. Larger studies are needed to assess the long-term results.
- Traumatic abdominal wall hernia (TAWH) is a relatively rare injury, accounting for only 1% of all blunt trauma admissions [1]. Traumatic flank hernia (TFH) is the most common type of these injuries [2], but trauma surgeons are not familiar with TFH, which frequently leads to misdiagnosis and delayed treatment [3]. Thus, the investigation of flank hernia with an abdominopelvic computed tomography scan is recommended when patients have high-energy blunt trauma to the torso, even in the absence of symptoms. TFH is best managed by a timely operative intervention in a patient with incarceration or strangulation [4,5]. However, the repair is complicated when the defect is large and involves all layers of the abdominal wall. Furthermore, to date, no well-defined guidelines exist on the optimal management strategy for these injuries. Herein, we describe the first successful treatment of TFH after blunt trauma using laparoscopic and open approaches with a dual tension-free repair method to maximize the strength of the herniorrhaphy.
INTRODUCTION
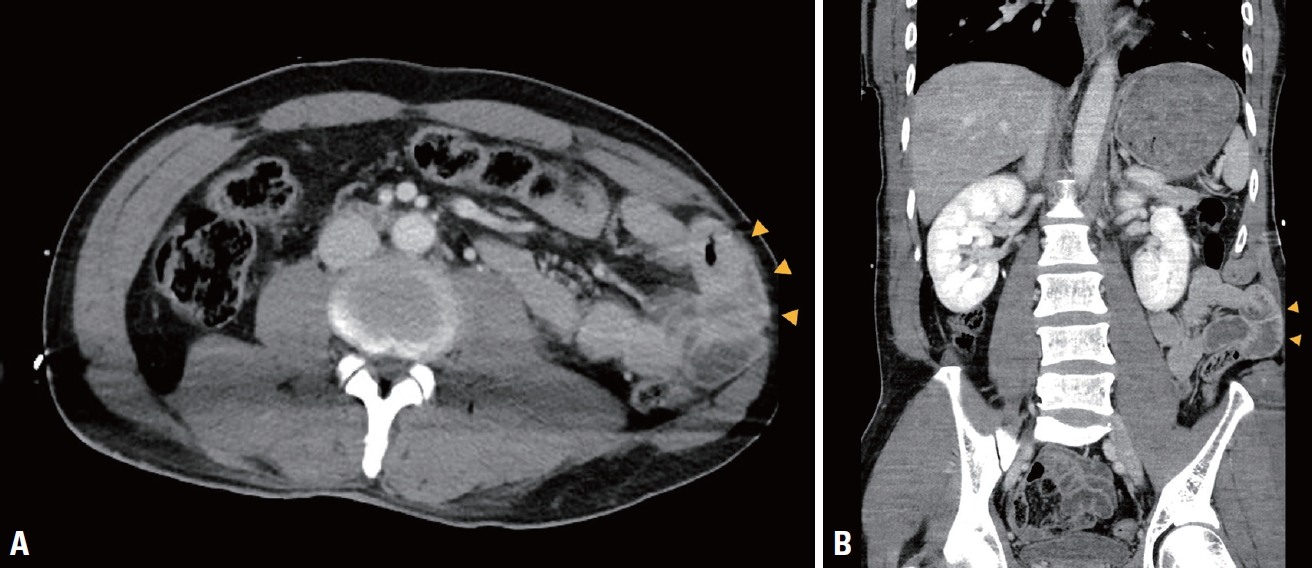
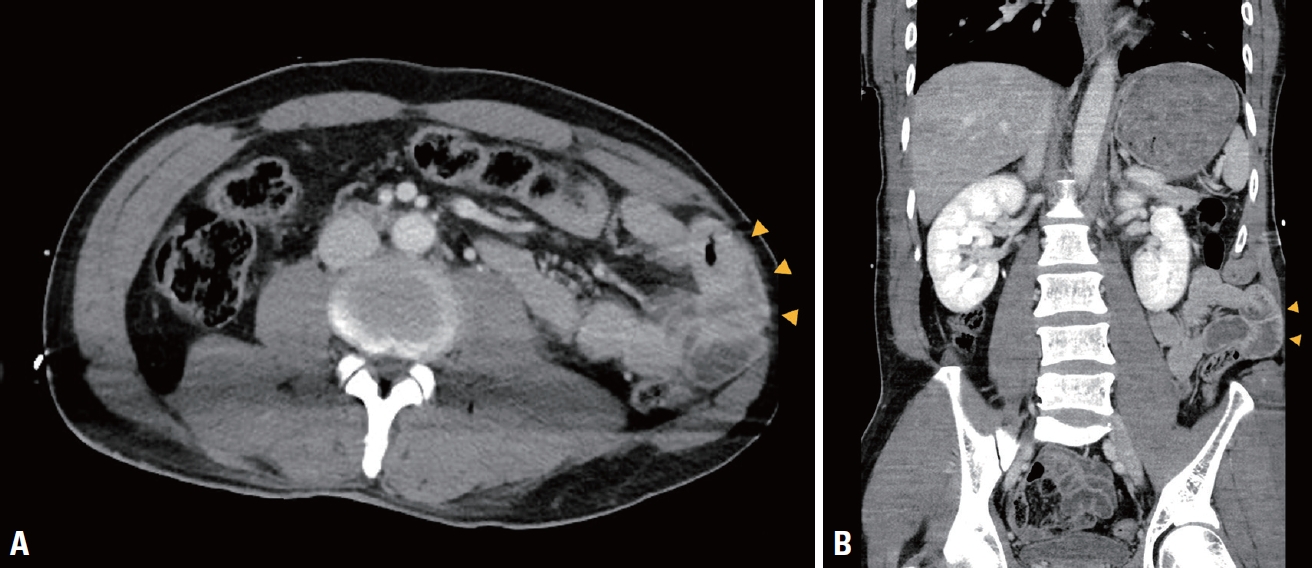
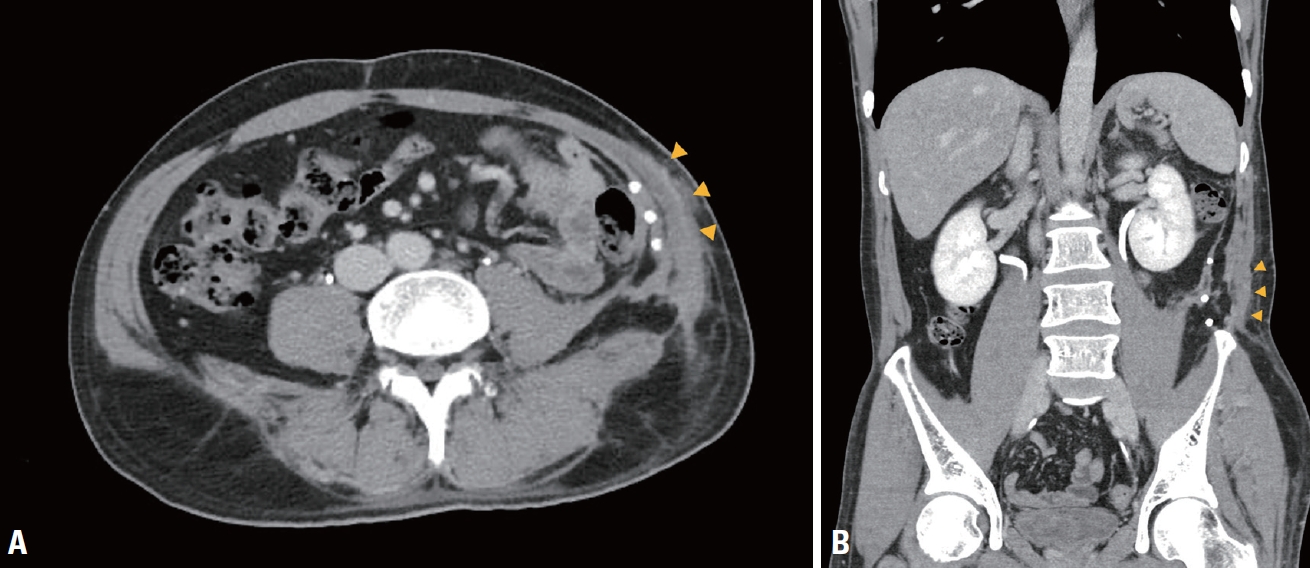
- A 46-year-old male patient whose right-sided torso had been sandwiched between industrial pressers presented to the emergency department of Dankook University Hospital. Upon admission, the patient’s hemodynamics were stable. Upon physical examination, the peritoneal irritation sign with muscle guarding was positive. The patient had a minor laceration of the right chest wall and abdominal bulging with multiple abrasions in the left flank (Fig. 1). An abdominopelvic computed tomography scan showed multiple rib fractures, fractures of the transverse and spinous processes of multiple lumbar vertebrae, multiple ruptured discs in the lumbar spine, and complete abdominal wall disruption (65×83 mm) with herniation of the small bowel in the left flank (Fig. 2). No definite associated injuries of the intra-abdominal organs were found. The patient’s Injury Severity Score was 17. Even though there were no other life-threatening injuries, surgery could no longer be delayed as the peritoneal irritation sign increased over time. Herniorrhaphy was performed immediately on hospital day 3 with a laparoscopic specialist in attendance.
- Surgical technique
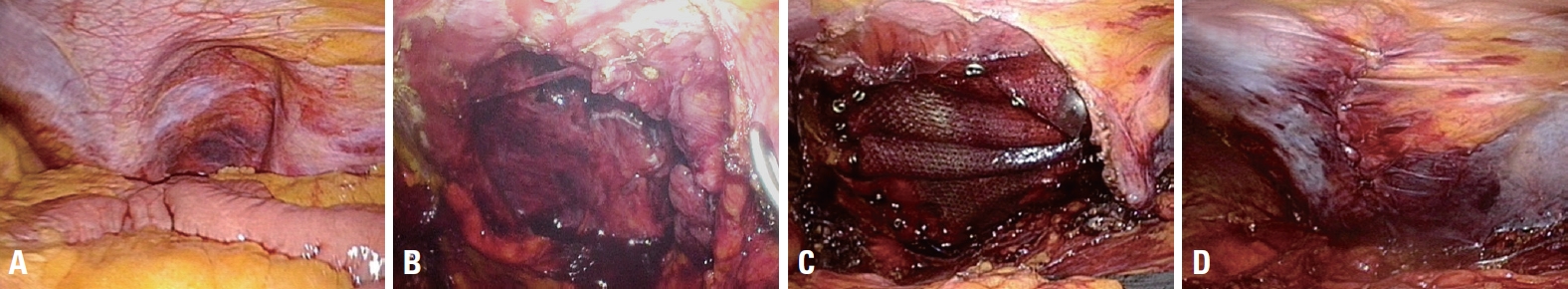
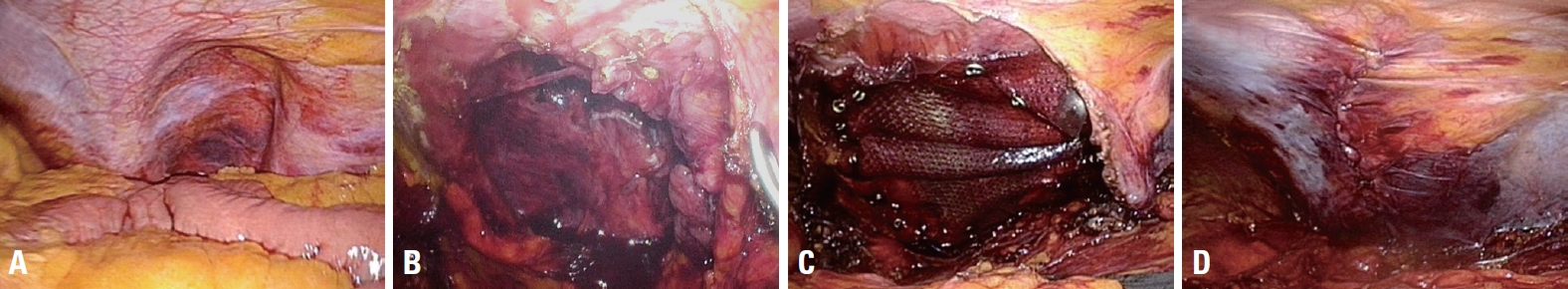
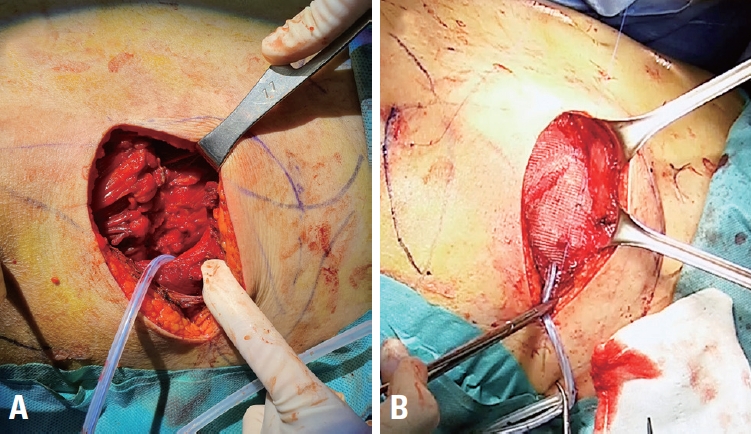
- A dual approach via both laparoscopic and open methods was planned. Under general anesthesia, the patient was placed in the right semi-lateral (45°) position. Laparoscopic surgery was conducted through the transabdominal approach. An 11-mm infra-umbilical camera-port and three working ports (a 5-mm port in the upper midline, an 11-mm port in the lower midline, and a 5-mm port in the right lower abdomen) were placed. The TFH in the left flank was identified, which included the small bowel and the descending colon (Fig. 3A). After the exploration of the whole bowel, a superficial mesenteric laceration of the small bowel and hematoma of the transverse colon were also observed. First, the descending colon was mobilized by making an incision along the lateral peritoneal fold, exposing the bottom edge of the hernia sac. After incision of the peritoneum, total disruption of the abdominal wall, measuring about 7×10 cm, was revealed (Fig. 3B). A sublay mesh (Parietene Composite Mesh; Covidien, Minneapolis, MN, USA) was introduced into the abdomen. A synthetic film side was laid to face the peritoneum to prevent painful adhesion of the parietal peritoneum to the mesh. The mesh was implanted via titanium tacker and a 3-0 barbed string (V-Loc 90 Absorbable, Covidien) with a 2-cm overlap on the edge of the disrupted transversalis muscle (Fig. 3C). The posterior margin of the polypropylene mesh was fixed to the lateral border of the psoas muscle. The mesh was then buried by continuously re-suturing the peritoneum (Fig. 3D). Extracorporeal hernioplasty (i.e., the open approach) was initiated after the termination of pneumoperitoneum. Full-thickness disruption of the external and internal oblique muscles of 11×15 cm was observed. A muscle split dissection was performed until it faced the intracorporeally augmented mesh. The separated internal oblique muscles were approximated using a 2-0 barbed suture (2/0 Stratafix Symmetric PDS Plus; Ethicon, Raritan, NJ, USA), and an onlay mesh (Prolene Mesh, Ethicon) was anchored on the muscular layer via a 3-0 Prolene suture (Fig. 4). A Jackson-Pratt drain was placed on the mesh to prevent fluid collection. The Scarpa’s fascia was then brought and closed up to cover the mesh as the bounced-off external oblique muscles were unreachable. The total duration of the operation was 255 minutes (Video S1).
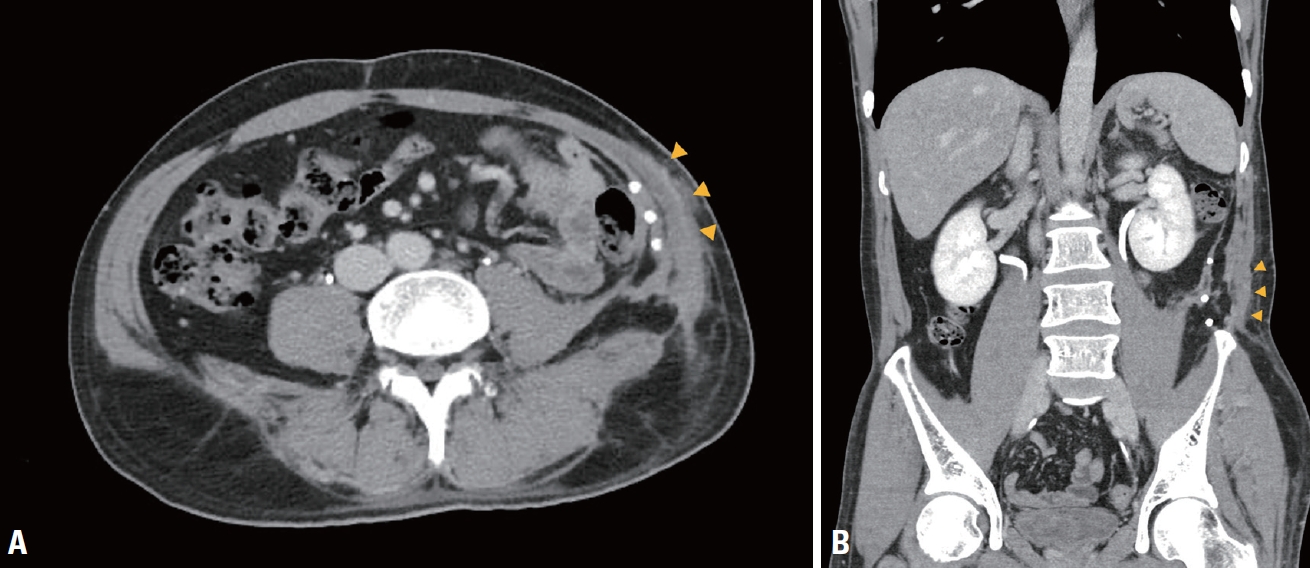
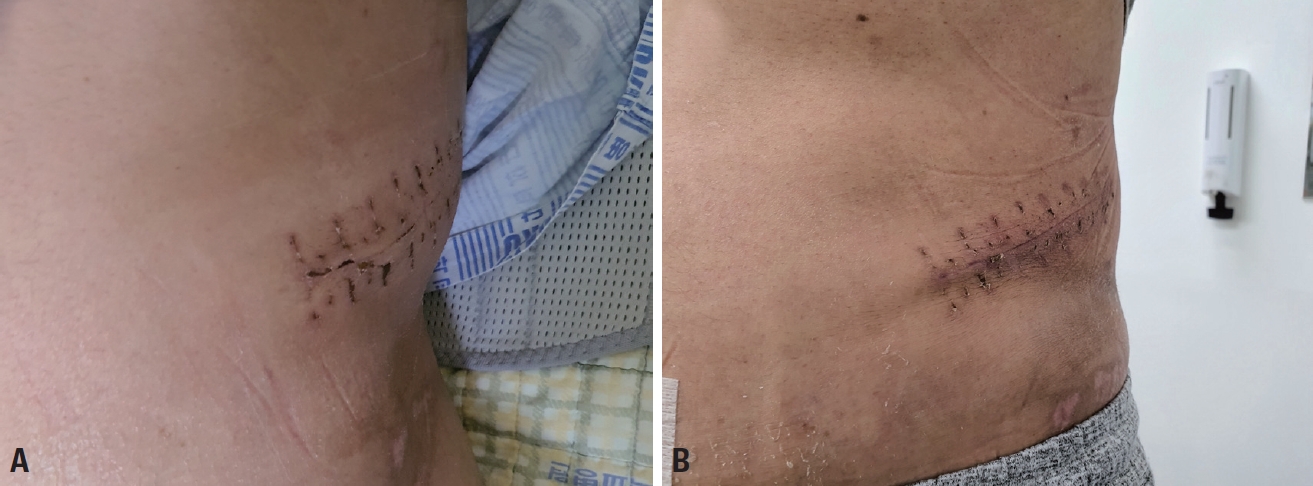
- The immediate postoperative period was uneventful. The Jackson-Pratt drain was withdrawn on postoperative day 3 as the content was minimal. The patient was discharged on postoperative day 18 after placement of an abdominal binder and did not experience any hernia recurrence during a 6-month follow-up period (Figs. 5, 6).
CASE REPORT
- A recent classification suggested by the largest single-institution series of TAWH categorizes it into three types: anterior abdominal, flank, and lumbar, which are affected by the rectus abdominis muscle, the oblique muscles, and the superior/inferior lumbar triangles, respectively [2]. TAWH does not always require operative repair, even though they are closely associated with other injuries. Several retrospective studies reported that delayed repair of TAWH was associated with fewer perioperative complications and lower recurrence [1]. The current consensus for patients with TAWH is conservative care unless the patient has hemodynamic instability or peritonitis [2]. In our case, the patient presented with persistent abdominal tenderness. Thus, laparoscopy was attempted with the double purpose of seeking other intra-abdominal injuries and implanting a sublay mesh.
- The open approach is traumatic and requires major dissection to expose the damaged planes and locate the defect, but it has the advantage of enabling complete parietal reconstruction. The laparoscopic approach has the advantages of being minimally invasive, producing less pain, resulting in a shorter length of hospital stay, and causing fewer wound complications. It also prevents major dissections, identifies the exact location of the lesion, and enables better visualization. However, the laparoscopic approach allows neither parietal reconstruction nor repair under controlled tension [4-6]. In our case, the sublay mesh implanted via laparoscopy alone was not enough to endure the large defect accompanying severe disruption of the external oblique muscle. Therefore, additional coverage of an onlay mesh was performed via the open approach.
- A sandwich technique that utilizes both onlay and sublay meshes for hernioplasty has been reported for lumbar hernia repair in many studies [7,8]. Mesh fixation in TFH repair is highly limited because the shearing force of the injury usually disrupts the musculofascial attachments to adjacent structures based on our previous experience. This technique is particularly well-suited for repairing TFH as well as lumbar hernia, where tension-free mesh fixation is anticipated from a severe injury. However, only the open approach has been used to perform the sandwich technique utilizing subcutaneous and extraperitoneal spaces according to the previous literature [9]. This is the first report using the dual tension-free repair method, which is a hybrid method taking advantage of both laparoscopic and open approaches.
- In conclusion, the dual tension-free repair method seems to be a feasible option for the treatment of large TFH, especially when concomitant intra-abdominal injuries are suspected. Although TFH is rare, the long-term success of this technique needs to be assessed to further prove its efficacy and safety. Trauma surgeons should reflect on the importance of making a correct preoperative assessment and an adequate choice of surgical techniques to offer the patients the best possible results.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: DHK; Methodology: YH; Investigation: YH; Visualization: YH; Project administration: DHK; Writing–original draft: YH; Writing–review&editing: DHK.
All authors read and approved the final copy of the manuscript.
ARTICLE INFORMATION
SUPPLEMENTARY MATERIALS

- 1. Netto FA, Hamilton P, Rizoli SB, et al. Traumatic abdominal wall hernia: epidemiology and clinical implications. J Trauma 2006;61:1058–61. ArticlePubMed
- 2. Coleman JJ, Fitz EK, Zarzaur BL, et al. Traumatic abdominal wall hernias: location matters. J Trauma Acute Care Surg 2016;80:390–6. ArticlePubMed
- 3. Suh Y, Gandhi J, Zaidi S, Smith NL, Tan MY, Khan SA. Lumbar hernia: a commonly misevaluated condition of the bilateral costoiliac spaces. Transl Res Anat 2017;8:1–5. Article
- 4. Moreno-Egea A, Baena EG, Calle MC, Martinez JA, Albasini JL. Controversies in the current management of lumbar hernias. Arch Surg 2007;142:82–8. ArticlePubMed
- 5. Park Y, Chung M, Lee MA. Traumatic lumbar hernia: clinical features and management. Ann Surg Treat Res 2018;95:340–4. ArticlePubMedPMC
- 6. Kaminski S, Diamond S. The early laparoscopic repair of a traumatic lumbar hernia: safe and successful. J Surg Case Rep 2017;2017:rjx188. ArticlePubMedPMC
- 7. Yang F. Extended Sublay repair: a modified open technique for lumbar hernias. J Plast Reconstr Aesthet Surg 2012;65:1605–6. ArticlePubMed
- 8. Lin R, Teng T, Lin X, et al. Sublay repair for primary superior lumbar hernia with the Kugel patch. ANZ J Surg 2020;90:776–80. ArticlePubMedPMC
- 9. Clothier JS, Ward MA, Ebrahim A, Leeds SG. Minimally invasive repair of a lumbar hernia utilizing the subcutaneous space only. Proc (Bayl Univ Med Cent) 2019;32:550–1. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Massive traumatic abdominal wall hernia in pediatric multitrauma in Australia: a case report
- Submental intubation using laparoscopic trocar in zygomaticomaxillary complex fracture surgery in Korea: a case report
- Repair of traumatic flank hernia with mesh strip suture: a case report
- Management of a traumatic anorectal full-thickness laceration: a case report
- Traumatic abdominal wall hernia with hemoperitoneum caused by blunt injury: laparoscopic exploration with mini-laparotomy repair. A case report
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite