Could the Injury Severity Score be a new indicator for surgical treatment in patients with traumatic splenic injury?
Article information
Abstract
Purpose
The purpose of this study was to determine whether a higher Injury Severity Score (ISS) could serve as an indicator of splenectomy in patients with traumatic splenic lacerations.
Methods
A total of 256 cases of splenic laceration were collected from January 1, 2005 to December 31, 2018. After the application of exclusion criteria, 105 were eligible for this study. Charts were reviewed for demographic characteristics, initial vital signs upon presentation to the emergency room, Glasgow Coma Scale, computed tomography findings, ISS, and treatment strategies. The cases were then divided into nonsplenectomy and splenectomy groups for analysis.
Results
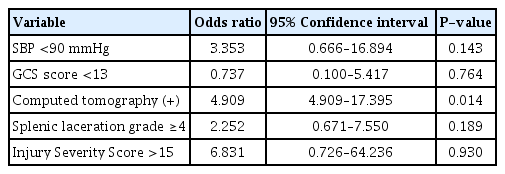
When analyzed with the chi-square test and t-test, splenectomy was associated with a systolic blood pressure lower than 90 mmHg, a Glasgow Coma Scale score lower than 13, active bleeding found on computed tomography, a splenic laceration grade greater than or equal to 4, and an ISS greater than 15 at presentation. However, in multivariate logistic regression analysis, only active bleeding on computed tomography showed a statistically significant relationship (P=0.014).
Conclusions
Although ISS failed to show a statistically significant independent relationship with splenectomy, it may still play a supplementary role in traumatic splenic injury management.
INTRODUCTION
Splenic lacerations are among the most common trauma-related injuries that may require surgery [1]. According to the World Society of Emergency Surgery classification and guidelines on splenic trauma, the anatomy of the injury, hemodynamic status, anatomic derangement, and associated injuries should be considered in treatment strategies. Occasionally, splenic laceration patients are treated with splenectomy. However, with medical advances, more patients are treated without surgery when hemodynamically stable.
In cases of splenic laceration without surgery, complications such as delayed subcapsular hematoma, pseudoaneurysm rupture, and splenic abscess may occur. However, overwhelming postsplenectomy infections may result after surgical management and can be fatal in up to 50% of cases [2].
The Injury Severity Score (ISS) is used to assess trauma patients through an anatomical evaluation of multiple injuries in six body parts. A higher ISS is associated with higher mortality [3]. Since ISS is associated with mortality, it is used worldwide to evaluate the severity of trauma patients. According to Rosati et al. [4], traumatic splenic laceration patients undergoing splenectomy have a higher ISS, as well as higher morbidity and mortality rates, than patients successfully managed without surgery. A study on pediatric trauma patients concluded that the ISS was the best predictor of the length of hospital stay and the need for surgery [5]. This study aimed to identify whether a higher ISS could be a new indicator of splenectomy in patients with traumatic splenic laceration.
METHODS
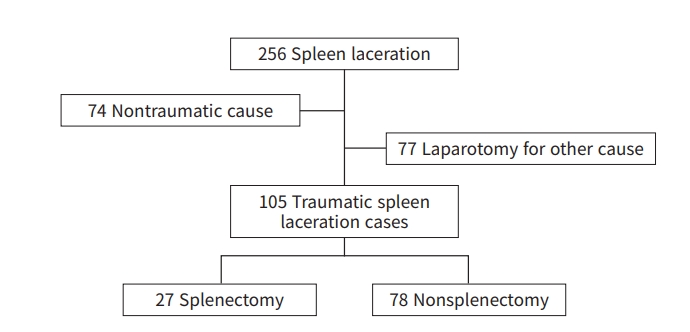
The study was approved by the Institutional Review Board of the Inje University Ilsan Paik Hospital (No. 2021-02-008). Informed consent was waived due to the retrospective nature of the study. In this retrospective, single-center study, patients with splenic laceration were searched from January 1, 2005 to December 31, 2018. Among 256 patients, 74 nontraumatic cases were excluded, as were the cases that required immediate laparotomy due to other causes besides splenic injury. In total, 105 patients were eligible for this study (Fig. 1).
Chart review was conducted to extract data on patients’ demographics, hemodynamic parameters at initial presentation, Glasgow Coma Scale (GCS), focused assessment with sonography for trauma findings if performed, computed tomography (CT) findings, ISS, and treatment modalities (surgery, embolization, or observation).
The patients were divided into nonsplenectomy and splenectomy groups. Total splenectomy was performed in all cases involving a surgical intervention. There were no cases of partial splenectomy, splenorrhaphy, or even simple bleeding control with cauterization.
The initial vital signs were considered unstable when the systolic blood pressure (SBP) was lower than 90 mmHg or the GCS was lower than 13. CT findings included active bleeding and the American Association for the Surgery of Trauma (AAST) splenic laceration grade. The ISS was calculated according to the Abbreviated Injury Scale updated in 2008. Out of the six body parts, the three parts with the highest assigned injury scores were squared and added together.
The data were analyzed with IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as mean values and standard deviations and analyzed using the t-test. Categorical data were expressed as numbers and percentages and analyzed using the chi-square test. Statistically meaningful factors from the univariate analysis were reanalyzed in multivariate logistic regression to identify independent indicators for splenectomy. A P-value ≤0.05 was considered to indicate statistical significance.
RESULTS
This study compared 105 patients according to whether they were managed without splenectomy (n=78) or underwent splenectomy (n=27). In the univariate analysis results shown in Table 1, the mean ages of patients were similar between the two groups (40.26 years in the nonsplenectomy group and 39.93 years in the splenectomy group). In the nonsplenectomy group, there was a higher proportion of patients older than 55 years (25.64%) than in the splenectomy group (11.11%), but this difference was not statistically significant. In both groups, the majority of patients were male (75.64% and 66.67%, respectively), and the between-group difference in sex distribution was not statistically significant.
Significantly more patients in the splenectomy group had an SBP lower than 90 mmHg upon presentation (P=0.021): seven of the 78 patients (8.97%) in the nonsplenectomy group versus eight of the 27 patients (29.63%) in the splenectomy group. The average GCS score was 14.40 in the nonsplenectomy group and 13.22 in the splenectomy group. When an analysis was conducting according to whether the GCS score was lower than 13, the two groups showed a statistically significant difference. Specifically, 10.26% of patients in the nonsplenectomy group had GCS scores lower than 13, while this was the case for 33.33% of the patients in the splenectomy group (P=0.012).
The splenectomy group had significantly more patients with active bleeding on CT (25.64% vs. 81.48%, P<0.001). The average AAST grade of the nonsplenectomy group was 2.71, while that of the splenectomy group was 3.78. The proportion of patients with a splenic laceration grade greater than or equal to 4 showed a statistically significant difference between the two groups (23.08% vs. 70.37% P<0.001).
The proportion of patients with an ISS greater than 15 was significantly different between the two groups: 39 of the 78 patients in the nonsplenectomy group versus 26 of the 27 patients in the splenectomy group (50.00% vs. 96.30%, P<0.001)
In the univariate analysis, an SBP lower than 90 mmHg, GCS score lower than 13, active bleeding on CT, splenic laceration grade greater than or equal to 4, and ISS greater than 15 were factors that showed statistically significant relationships with splenectomy. Multivariate logistic regression analysis was performed with these factors (Table 2). Only positive CT findings showed a statistically significant (P=0.014) independent relationship for determining splenectomy.
DISCUSSION
The decision to perform splenectomy in trauma patients is important because of complications that might develop later in their clinical course. This study attempted to identify whether the ISS could serve as a new indicator of splenectomy to improve the management of multiple trauma patients.
When choosing management without surgery, patients’ age was traditionally an important factor. Patients older than 55 years were believed to have a higher rate of failure in nonsurgical management. Thus, older patients were likely to be excluded from conservative management. In this study, however, patients older than 55 years were successfully managed without surgery. This finding could be attributed to medical advances in treating trauma patients over the past decades [6–9]. Unlike the older age group, there is a tendency to attempt to salvage the spleen in pediatric patients. However, in this study, pediatric patients were not included.
Splenic injury with hemodynamic instability is a well-known factor for failure of nonsurgical management, eventually leading to splenectomy [10,11]. Hemodynamic instability, represented by an SBP lower than 90 mmHg in this study, was also considered a statistically significant factor associated with splenectomy.
The GCS score is a readily accessible parameter since it is routinely recorded in trauma patients. The GCS score could be affected both by hemodynamic instability and traumatic brain injury. To preclude any possible confusion, patients with a low GCS score due to brain injury were excluded. In this study, a GCS score lower than 13 was associated with a significantly higher risk of splenectomy. However, according to Poletti et al. [12], patients with a GCS above 13 still had major abdominal injuries that would require surgery or embolization. Thus, it is questionable whether the GCS score should be used as a factor informing the choice of traumatic splenic injury management.
Zarzaur et al. [13] and Schurr et al. [14] demonstrated that active bleeding on abdominal CT observed upon presentation was a strong predictor of splenectomy. Through multivariate logistic regression analysis, this study also revealed that significantly more patients in the splenectomy group had active bleeding found on CT. However, Omert et al. [15] demonstrated that contrast extravasation alone was not an absolute indication for surgical or angiographic intervention. In another study, Teuben et al. [16] concluded that even with contrast extravasation on CT, hemodynamically stable splenic laceration patients could be managed without surgery in the absence of a concomitant hollow organ injury. Though it is important to obtain objective information on a patient’s medical condition through laboratory or imaging tests, the clinical presentation should always be taken into consideration.
Previous studies on splenic injury demonstrated that higher-grade splenic injuries are predictors of the failure of nonsurgical management. These patients should not be discharged early for further observation [17–19]. According to Olthof et al. [19] and McIntyre et al. [7], nonsurgical management was prone to fail for patients with an injury grade of 3 or more and a higher ISS (>25). Likewise, in this study, significantly more patients in the splenectomy group had a splenic laceration grade greater than or equal to 4.
In 1987, Boyd et al. [20] established that an ISS greater than 15 could serve as a threshold to indicate a severe injury, being predictive of 10% mortality. Therefore, the ISS threshold was set at 15 for this study. However, an ISS greater than 15 may correspond to a sole splenic injury with a score greater than 4 or multiple trauma injuries including splenic injury. In order to clarify any possible confusion, sole spleen injury patients were excluded, leaving multiple trauma patients only. Peitzman et al. [21] demonstrated that patients with ISS greater than 15 were significantly more likely to undergo surgery and experience failure of nonsurgical management. Thus, they examined the ISS as a new predictor of splenectomy in the management of splenic lacerations. In a pediatric trauma study, Potoka et al. [22] demonstrated that patients who underwent splenectomy were more likely to have an ISS greater than 15. However, hemodynamic instability—a well-established factor for surgical management—did not show a statistically significant association with splenectomy in their study. A possible explanation is that surgeons who conducted splenectomy considered only the ISS, but not patients’ hemodynamic status when deciding upon a treatment strategy. This demonstrates the importance of validating a factor before utilizing it in a management protocol since it may lead to inadequate management.
At first, the ISS seemed promising as a new indicator of surgery in splenic injury management. However, the statistical significance of the ISS did not remain in the multivariate logistic regression analysis. Thus, the ISS alone may not function as an indicator of splenectomy in trauma patients. However, a point to consider is that patients with an ISS greater than 15 had a tendency for active bleeding on CT (P<0.001) and high-grade splenic laceration (P<0.001), and were more likely to undergo splenectomy (P<0.001) (Table S1). Although the ISS was not proven to be suitable as a new indicator of splenectomy, it can still serve as a supplementary factor to improve the management of traumatic splenic lacerations.
Due to the development of radiologic interventions, embolization could be a possible solution for patients with active bleeding who are nonetheless hemodynamically stable [23]. In this study, there was only one case of embolization. However, this patient later developed splenic abscess and eventually underwent splenectomy (one out of 27, P=0.257). To establish a management protocol, including embolization as a possible approach in Inje University Ilsan Paik Hospital, more recent data are needed. In addition, long-term follow-up and complications should be recorded to evaluate the most appropriate treatment strategy for patients with splenic lacerations.
This study has some limitations. Even though multiple trauma patients may deteriorate at any given time, the hemodynamic instability recorded was represented with only the initial vital signs at the lowest point observed during the emergency room stay. Another limitation relates to the study design involving retrospective chart review. The ISS was also calculated only based on the recorded data and radiologic exams performed at the time of admission. Since this was a retrospective study, trauma patients were not thoroughly examined for the purpose of ISS evaluation on presentation. However, a prospective randomized control study on trauma patient management based on the ISS alone may lead to ethical issues. Due to the rarity of embolization, the effects of angiographic interventions could not be analyzed in this study.
The purpose of this study was to identify whether the ISS could serve as an indicator for splenectomy, thereby helping to reduce any possible complications. Further research is warranted with more recent data, including embolization cases and the treatment outcomes with long-term outpatient data.
In conclusion, in this study, a higher ISS alone did not show significant relevance to splenectomy in cases of traumatic splenic laceration. Although the ISS was not confirmed as a new indicator of splenectomy, it may still play a supplementary role in traumatic splenic injury management.
SUPPLEMENTARY MATERIALS
Table S1.
Univariate analysis using ISS as independent factor
Supplementary materials are available from: https://doi.org/10.20408/jti.2021.0065.
Notes
Ethical statements
The study was approved by the Institutional Review Board of the Inje University Ilsan Paik Hospital (No. 2021-02-008). Informed consent was waived due to the retrospective nature of the study.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: HJJ, SWJ; Data curation: all authors; Formal Analysis: HJJ, SWJ; Methodology: HJJ, SWJ; Project administration: SWJ; Supervision: SWJ; Visualization: HJJ; Writing–original draft: HJJ; Writing–review & editing: all authors.
All authors read and approved the final manuscript.