Radiologic assessment of the optimal point for tube thoracostomy using the sternum as a landmark: a computed tomography‐based analysis
Article information
Abstract
Purpose
This study aimed at developing a novel tube thoracostomy technique using the sternum, a fixed anatomical structure, as an indicator to reduce the possibility of incorrect chest tube positioning and complications in patients with chest trauma.
Methods
This retrospective study analyzed the data of 184 patients with chest trauma who were aged ≥18 years, visited a single regional trauma center in Korea between April and June 2022, and underwent chest computed tomography (CT) with their arms down. The conventional gold standard, 5th intercostal space (ICS) method, was compared to the lower 1/2, 1/3, and 1/4 of the sternum method by analyzing CT images.
Results
When virtual tube thoracostomy routes were drawn at the mid-axillary line at the 5th ICS level, 150 patients (81.5%) on the right side and 179 patients (97.3%) on the left did not pass the diaphragm. However, at the lower 1/2 of the sternum level, 171 patients (92.9%, P<0.001) on the right and 182 patients (98.9%, P= 0.250) on the left did not pass the diaphragm. At the 5th ICS level, 129 patients (70.1%) on the right and 156 patients (84.8%) on the left were located in the safety zone and did not pass the diaphragm. Alternatively, at the lower 1/2, 1/3, and 1/4 of the sternum level, 139 (75.5%, P=0.185), 49 (26.6%, P<0.001), and 10 (5.4%, P<0.001), respectively, on the right, and 146 (79.3%, P=0.041), 69 (37.5%, P<0.001), and 16 (8.7%, P<0.001) on the left were located in the safety zone and did not pass the diaphragm. Compared to the conventional 5th ICS method, the sternum 1/2 method had a safety zone prediction sensitivity of 90.0% to 90.7%, and 97.3% to 100% sensitivity for not passing the diaphragm.
Conclusions
Using the sternum length as a tube thoracostomy indicator might be feasible.
INTRODUCTION
Background
Tube thoracostomy (TT) is classically inserted directly in front of the mid-axillary line (MAL) and 5th intercostal space (ICS). The lateral border of the pectoralis major, lateral border of the latissimus dorsi, and upper border of the 5th ICS are called the “safety triangle” [1,2]. However, according to the studies by Griffiths and Roberts [3] and Elsayed et al. [4], many physicians are unable to accurately locate this safety triangle. Improper chest tube insertion outside the safety triangle can cause serious complications such as diaphragm injury [5]. To date, studies have been conducted to find the 5th ICS using ultrasound or the safety triangle using the nipples, axillary hair, or humerus length [6–8]. In patients with traumatic cardiac arrest or severe tension pneumothorax, insertion of a chest tube using ultrasound can be time-consuming. In addition, obesity, presence of developed breasts in females, and variable soft tissue position due to the arm position render finding the 5th ICS more challenging [9]. Therefore, it is necessary to develop a fast and easy TT technique using other fixed anatomical structures as an indicator.
Objectives
The sternum is a fixed, outermost part of the human body, which renders finding it easy. Accordingly, it is used as an indicator for the accurate application of chest compressions in cardiac arrest [10]. Additionally, the sternum has been used to guide emergent resuscitative endovascular balloon occlusion of the aorta (REBOA) or thoracic surgery [11,12]. However, to date, using the sternum as a guide for TT has not been investigated. Thus, this study aimed to evaluate the sternum as an indicator for TT, comparing the conventional TT technique using the 5th ICS with that using the sternum length.
METHODS
Ethics statement
This study was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GDIRB2023-270). The requirement for informed consent was waived due to the retrospective nature of this study. This study complies with the guidelines set forth by the Declaration of Helsinki
Study design and data collection
This retrospective study was conducted using preliminary data of the Korea Trauma Data Bank (KTDB) from a single regional trauma center (Gachon University Gil Medical Center, Incheon, Korea) in Korea. The preliminary data contained information on patients with trauma who visited this center between April and June 2022. The KTDB project studies the epidemiology of patients with trauma in Korea. As a government-developed database, all trauma centers in Korea are obligated to register in the KTDB the data of all the patients who are hospitalized due to trauma regardless of their Injury Severity Score (ISS). Accordingly, the KTDB includes data that are submitted by all 23 trauma centers in Korea regardless of the trauma center level.
The KTDB data consists of 392 items, including the characteristics and etiology of injury, diagnosis, treatment, complications, and outcomes of patients [13,14]. Demographic data, including age, sex, height, weight, mechanism of injury, Glasgow Coma Scale (GCS) score, vital signs, Revised Trauma Score (RTS), and final ISS were selected and collected.
Study population
All patients who visited a single regional trauma center in Korea were screened. Patients aged ≥18 years who underwent chest computed tomography (CT) for trauma with their arms down were included; whereas patients who underwent chest CT with their arms up were excluded. The relevant CT scans were retrieved by entering the patient’s medical record number, which is the preliminary data of the KTDB, into the picture archiving and communication system.
CT protocol
Patients with suspected chest trauma who arrived at the trauma center underwent a chest CT scan using the order, chest CT trauma. Patients were placed in the supine position, with their arms were placed downwards and at the side of the torso.
Nonenhanced and intravenous contrast-enhanced chest, abdomen, and pelvis CT scans were performed with a 6-second delay and scan time of 8.51 seconds using a 128-channel CT scanner (Siemens Healthineers). Patients were scanned with a pitch ratio of 1.5:1 and rotation speed of 0.5 seconds. Images were retrospectively reconstructed at the CT console to a 3.00-mm slice thickness.
Definitions and measuring method
In the CT scan, physical information of the patients, such as injured organs in the thorax and length of the sternum, was obtained, measured, and analyzed. Data involving the presence of subcutaneous emphysema, traumatic pneumothorax, hemothorax, fractured ribs, number of fractured ribs, and sternum fracture were collected.
In line with a pervious study by Wax and Leibowitz [15], the point was located on the right chest wall where the horizontal plane at the xiphoid process level meets the mid-axillary line (MAL) (Figs. 1A, S1). This point was found in the sagittal plane using the crosslink built into the picture archiving and communication system.
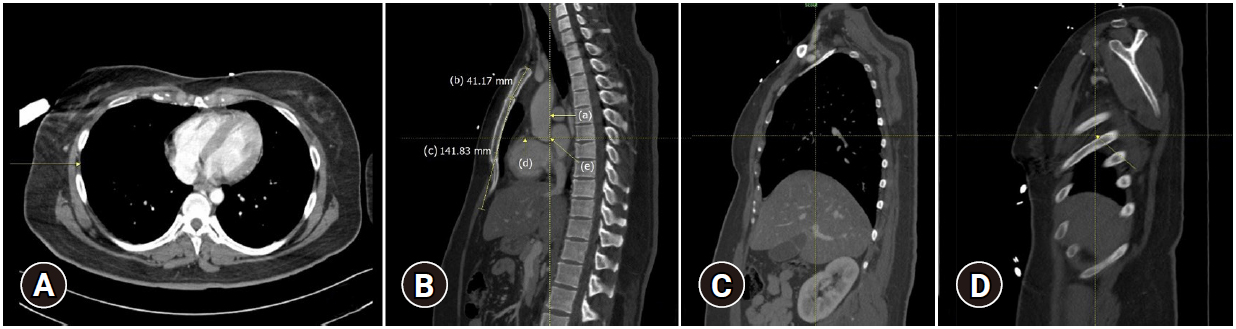
The process of finding the mid-axillary line (MAL), measuring the sternum length, and finding the lower 1/2 level of the sternum in the MAL at the end of the right torso. (A) The point on the right chest wall where the horizontal plane at the xiphoid process level meets the MAL (arrow). (B) The MAL at median plane (a). The length of the manubrium (b) was measured at 41.17 mm. The length from the sternal body to the xiphoid process (c) was measured at 141.83 mm. The scout line indicating the lower 1/2 level of the sternum (d) is obtained through (b) and (c). The point at the lower 1/2 level of the sternum and in the MAL at median plane (e). (C) Scrolling to the right side of the torso while maintaining a lower 1/2 level of the sternum and the MAL. (D) Moving to the right end of the torso shows that the lower 1/2 level of the sternum in the MAL is located at the 5th intercostal space and at the end of the right torso (arrow).
The MAL was defined as the scout line corresponding to the craniocaudal axis of the patient passing through this point (Fig. S2). Afterwards, we located a median plane and measured the lengths of the manubrium, sternal body-xiphoid process, total sternum (total length from sternal notch to xiphoid process, which is the sum of the manubrium length and straight length from sternal angle to the end of the xiphoid process), and the lower 1/2, 1/3, and 1/4 of sternum using the length calculator embedded in the picture archiving and communication system (Figs. 1B, S3, S4A) [16,17]. The sagittal section was scanned to determine which ICS was at the lower 1/2, 1/3, and 1/4 levels of the sternum in the MAL; that point was defined as the “possible TT site” (Figs. 1B–D, S4).
The presence of breast tissue at the “possible TT site” was assessed and the chest wall thickness through the scout line was measured from the skin to the pleural membrane (Fig. S5). The left-right scout line from the skin to the pleural membrane was defined as a “possible TT route.” The shortest perpendicular distance from the “possible TT route” at the sagittal plane to the pectoralis major and latissimus dorsi muscles was measured (Fig. S6). In addition, the cranio-caudal distance from the “possible TT route” to the highest point of the diaphragm at the coronal view was measured (Fig. S7). Moreover, the craniocaudal distance from the level of “possible TT route” to the highest point of the diaphragm at any anterioposterior location was measured (Fig. S8).
At the lower 1/2, 1/3, and 1/4 levels of the sternum and at the 5th ICS level, the same process was performed to gather information about the chest wall thickness, distance from the pectoralis major and latissimus dorsi, and the presence of breast tissue. Similarly, information about the left side of the torso was gathered.
The sternum 1/2, 1/3, and 1/4 methods was defined as performing TT through “possible TT route” of the lower 1/2, 1/3, and 1/4 levels of the sternum; the “5th ICS method” was defined as performing TT conventionally referring to the 5th ICS level.
“The feasibility of TT at safety zone” was defined as “possible TT routes” that are not passing the pectoralis major and latissimus dorsi, but passing the 5th ICS level and above. In practice, when a clinical practitioner locates a specific rib as a possible TT route, TT is performed at the ICS above that specific rib. Accordingly, “possible TT route” passing through a specific rib level was defined as passing the upper ICS. For instance, when the TT route was passing the 5th rib, it was considered as passing the 4th ICS, and it was regarded as the 4th ICS.
Primary outcome
The primary outcome was the predicted performance of the sternum 1/2, 1/3, and 1/4 methods compared to the performance of the 5th ICS method on adjacent structure injury and locating the safety zone.
Statistical analysis
Data were analyzed using SPSS ver. 17.0 (SPSS Inc). Continuous variables are presented as medians and interquartile ranges (IQRs) because of their skewed distributions. Paired comparisons were performed using the Wilcoxon signed rank test between each method using the sternum length and the standard method using the 5th ICS method. Categorical variables are expressed as frequencies and percentages, and comparisons were performed using the McNemar test between the methods. The sensitivity, specificity, and negative predictive value (NPV) and positive predictive value (PPV) of each method using the sternum length were calculated for the prediction of the safety zone compared to the standard method using the 5th ICS method. All statistical tests were two-sided, and a P-value <0.05 was considered as statistically significant.
RESULTS
Enrollment
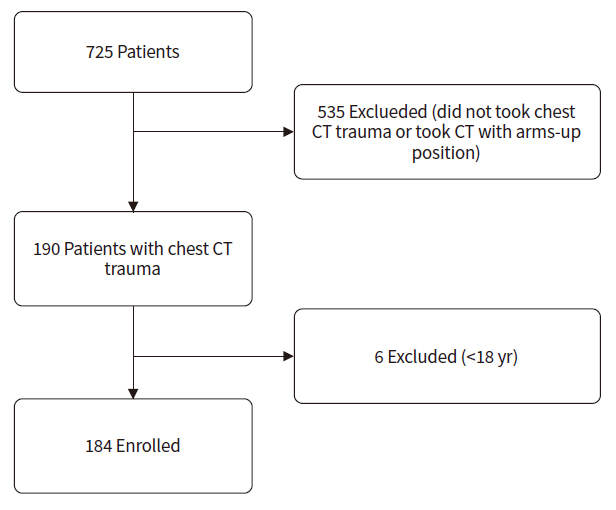
This study included 725 patients who visited a single regional trauma center in Korea (Fig. 2). A total of 535 patients were excluded. The exclusion criteria were the following: (1) not undertaking the chest CT trauma; or (2) undergoing CT with the arms in an upward position. Chest CT trauma was obtained in 190 of 725 patients (26.2%). Six patients were aged <18 years; thus, they were excluded. A total of 184 patients were enrolled in this study.
Characteristics of the study population
The median age of the 184 patients who visited the hospital was 53.5 years (IQR, 41.0–63.0 years) (Table 1). A total of 138 patients (75.0%) were male; the median weight was 67.5 kg (IQR, 56.1–78.2 kg) and the median height was 168.0 cm (IQR, 161.6–175.0 cm). Sternum fracture occurred in 31 patients (16.8%). The median number of fractured right and left ribs were 5 (IQR, 2–6) and 4 (IQR, 2–6), respectively. Among the injury mechanisms, blunt injuries were the most common form (168 patients, 91.3%). The median length of the sternum was 199.8 mm (IQR, 182.1–213.0 mm). The median lengths of the lower 1/4, 1/3, and 1/2 sternum levels were 50.0 mm (IQR, 45.5–53.2 mm), 66.6 mm (IQR, 60.7–71.0 mm), and 99.9 mm (IQR, 91.0–106.5 mm), respectively.
Comparison between the sternum and standard 5th ICS methods
The relationship between the sternum 1/2, 1/3, 1/4 methods and the 5th ICS method with adjacent structures was analyzed in 184 patients (Tables 2, 3). The routes of the sternum 1/2 method were located at the 5th ICS and above in 178 patients (96.7%) on the right side and 173 patients (94.0%) on the left side. The routes of the sternum 1/3 method were located at the 5th ICS and above in 91 patients (49.5%) on the right and 84 patients (45.7%) on the left. The routes of the sternum 1/4 method were located at the 5th ICS and above in 30 patients (16.3%) on the right and 25 patients (13.6%) on the left.

Relationships between “possible tube thoracostomy routes” and adjacent structures on the right side (n=184)

Relationships between “possible tube thoracostomy routes” and adjacent structures on the left side (n=184)
The routes of the 5th ICS method were not passing the diaphragm in 150 patients (81.5%) on the right and 179 patients (97.3%) on the left. Compared to the standard 5th ICS method, the sternum 1/2 method were not passing the diaphragm in 171 patients (92.9%, P<0.001) on the right and 182 patients (98.9%, P=0.250) on the left. The sternum 1/3 method were not passing the diaphragm in 105 patients (57.1%, P<0.001) on the right and 155 patients (84.2%, P<0.001) on the left. The sternum 1/4 method were not passing the diaphragm in 67 patients (36.4%, P<0.001) on the right and 108 patients (58.7%, P<0.001) on the left.
The median distances from the routes of the 5th ICS method to the highest diaphragm in the MAL were 31.0 mm (IQR, 8.3–54.6 mm) on the right and 48.6 mm (IQR, 29.3–69.9 mm) on the left. Compared to the 5th ICS method, the median distances from the routes of the sternum 1/2 method to the highest diaphragm in the MAL were 37.6 mm (IQR, 22.5–64.2 mm; P<0.001) on the right and 54.2 mm (IQR, 38.8–73.9 mm; P<0.001) on the left. The median distances from the routes of the sternum 1/3 method to the highest diaphragm in the MAL were 5.3 mm (IQR, 0–30.4; P<0.001) on the right and 22.2 mm (IQR, 9.0–42.6; P<0.001) on the left. The median distances from the routes of the sternum 1/4 method to the highest diaphragm in the MAL were 0 mm (IQR, 0–13.9 mm; P<0.001) on the right and 5.3 mm (IQR, 0–26.1 mm; P<0.001) on the left. The routes of the 5th ICS method were located at the safety zone in 160 patients (87.0%) on the right and 161 patients (87.5%) on the left. Compared to the 5th ICS method, the routes of the sternum 1/2 method were located at the safety zone in 151 patients (82.1%, P=0.093) on the right and 148 patients (80.4%, P=0.002) on the left. The routes of the sternum 1/3 method were located at the safety zone in 75 patients (40.8%, P<0.001) on the right and 73 patients (39.7%, P<0.001) on the left. The routes of the sternum 1/4 method were located at the safety zone in 30 patients (16.3%, P<0.001) on the right and 21 patients (11.4%; P<0.001) on the left.
The routes of the 5th ICS method were located at the safety zone and were not passing the diaphragm in 129 patients (70.1%) on the right and 156 patients (84.8%) on the left. Compared to the 5th ICS method, the routes of the sternum 1/2 method were located at the safety zone and were not passing the diaphragm in 139 patients (75.5%, P=0.185) on the right and 146 patients (79.3%, P=0.041) on the left. The routes of the sternum 1/3 method were located at the safety zone and were not passing the diaphragm in 49 patients (26.6%, P<0.001) on the right and 69 patients (37.5%, P<0.001) on the left. The routes of the sternum 1/4 method were located at the safety zone and were not passing the diaphragm in 10 patients (5.4%, P<0.001) on the right and 16 patients (8.7%, P<0.001) on the left.
Predicting the performance of the sternum 1/2, 1/3, 1/4 methods and the 5th ICS method on safety
Compared to the 5th ICS method, on the right, the routes of the sternum 1/2 method locating at the safety zone had a sensitivity of 90.0%, specificity of 70.8%, PPV of 95.4%, NPV of 51.5%, accuracy of 87.5%, and P-value of 0.093 (Table 4). Not passing the diaphragm had a sensitivity of 97.3%, specificity of 26.5%, PPV of 85.4%, NPV of 69.2%, accuracy of 84.2%, and P-value of <0.001. Locating at the safety zone and not passing the diaphragm had a sensitivity of 86.0%, specificity of 49.1%, PPV of 79.9%, NPV of 60.0%, accuracy of 75.0%, and P-value of 0.185. Locating at the safety zone and not passing the diaphragm or the breast tissue of the sternum 1/2 method had a sensitivity of 88.6%, specificity of 52.7%, PPV of 81.0%, NPV of 61.7%, accuracy of 76.1%, and P-value of 0.291.

Predicting the performance of the sternum 1/2, 1/3, 1/4 methods and the 5th ICS method on safety on the right side (n=184)
Compared to the 5th ICS method, on the left, the routes of the sternum 1/2 method locating at the safety zone had a sensitivity of 90.7%, specificity of 91.3%, PPV of 98.6%, NPV of 58.3%, accuracy of 90.8%, and P-value of 0.002 (Table 5). Not passing the diaphragm had a sensitivity of 100%, specificity of 40.0%, PPV of 98.4%, NPV of 100%, accuracy of 98.4%, and P-value of 0.250. Locating at the safety zone and not passing the diaphragm had a sensitivity of 90.4%, specificity of 82.1%, PPV of 96.6%, NPV of 60.5%, accuracy of 89.1%, and P-value of 0.041. Locating at the safety zone and not passing the diaphragm or the breast tissue of the sternum 1/2 method had a sensitivity of 89.5%, specificity of 78.1%, PPV of 95.1%, NPV of 61.0%, accuracy of 87.5%, and P-value of 0.093.
DISCUSSION
The routes of the sternum 1/2 method were located at the 5th ICS and above in 178 patients (96.7%) on the right and 173 patients (94.0%) on the left sides. The height difference from the diaphragm was the largest in the sternum 1/2 method on both sides, followed by the 5th ICS method, the sternum 1/3 method, and the sternum 1/4 method. On both sides, the routes of the 5th ICS method were most commonly located in the safety zone. Among the sternum methods, the sternum 1/2 method best predicted the safety zone, where the possibility of performing TT in the safety zone did not show a significant difference compared to that with the 5th ICS method on the right, but there was a significant difference on the left. On both sides, the routes of the sternum 1/2 method were passing the diaphragm to a lesser extent than the routes of the 5th ICS method, and there was a statistically significant difference on the right.
In this study, we aimed to evaluate whether the sternum, one of the easiest structures to locate when a clinician intuitively observes a patient’s body, can be used as an indicator for inserting a chest tube. Occasionally, the conventional method renders finding the structures that form the safety triangle difficult due to the patient’s physical characteristics. In patients with tension pneumothorax, trying TT for a long time finding the safety triangle can jeopardize the patient’s life. Advanced Trauma Life Support [6] recommends needle thoracostomy in urgent situations in patients with severe trauma. However, according to previous studies, the success rate of needle thoracostomy is not high, which could be attributed to the fact that the chest wall thickness of the thorax varies depending on the patient, making it difficult to predict the appropriate depth of needle thoracostomy. Moreover, anatomical differences between patients require different locations for needle thoracostomy [18–21]. In this case, a faster TT is needed, and we hypothesized that the sternum could be an auxiliary landmark for TT. The sternum can be useful in the cases were finding the safety triangle is rendered as difficult due to the physical characteristics of the patient and in urgent situations.
Among the methods using the sternum as a landmark, the sternum 1/3 and 1/4 methods pointed to a lower level than did the 5th ICS in about 50% to 90% of cases. Additionally, there were many cases where the possible TT routes passed the diaphragm. Accordingly, predicting the TT site using these methods seems inappropriate. However, when compared to the conventional 5th ICS method, the sternum 1/2 method showed superior prediction levels with a sensitivity of 90.0% to 90.7% for predicting the safety zone and a sensitivity of 97.3% to 100% for not passing the diaphragm. The sternum 1/2 method predicted the safety zone without a significant difference compared to the 5th ICS method, and the possibility of diaphragm injury was lower; thus, it may be sufficiently applicable in clinical practice. However, the sternum 1/2 method can point to an ICS that is too low or too high. According to our study results, the TT site of the sternum 1/2 method pointed to the 3rd–4th and 6th ICS in about 48% of the patients on the right side and 45% of the patients on the left. Therefore, caution is needed when performing TT with the sternum 1/2 method as injury to the surrounding anatomical structures may occur. Secondly, there may be differences between the method of measuring the sternum with the naked eye and that used in our study because the sternum is not a straight structure. Based on previous studies, we tried to measure the sternum length as closely as possible using the naked eye. However, clinicians need to ensure the accurate measurement of the sternum length when using this method since there may be differences in the actual sternum length in some cases.
Limitations
This study had some limitations. First, because this was a single-center study with a small study sample, it is difficult to generalize these results. Second, the MAL was defined according to a previous study by Wax and Leibowitz [15], which could be different from the actual clinical setting. In our study population, there was a difficulty in locating the accurate MAL in older people with kyphosis. Third, since the actual TT was performed by palpating the pectoralis major and breast tissue, the importance of passing tube through the pectoralis major, latissimus dorsi, and mammary gland could be questionable. This study was conducted using CT scan; thus, there was a difficulty associated with localizing the end of the attachment points of the pectoralis major and latissimus dorsi. Accordingly, it could be different from the actual palpating of these muscles when performing TT. Fourth, when TT is implemented, it is placed through the cephalic direction. “Passing the diaphragm in possible TT route” in this study did not imply causing diaphragm injury. Fifth, unlike the posture during performing TT, in this study, the soft tissue of the chest wall may be pressed and measured due to the supine and arms-down position with arms completely attached to the trunk in the obtained CT. Sixth, the patient’s diverse posture in the CT could result in errors during measurements. Lastly, depending on the patient’s posture during performing TT, some of the anatomical landmarks we measured may change. Caution is required when applying it in actual clinical settings.
Conclusions
The sternum 1/2 method predicted the safety zone with a good accuracy for TT insertion. When using the sternum 1/2 method, the possibility of cannulation in the safety zone did not show a significant difference compared to that of the 5th ICS method on the right side, but there was a significant difference on the left side. The routes of the sternum 1/2 method passed the diaphragm to a lesser extent than did the routes of the 5th ICS method on both sides, with a statistical difference on the right side. Thus, the sternum 1/2 method could be considered as a feasible additional landmark technique for TT.
Notes
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
The authors received no financial support for this study.
Author contributions
Conceptualization: all authors; Data curation: JJ, JHW, ML; Formal analysis: JHW; Methodology: JJ, JHW, WSC, YSL, JSC, JHJ, JYC, SYH; Project administration: JJ, JHW; Supervision: JHW; Visualization: JJ; Writing–original draft: JJ, JHW; Writing–review & editing: JHW, ML, WSC, YSL, JSC, JHJ, JYC, SYH. All authors read and approved the final manuscript.
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
Supplementary materials
Fig. S1.
The point on the right chest wall where the horizontal plane at the level of the xiphoid process meets the mid-axillary line is shown (arrow).
Fig. S2.
The process finding the mid-axillary line.
Fig. S3.
The median plane.
Fig. S4.
The lower 1/2 level of the sternum at the mid-axillary line.
Fig. S5.
Measurement of the chest wall thickness at the “possible tube thoracostomy route” at the lower 1/2 level of the sternum is shown.
Fig. S6.
Measurement of the shortest perpendicular distance to the pectoralis major from the “possible tube thoracostomy route” on the sagittal plane.
Fig. S7.
Measurement of the craniocaudal distance from the “possible tube thoracostomy route” to the highest point of the diaphragm on the coronal view.
Fig. S8.
Measurement of the craniocaudal distance from the level of the “possible tube thoracostomy route” to the highest point of the diaphragm at any anteroposterior location.
Supplementary materials are available from https://doi.org/10.20408/jti.2023.0058.