A rare and unique experience of a blunt intrathoracic traumatic injury of the trachea and its management in South Africa: a case report
Article information
Abstract
Blunt intrathoracic tracheal injuries are rare, even among blunt chest trauma patients. An early diagnosis based on a high index of suspicion allows for timely surgical management of potentially fatal airway trauma, thereby improving overall outcomes. Diagnosing these injuries can be difficult due to their nonspecific clinical features and the occasional difficulty in radiologic diagnosis. If a patient exhibits respiratory compromise with difficult ventilation and poor lung expansion, despite the insertion and management of an intercostal drain following high-energy blunt trauma, there should be a heightened suspicion of potential airway trauma. The aim of primary repair is to restore airway integrity and to minimize the loss of pulmonary parenchyma function. This case report discusses the rare clinical presentation of a patient with blunt trauma to the intrathoracic airway, the surgical management thereof, and his overall outcome. Although blunt traumatic injuries of the trachea are extremely rare and often fatal, early surgical intervention can potentially reduce the risk of mortality.
INTRODUCTION
Blunt intrathoracic tracheal injury is a rare finding among trauma patients. Its diagnosis is often delayed due to nonspecific symptoms, and it can have potentially devastating consequences [1]. Karmy-Jones and Wood [2] estimated the incidence of tracheobronchial injuries among blunt trauma patients to be approximately 0.5% to 2% based on clinical and autopsy reports but emphasized that the true incidence is difficult to determine since most studies combined penetrating and blunt cases. In a review of 1,178 blunt trauma autopsy reports [3], the incidence of tracheobronchial rupture was 2.8% and 81% of these patients died before reaching the hospital. For those patients who reach the hospital, mortality is still high: in a retrospective study comprising 265 blunt trauma cases [4] 26% of the patients with ruptures of the trachea died despite hospital treatment, while another retrospective review article comprising over 200 blunt tracheobronchial injury cases [5] found a mortality rate of up to 30%.
High-energy trauma with abrupt compression, deceleration, or shearing forces can injure trachea, usually within 3 cm of the carina [1,4,6]. Signs and symptoms include dyspnea, hemoptysis, and subcutaneous emphysema, but the clinical findings are nonspecific, and up to 10% of patients that have blunt intrathoracic tracheal trauma have no radiographic or physical evidence of the injury on their initial presentation [1]. The median time to diagnosis in blunt thoracic tracheal trauma has been reported to be 72 hours [4]. A high index of suspicion is crucial in order not to miss these injuries, as the mortality rate is reported to be up to 30%, but the functional outcome is generally good with early diagnosis and surgical repair [1,2,4,5,7]. Primary repair with suturing of the injury is the mainstay of surgical treatment, and intrathoracic tracheal injuries near the carina are approached via a right posterolateral thoracotomy [1,8,9].
As rare as this type of injury may be, the outcomes may be improved with early surgical intervention if there are indications noted on imaging, respiratory compromise with difficult ventilation, and poor lung expansion despite intercostal drain (ICD) insertion and management [1,6]. This case report discusses the rare clinical presentation of a patient with blunt trauma to the intrathoracic airway, the surgical management thereof, and his overall outcome.
CASE REPORT
Presentation
A 60-year-old man was found lying in a park, presumably assaulted with blunt objects to the torso and back. At the time of arrival, no known comorbidities were reported, but he was later diagnosed with smoker's bullous lung disease. Paramedics found him and transported him to a primary health care facility, where he presented with a Glasgow Coma Scale (GCS) score of 7 out of 15. A pneumothorax was identified on a chest x-ray (CXR), and a right ICD was inserted. The patient was then transferred to a trauma emergency unit. Upon examination, he was found to have subcutaneous emphysema extending from the neck down to the scrotum and both arms. His vital signs were as follows: oxygen saturation of 96% on a fraction of inspired oxygen (FiO2) of 0.5, blood pressure of 134/82 mmHg, and a pulse of 102 beats/min. An arterial blood gas analysis revealed a pH of 7.30, PCO2 of 68, PO2 of 92, lactate of 1.6, base excess of –1.1, bicarbonate of 24.1, hemoglobin of 13.3, and potassium of 4. Based on clinically reduced breath sounds detected on auscultation, a left ICD was subsequently inserted. Due to the patient's low GCS score, he was intubated in the emergency department of the trauma unit without immediate complications.
Imaging
The CXR revealed a significant amount of subcutaneous emphysema, a massive right pneumothorax with an ICD in situ, and a small left pneumothorax, also with an ICD in situ (Fig. 1). The computed tomography (CT) pan-scan showed notable surgical emphysema, tracking inferiorly along the anterior and lateral abdomen and flank, and extending into the scrotum and anterior thighs. There was a tracheal injury at the level of T3 to T4, which was complicated by extensive surgical emphysema and pneumomediastinum (Figs. 2, 3). Multiple rib fractures were present, accompanied by associated lung contusions, and a collapse of the right middle and lower lobe of the lung.
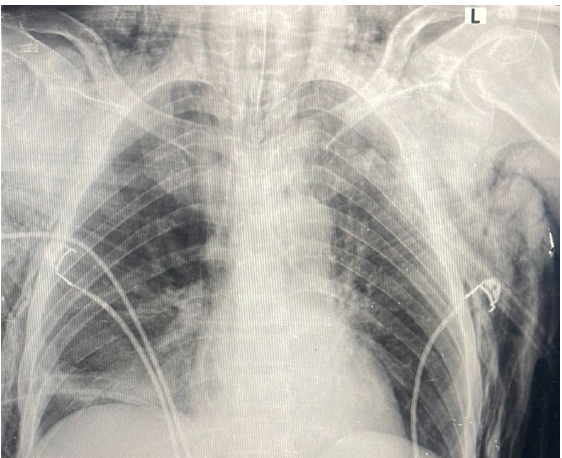
Preoperative chest x-ray of a patient with blunt tracheal trauma, showing massive subcutaneous emphysema, bilateral pneumothorax with bilateral intercostal drains, and the intubation tube in situ.
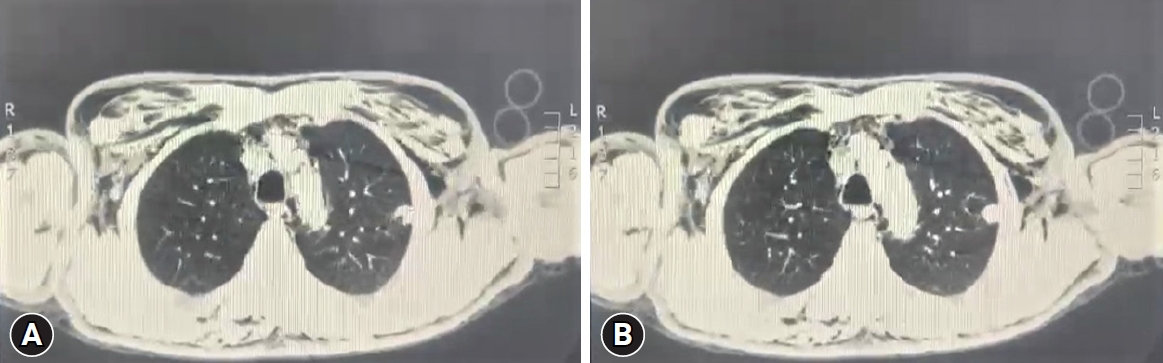
(A, B) Preoperative computed tomography images of the patient, showing the tracheal injury at the disrupted level of T3 to T4.
Surgery
The decision to proceed with surgery was made after the CT scan, without conducting further investigations such as bronchoscopy. The patient gave consent for surgery. In the operating room, the patient was placed in the left lateral position. A right 4th intercostal space posterolateral thoracotomy was performed. A disruption and laceration of the right lateral tracheal cartilage was noted at the T3 to T4 level, spanning over two cartilage rings in an oblique line of 1.5 cm. The visceral pleura remained intact over the injury, with the right lung poorly expanding. The injury was repaired using absorbable braided 3-0 sutures. The lung was then reexpanded and inflated. It was noted that the patient had bullous lung disease. Upon completion of the surgery, an arterial blood gas test was performed on the table with a FiO2 of 0.4. The results were as follows: pH of 7.37, PCO2 of 44, PO2 of 202, lactate of 0.9, base excess of –0.1, bicarbonate of 24.9, hemoglobin of 11.6, and potassium of 4.0. The patient was then transferred to the ward, as no intensive care unit beds were available. The patient was ventilated and did not require inotropic support.
Postoperative
The patient was ventilated in the ward for 10 days. The initially high ventilation pressures were reduced, and nosocomial respiratory sepsis was managed with empiric antibiotics, despite no growth in cultures. Nasogastric tube feeds were initiated, along with thromboprophylaxis and chest physiotherapy. On the 11th postoperative day, the patient was extubated, maintaining saturation on nasal prong oxygen at a rate of 2 mL/hr. The ICD was removed first on the left, then subsequently on the right, resulting in good lung expansion. Chest physiotherapy was conducted twice daily.
Ethics statement
This study was approved by the University of Witwatersrand Human Research Ethics Committee (No. M230288). Written informed consent for publication of the research details and clinical images were obtained from the patient.
DISCUSSION
As demonstrated by this case, early diagnosis is a prerequisite for the appropriate and successful treatment of tracheal rupture [6]. In keeping with previous reviews, primary repair of the trachea is adequate if the anatomy can be restored [9]. The respiratory complications of sepsis were treated accordingly when the indications arose, and this avoided further morbidity associated with such injuries [10,11]. The patient’s background of smoking and bullous lung disease predicted a longer or protracted recovery and the need for ventilatory support; however, the prognosis and outcome were still favorable and acceptable [2].
The majority of blunt intrathoracic tracheal injuries result from motor vehicle accidents or crush injuries [3–5]. Typically, the development of shearing forces at fixed points, such as the carina, during abrupt deceleration, or when the chest is compressed along its anteroposterior axis may explain why up to 80% of the injuries are found within 2 to 3 cm from the carina [2,4,7]. The tracheal cartilage may be disrupted, or sagittal tears may occur, with 8% presenting as complex injuries [1]. The related injuries seen with intrathoracic tracheal injuries after a high-energy impact are clavicular, sternal, and multiple rib fractures and lung contusions [1,5].
The signs and symptoms are mostly nonspecific, making the diagnosis challenging [1,6]. Tracheobronchial injuries in cases of blunt trauma are not immediately diagnosed in 25% to 68% of patients, and the median time to diagnosis of intrathoracic tracheal injury has been presented to be 72 hours [4]. Clinically subcutaneous emphysema is the most commonly occurring sign, and a large air leak and the inability of the lung to reexpand once an ICD is placed is indicative of these injuries, especially when there is a breach to the connective tissue around the trachea [1,12,13]. The diagnosis may be confirmed via imaging in the form of a plane CXR, neck and chest CT, or bronchoscopy [1,6]. The CXR may show pneumothorax, pneumomediastinum, subcutaneous emphysema and bony thoracic fractures. Radiolucent shadow along the anterior aspect of the spine, called “deep cervical emphysema,” should imply the possibility of tracheobronchial injury [1]. Findings suggestive of tracheal injury in CT are gas dispersion around the injury and bronchial lumen stenosis or displacement, but the radiologic diagnosis might still be challenging, raising the importance of clinical suspicion [6]. If the diagnosis remains unclear, bronchoscopy should be performed [1,2,6].
Intrathoracic tracheal injuries may be treated conservatively if the injury is less than 2 cm or less than one-third of the diameter of the trachea, there are no other injuries (e.g., to the esophagus), air leakage can be adequately controlled with the placement of ICD (i.e., there is expansion of the lung and no worsening subcutaneous emphysema), and there is no hemodynamic or respiratory compromise [1,6]. Additionally, the indications for surgery include the need to close a defect to improve ventilation and to avoid complications of spontaneously healed injuries that may result in stenosis or recurrent respiratory infections [14]. Tracheostomy is no longer routinely performed in airway trauma, especially if endotracheal intubation is achievable [4,15]. Intrathoracic tracheal injuries should be approached via a right thoracotomy in the 4th intercostal space [2,6,7]. Most injuries can be repaired by simple interrupted sutures or debridement and end-to-end anastomosis [1,2].
The overall mortality rate has been reported to be up to 30%, but when the diagnosis and surgery are done early after the injury, the long-term outcome is acceptable for 90% of patients [1,2,4–6]. Most instances of morbidity and complications are related to sepsis and long-term recovery [10,11]. Undiagnosed and untreated blunt intrathoracic tracheal injuries are usually followed by problems related to fibrosis and stenosis [1].
An early diagnosis, guided by a high index of suspicion, enables potentially fatal airway trauma to be managed surgically in a timely manner, thereby improving overall outcomes. The primary goal of repair is to restore the integrity of the airway and minimize the loss of pulmonary parenchyma function. Imaging modalities such as CXR, bronchoscopy, and CT scans can aid in identifying the extent of the injury, confirming the diagnosis, and facilitating surgical planning. Therefore, despite the extreme rarity and high mortality rate of blunt traumatic tracheal injuries, early management with surgical intervention may reduce the mortality rate.
Notes
Author contributions
Conceptualization: all authors; Methodology: all authors; Investigation: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
The authors received no any financial support for this study.
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.

