Validity of the scoring system for traumatic liver injury: a generalized estimating equation analysis
Article information
Abstract
Purpose
The scoring system for traumatic liver injury (SSTLI) was developed in 2015 to predict mortality in patients with polytraumatic liver injury. This study aimed to validate the SSTLI as a prognostic factor in patients with polytrauma and liver injury through a generalized estimating equation analysis.
Methods
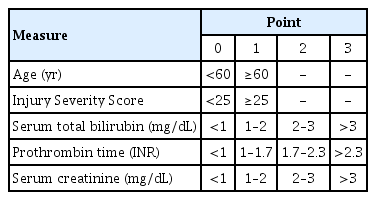
The medical records of 521 patients with traumatic liver injury from January 2015 to December 2019 were reviewed. The primary outcome variable was in-hospital mortality. All the risk factors were analyzed using multivariate logistic regression analysis. The SSTLI has five clinical measures (age, Injury Severity Score, serum total bilirubin level, prothrombin time, and creatinine level) chosen based on their predictive power. Each measure is scored as 0–1 (age and Injury Severity Score) or 0–3 (serum total bilirubin level, prothrombin time, and creatinine level). The SSTLI score corresponds to the total points for each item (0–11 points).
Results
The areas under the curve of the SSTLI to predict mortality on post-traumatic days 0, 1, 3, and 5 were 0.736, 0.783, 0.830, and 0.824, respectively. A very good to excellent positive correlation was observed between the probability of mortality and the SSTLI score (γ=0.997, P<0.001). A value of 5 points was used as the threshold to distinguish low-risk (<5) from high-risk (≥5) patients. Multivariate analysis using the generalized estimating equation in the logistic regression model indicated that the SSTLI score was an independent predictor of mortality (odds ratio, 1.027; 95% confidence interval, 1.018–1.036; P<0.001).
Conclusions
The SSTLI was verified to predict mortality in patients with polytrauma and liver injury. A score of ≥5 on the SSTLI indicated a high-risk of post-traumatic mortality.
INTRODUCTION
The abdominal cavity is the third most common site affected by trauma [1]. The liver is the most frequently injured organ in abdominal trauma despite being relatively shielded by the ribs [2–5], and liver trauma is the leading cause of death in major abdominal trauma [6,7]. Therefore, one of the most important roles of trauma centers is the successful treatment of liver injuries. Previously, patients with liver trauma underwent surgical treatment with techniques including packing, hepatorrhaphy, vessel ligation, and hepatic resection [8]. Emergent operative management (OM) for liver injuries in hemodynamically unstable patients is essential [7,9]. However, nonoperative management (NOM), including watchful waiting and/or arterial embolization, is the preferred treatment modality in hemodynamically stable patients [7,10].
There are various scoring systems to establish the physiological severity of injuries and the prognoses of patients who have sustained trauma. The Acute Physiology and Chronic Health Evaluation Score [11], Injury Severity Score (ISS) [12], Revised Trauma Score [13], and Trauma and Injury Severity Score [14] are used to determine the severity and prognosis of injuries. However, these scoring systems are not specific to liver trauma; they are specific to various other types of injuries [15].
Given the lack of a liver-specific scoring system despite the importance of liver trauma treatment, we published a study that examined prognostic factors in patients with polytrauma and liver injury and developed a scoring system for traumatic liver injury (SSTLI) to predict mortality in 2015 [15]. This study aimed to validate the SSTLI as a prognostic factor in patients with polytrauma and liver injury.
METHODS
This study was approved by the Institutional Review Board of the Pusan National University Hospital, Busan (No. H-2012-022-098).
Components of the SSTLI
We published a study on the SSTLI in 2015 using patients’ laboratory values and initial history data [15]. As shown in Table 1, the SSTLI uses five clinical measures (age, ISS, serum total bilirubin level, prothrombin time, and creatinine level), and each measure was scored from 0 to 1 (age and ISS) or from 0 to 3 (serum total bilirubin level, prothrombin time, and creatinine level). The SSTLI score corresponds to the sum of points for each item (0–11 points).
Study population
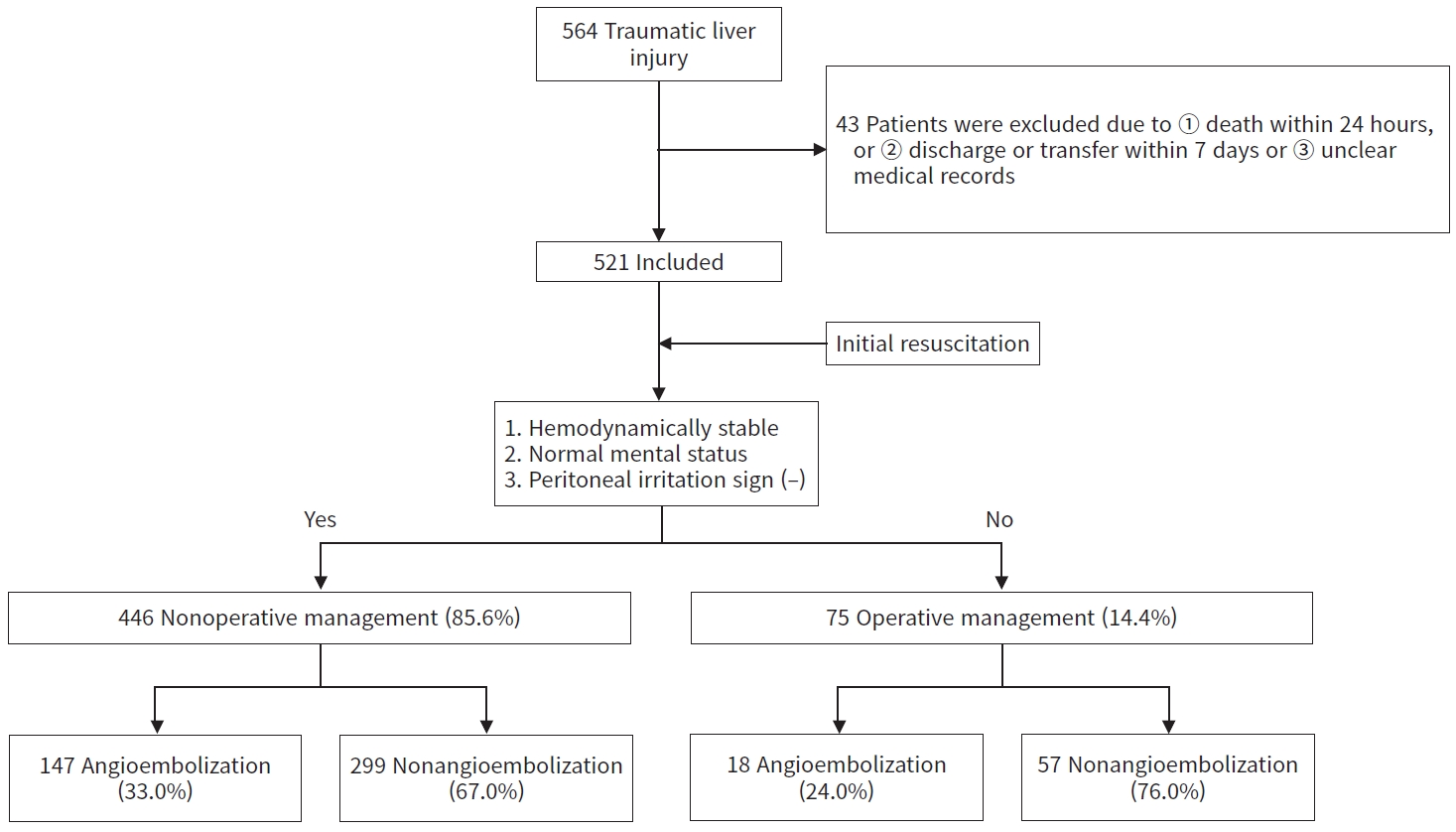
Patients with polytrauma and liver injury were included in this study because liver trauma is almost always accompanied by other organ injuries. In total, 564 patients with polytrauma and liver injury admitted to the emergency room at Pusan National University Hospital, Busan between January 2015 and December 2019 were considered for this study. Patients who died within 24 hours or who were discharged or transferred within 7 days were excluded because they were judged to be unsuitable for determining patients’ prognosis after successful resuscitation. With the additional exclusion of those with inadequate medical records, 43 patients were excluded. Therefore, 521 patients were enrolled in this study. If a patient was hemodynamically stable after initial resuscitation, had a normal mental status, and had no signs of peritoneal irritation upon arrival at the emergency room, the patient underwent NOM. According to this protocol, 446 patients underwent NOM and 75 patients underwent OM.
We performed a retrospective chart review of 521 patients with polytrauma and liver injury. We collected data on age, sex, and laboratory values (levels of total bilirubin, prothrombin time, and creatinine) from electronic medical records.
Outcome measures
The primary outcome variable was in-hospital mortality. Clinical variables were analyzed to identify factors predicting mortality after hospital management.
Statistical analysis
The Mann-Whitney U-test and the Wilcoxon rank-sum test were used to compare the mean values of the continuous variables and ordinal data, respectively. The chi-square test and Fisher exact test were used to compare the frequencies of categorical variables between groups. We modelled repeated measurements of all variables related to the SSTLI over time using a generalized estimating equation (GEE) extension of a logistic regression model [16]. We used the receiver operating characteristic curve and area under the curve (AUC) to evaluate prognostic factors predicting death. All risk factors were analyzed using multivariate logistic regression analysis. The SSTLI was created based on the predictive power of each factor. A P-value of ≤0.05 was considered to indicate statistical significance. All statistical analyses were performed using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA) and Stata ver. 14.2 (Stata Corp., College Station, TX, USA).
RESULTS
Clinical characteristics of patients with traumatic liver injury
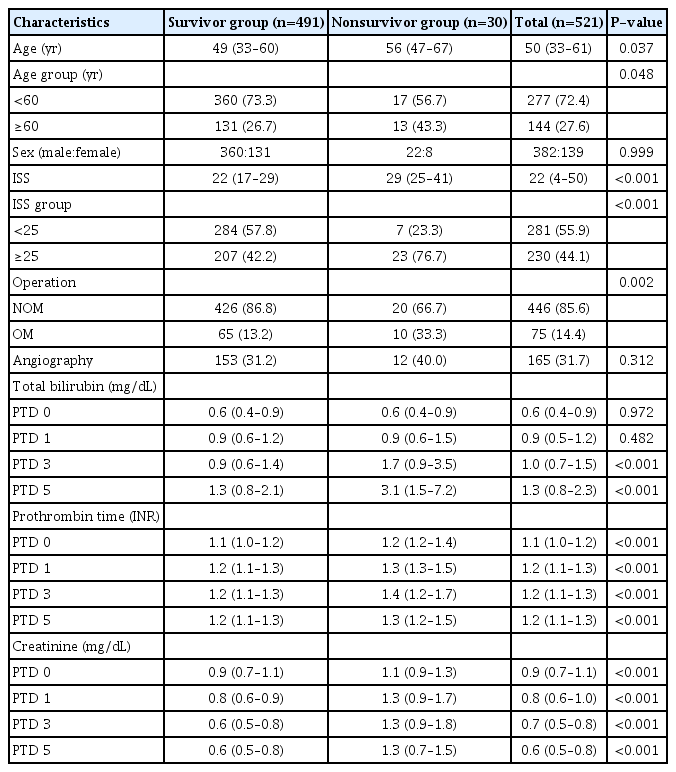
The clinical characteristics of patients (382 male patients [73.3%] and 139 female patients [26.7%]; median age, 50 years; interquartile range [IQR], 33–61 years) are shown in Table 2. The average ISS was 22 (IQR, 4–50). In total, 446 patients (85.6%) underwent NOM, 75 patients (14.4%) underwent OM, and 165 patients (31.7%) underwent angiography (Fig. 1).
Of the 521 patients, 30 patients (5.8%) died in the hospital. There was no significant difference between survivors and nonsurvivors with regard to sex. The median age, median ISS, and percentage of OM were higher in nonsurvivors than in survivors (P=0.037, P<0.001, and P=0.002, respectively). The serum total bilirubin level (after post-traumatic day [PTD] 3), prothrombin time, and creatinine level were higher in nonsurvivors than in survivors. The AUC values for age and ISS showed a significant increase relative to the null curve (AUC=0.613, P=0.037 and AUC=0.740, P<0.001, respectively) (Fig. S1).
Clinical characteristics of patients according to the treatment method (NOM vs. OM)
The clinical characteristics of patients according to the treatment method (NOM vs. OM) are summarized in Table S1. Median age, sex, and ISS did not significantly differ between the OM and NOM groups.
Validation of the SSTLI and the cutoff point to distinguish between low-risk and high-risk patients
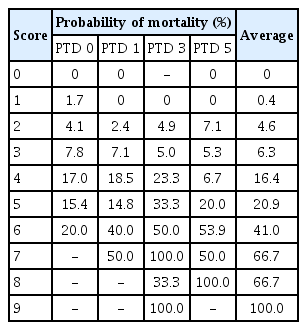
The application and effectiveness of the SSTLI in predicting mortality are summarized in Table 3. The mean and standard error plots of the SSTLI are shown in Fig. 2. The effectiveness of the SSTLI for predicting mortality was significant for PTDs 0, 1, 2, 3, and 5 (P<0.001, P<0.001, P<0.001, P<0.001, and P<0.001, respectively).
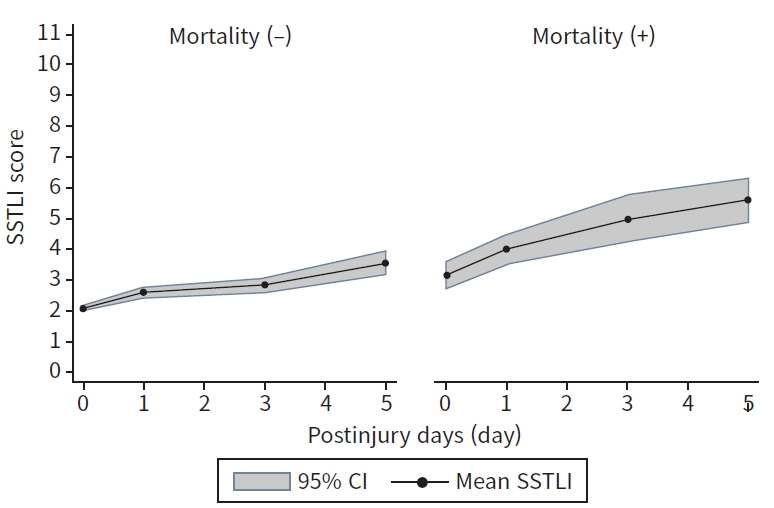
Mean and standard error plots of the scoring system for traumatic liver injury (SSTLI); shaded areas represent ±2 standard errors. CI, confidence interval.
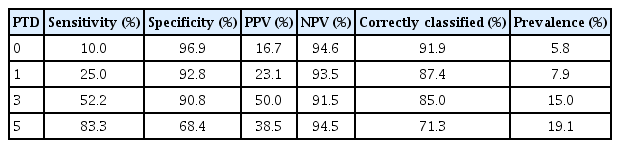
The AUCs of the SSTLI to predict mortality on PTDs 0, 1, 3, and 5 were 0.736 (P<0.001), 0.783 (P<0.001), 0.830 (P<0.001), and 0.824 (P<0.001), respectively (Fig. 3). When the ability of the SSTLI to predict death was compared with that of age and ISS, the AUC of the SSTLI on PTD 0 was not statistically significantly different from that of age and ISS (P=0.081) (Fig. 4A). However, the AUC of the SSTLI was higher than that of age and ISS on PTDs 1, 3, and 5 (P=0.032, P<0.001, and P<0.001, respectively) (Fig. 4B–D). Table 4 shows the probability of mortality in our population according to the SSTLI. A very good to excellent positive correlation was observed between the probability of mortality and the SSTLI score (γ=0.997, P<0.001) (Fig. 5). Based on this result, we used a value of 5 points as the threshold to distinguish between low-risk (<5) and high-risk (≥5) patients. The sensitivity, specificity, positive predictive value, negative predictive value, and the correctly classified rate of the SSTLI with a cutoff of 5 points are shown in Table 5.
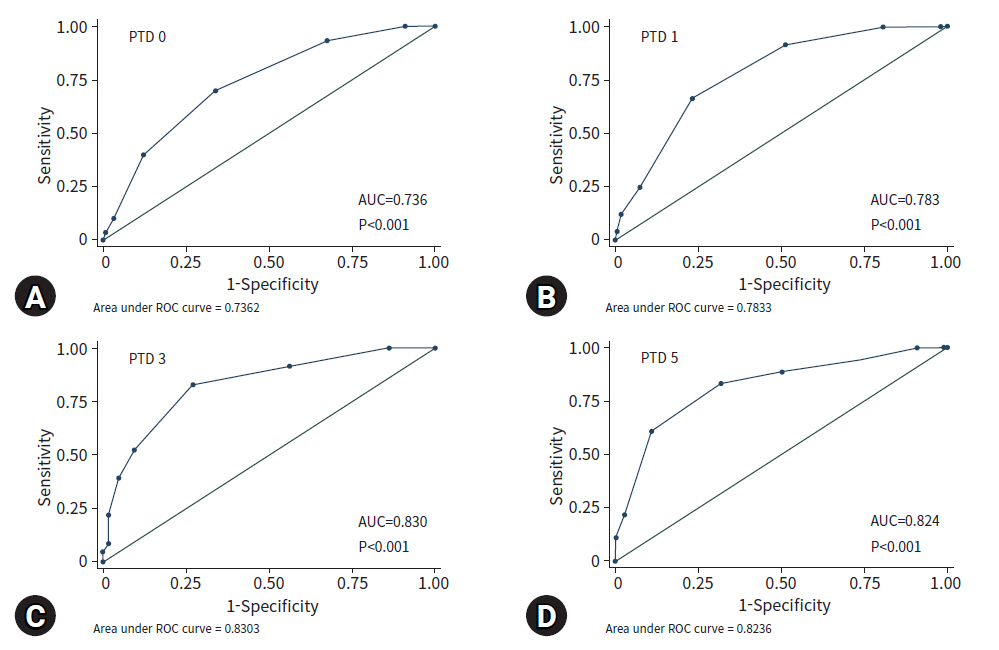
Receiver operating characteristic (ROC) curves for the scoring system for traumatic liver injury; all areas under the ROC curves were significantly greater than that of the null area. (A) PTD 0, (B) PTD 1, (C) PTD 3, and (D) PTD 5; P<0.001. PTD, post-traumatic day; AUC, area under the curve.
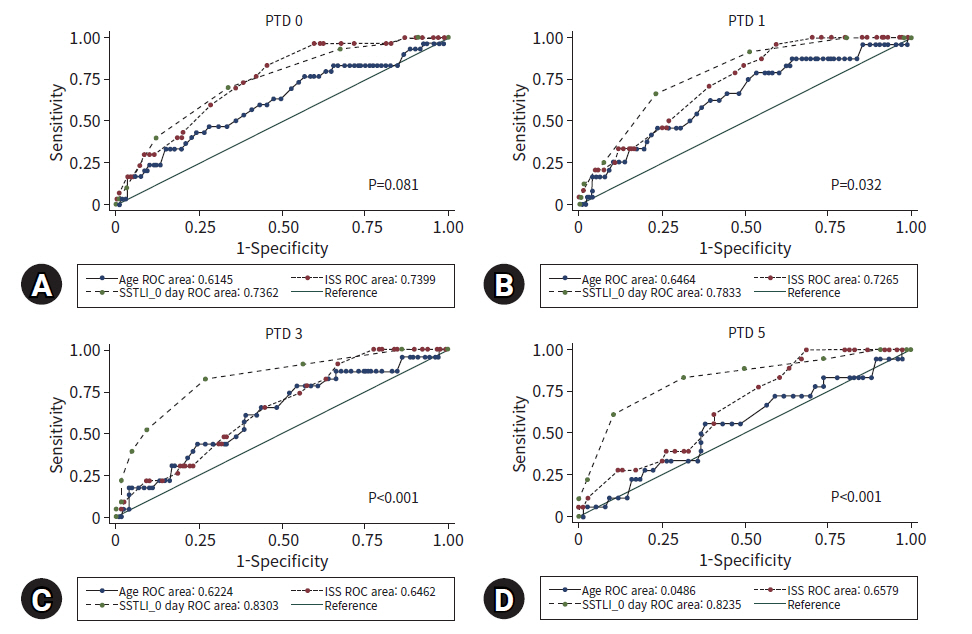
Receiver operating characteristic (ROC) curves for age, Injury Severity Score (ISS), and the scoring system for traumatic liver injury (SSTLI); the area under the curve of the SSTLI on (A) post-traumatic day (PTD) 0 was not statistically significantly different from that of age and ISS. However, the area under the curve of the SSTLI was greater than that of age and ISS on (B) PTD 1, (C) PTD 3, and (D) PTD 5.

Correlation between the probability of mortality in patients with polytrauma and liver injury and the scoring system for traumatic liver injury (SSTI; Spearman rho=0.997, P<0.001; SSTLI 0–SSTLI 5).
Multivariate analysis using a GEE
Multivariate analysis using a GEE in a logistic regression model indicated that the SSTLI score was an independent predictor of mortality (odds ratio, 1.027; 95% confidence interval, 1.018–1.036; P<0.001) (Table 6).
DISCUSSION
This study demonstrated the efficiency and performance of the SSTLI in predicting mortality in patients with polytraumatic liver injury. Although several scoring systems to predict the prognosis after trauma have been developed, they are not specific to traumatic liver injury. In the case of patients with trauma and chronic liver disease, chronic liver disease scoring systems such as the Child-Turcotte-Pugh system or the model for end-stage liver disease can be useful predictors of hepatic complications and the overall prognosis [17,18]. Hence, we developed the SSTLI in 2015 for traumatic liver injury based on the Child-Pugh scoring system (Table 1) [15,19].
The SSTLI employs five clinical measures (serum total bilirubin, prothrombin time, serum creatinine, age, and the ISS) [15]. Each risk factor is assigned a point value. The discriminatory value of the SSTLI was high. In addition, the SSTLI was found to be more predictive of mortality than age or ISS alone. In this study, multivariate analysis using a GEE with a logistic regression model indicated that the SSTLI was an independent predictor of mortality. A cutoff of 5 points in the SSTLI was used to distinguish patients at a high-risk of mortality. With its high specificity and negative predictive value, this scoring system demonstrated the potential to rule out mortality risk. Multivariate analysis using the GEE with the logistic regression model indicated that the SSTLI was an independent predictor of mortality. These data resemble the findings of a previous study [15], and the SSTLI also predicted mortality in patients with traumatic liver injury in this study.
The SSTLI has several advantages. First, it is easy to calculate and intuitive because it involves only addition using the SSTLI table. The mortality of patients with polytrauma and liver injury can be predicted immediately. Second, the SSTLI can be calculated daily using the daily laboratory data of serum bilirubin level, prothrombin time, and creatinine level, and changes in the SSTLI can be used to predict the prognosis of patients with polytrauma and liver injury. If the SSTLI score decreases after PTD 0, the patient’s prognosis may be better. Alternatively, if the SSTLI score consistently increases or remains >5 points, the patient’s prognosis may be worse. Third, the selected variables are indicators of poor outcomes of any injury. Therefore, we think that this model can be extended to encompass other injury types as well as liver injury.
This study was a result of follow-up with a larger group of patients over a longer period than in our previous study [15]. This study suggests that the SSTLI is useful, as it was verified to be a prognostic factor in patients with polytrauma with liver injury.
This study has several limitations. First, there are many other variables that could have been considered, but were not included in our model (e.g., serum levels of base deficit and lactic acid increase in the case of sepsis, multiple organ dysfunction, and shock) [20–24]. Second, age and ISS, which are the major factors we used in the scoring system, are themselves major factors already used to predict the prognosis of trauma patients. In addition, the question remains of whether serum total bilirubin, prothrombin time, and creatinine are specific factors related to liver injury in trauma patients. In the future, a comparative study between patients without liver damage and those with liver injury using this scoring system would be helpful. Finally, this study included patients from a single center and also was a nonrandomized, retrospective analysis. Our study population might be specific to a region, which might limit the generalizability of our findings. External validation would be required to confirm the generalizability of the SSTLI. Additional prospective, randomized, controlled trials with larger sample sizes are necessary to confirm the validity of the SSTLI.
In conclusions, we investigated prognostic factors in patients with traumatic liver injury and reaffirmed the validity of the SSTLI to predict mortality. An SSTLI score of 5 or higher indicated a high-risk of post-traumatic mortality. Our study suggests that the SSTLI could be used to predict mortality in patients with traumatic liver injury. Patients who score 5 or higher on the SSTLI should be monitored particularly carefully.
SUPPLEMENTARY MATERIALS
Fig. S1.
Receiver operating characteristic (ROC) curves for (A) age and (B) Injury Severity Score (ISS); the area under the curve (AUC) for age and ISS were significantly greater than the null area (P<0.01).
Table S1.
Clinical characteristics of patients with traumatic liver injury according to the treatment method
Supplementary materials are available from: https://doi.org/10.20408/jti.2021.0009.
Notes
Ethical statement
This study was approved by the Institutional Review Board of the Pusan National University Hospital, Busan (No. H-2012-022-098).
Conflicts of interest
Hohyun Kim and Chan Yong Park serve on the Editorial Board of Journal of Trauma and Injury, but were not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
Funding
This work was supported by a clinical research grant from Pusan National University Hospital in 2021.
Author contributions
Conceptualization: RDY, KHH; Data curation: RDY; Formal analysis: KHH; Investigation: RDY; Methodology: LGH, JCH, KHH; Project administration: RDY, KHH; Resources: LGH, KHH; Supervision: KJH, YSR; Validation: KHH, KJH; Visualization: JCH; Writing–original draft: LGH; Writing–review & editing: KHH, PCY, YSR.
All authors read and approved the final copy of the manuscript.