Delayed manifestation of Isolated Intramural Hematoma of the duodenum resulting from Blunt abdominal Trauma
Article information
Abstract
Duodenal injury following blunt abdominal trauma is a relatively unusual complication, and it may sometimes be difficult to distinguish a duodenal hematoma from duodenal perforation. According to recent reports, intramural hematomas typically resolve spontaneously with conservative treatment. Surgery, however, is occasionally necessary in some cases if the diagnosis is delayed, conservative therapy fails, or a high degree of suspicion of duodenal injury persists. We experienced a case of delayed manifestation of a duodenal intramural hematoma that was surgically treated.
INTRODUCTION
Duodenal injuries are uncommonly encountered, but their incidence has increased in recent years because of the increasing frequency of automobile accidents and violent incidents [1]. Since duodenal injuries can be accompanied by injuries of other organs, including the liver, biliary tract, stomach, and pancreas, the early diagnosis and treatment of duodenal injuries are critical. Intramural duodenal hematoma after blunt abdominal trauma mostly occurs in children and young adults, and manifests with various symptoms that range from mild abdominal pain to severe abdominal pain with vomiting, intestinal obstruction, and bowel perforation in critically ill patients with a large hematoma [2]. Due to the rarity of this condition, many clinicians have an insufficient understanding of duodenal injuries and a lack of experience treating them; as a result, the diagnosis and treatment of these injuries can be delayed, with significant effects on morbidity and death [3]. Therefore, we report a case of a delayed manifestation of isolated intramural hematoma of the duodenum following blunt abdominal trauma.
CASE REPORT
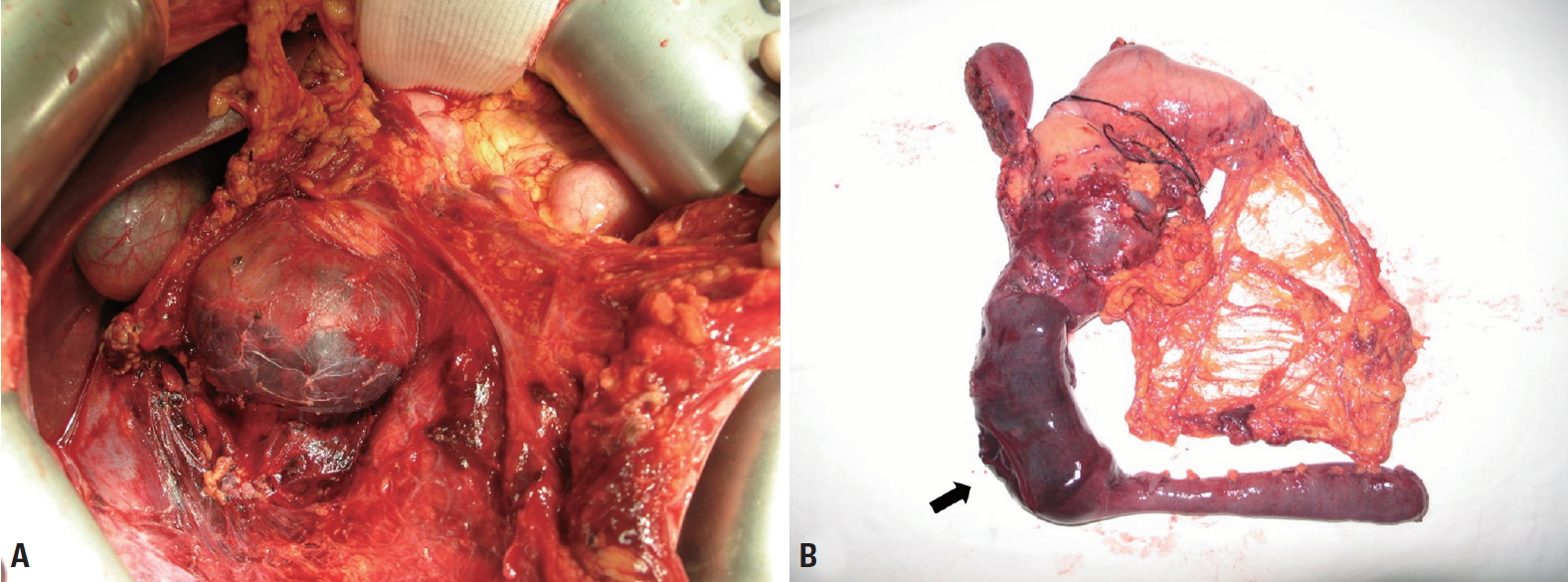
A 17-year-old boy who abruptly presented with severe epigastric pain and several episodes of biliary vomiting the day before admission was admitted to an emergency department after being diagnosed with a duodenal injury on abdominal computed tomography (CT) at a local hospital. Although he had been kicked in the abdomen during a violent tackle in a soccer game 8 days prior, the patient had no symptoms immediately after the injury. Upon arrival, the patient’s vital signs included a blood pressure of 120/70 mmHg, a pulse of 110 beats/min, a respiratory rate of 20 breaths/min, and a body temperature of 37.4°C. The physical examination revealed no palpable mass, but decreased bowel sounds, severe tenderness, and rebound tenderness on the upper abdomen. The initial upright abdominal X-ray did not show signs of free air. The patient’s laboratory data upon arrival were as follows: white blood cell count, 8,280/µL; hemoglobin, 13.5 g/dL; platelet count, 143,000; total bilirubin, 1.84 mg/dL; aspartate aminotransferase, 27 IU/L; alanine aminotransferase, 11 IU/L; amylase, 43 IU/L; and lipase, 26 IU/L. The coagulation test was normal. Abdominal CT showed a large hematoma (11×8 cm) in the third and fourth portions of the duodenum without any extraluminal air or abnormal fluid collection (Fig. 1). Approximately 4 hours after admission, however, the patient presented a high fever (above 38°C), aggravated pain throughout the entire abdomen, and severe rebound tenderness with muscle guarding. Since ultrasonography (US) was not available at night in the hospital, an abdominal US examination could not be performed. Based on acutely worsening physical examination findings with a high fever, we assumed the possibility of micro-perforation of the duodenum, rather than simple intramural hematoma, and performed an exploratory laparotomy. The emergency laparotomy revealed an intramural hematoma (13×9 cm) in the third and fourth portions of the duodenum without perforation of the duodenum or other organ injury (Fig. 2). After dissection of the duodenum by the Kocher maneuver, we made an incision on the anterior wall of the third portion of the duodenum to reveal an intramural hematoma, which we manually evacuated. The mucosa was intact with no evidence of perforation, and no source of active bleeding was identified. We identified no more bleeding at the injury site, and carried out primary repair of the serosa of the duodenum. On the third postoperative day, the patient developed unexpected severe abdominal pain, accompanied by a change of the Jackson-Pratt drain from serous to sanguineous. His hemoglobin level dropped from 11.6 g/dL to 8.8 g/dL over the course of 2 hours. Abdominal CT with contrast showed hemoperitoneum and distension of the second and third portions of the duodenum with intraluminal bleeding. We performed a reoperation with the suspicion of rupture of the surgical site and bleeding (Fig. 3). In the second operation, we identified a hemoperitoneum of 2,500 mL, a hematoma extending from the first portion of the duodenum to the proximal jejunum 7 cm distal from the Treitz ligament, and longitudinal tearing of the jejunum under the Treitz ligament with active bleeding (Fig. 4). We performed a pancreatoduodenectomy (Whipple operation), not a pylorus-preserving pancreatoduodenectomy, due to the hematoma in the upper and lower parts of the pylorus of the stomach. After the second operation, the patient’s diet gradually progressed after 6 days, after which no complications occurred. The patient was discharged on the 20th day after the second operation.

Initial abdominal computed tomography showed a huge intramural hematoma in the third and fourth portions of the duodenum. (A) Axial image. (B) Coronal image.
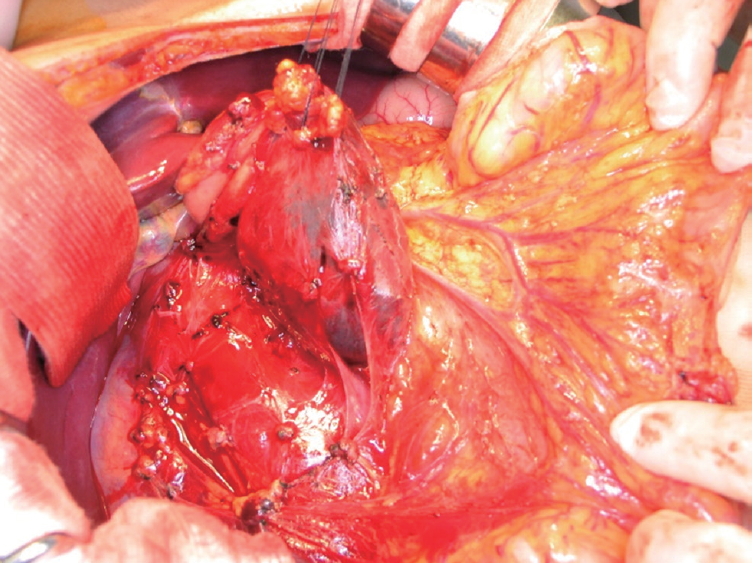
A photograph from the first operation shows intramural hematoma of the third and fourth portions of the duodenum.
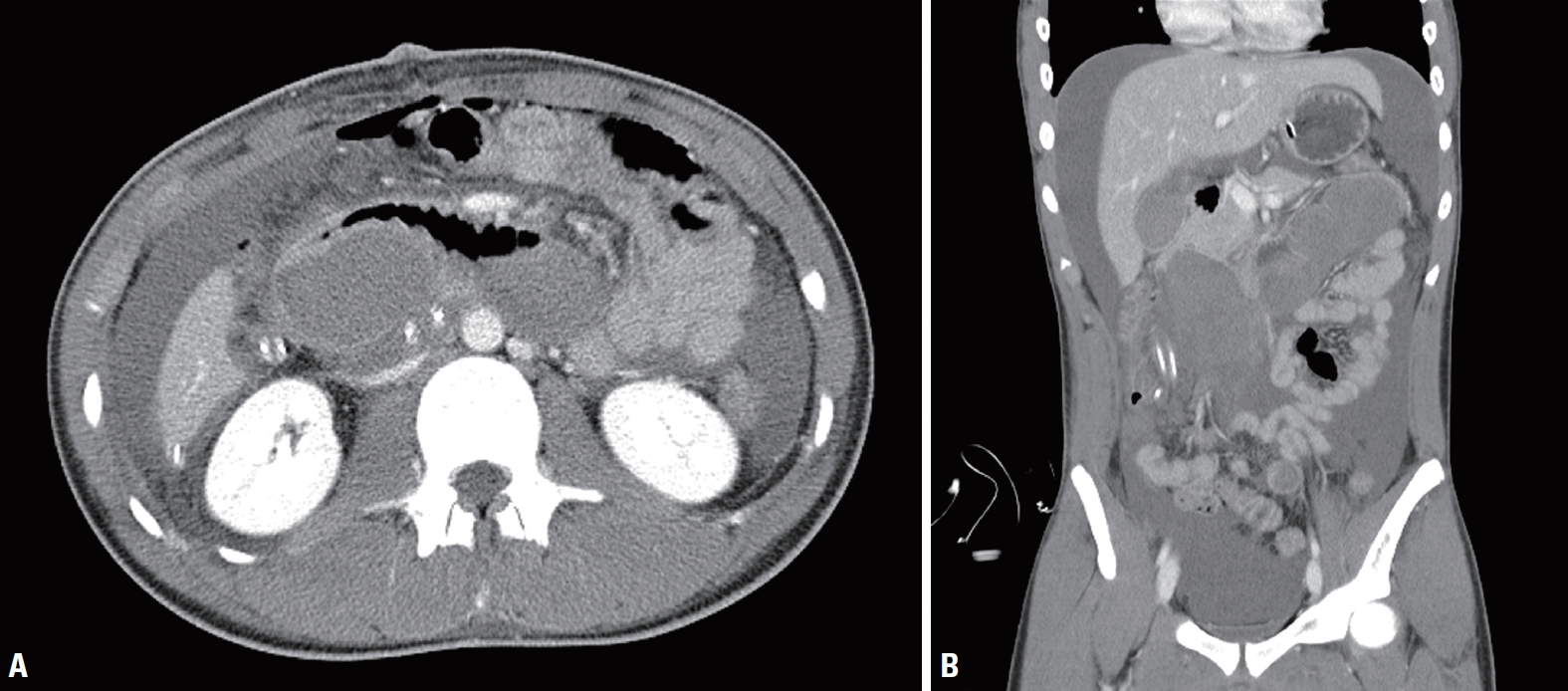
On the third postoperative day, follow-up abdominal computed tomography showed an intramural hematoma in the second and third portions of the duodenum with hemoperitoneum. (A) Axial image. (B) Coronal image.
DISCUSSION
The incidence of duodenal injury after abdominal trauma ranges from 3.7% to 5%. Penetration and blunt injuries have been reported to account for 78% and 22% of duodenal injuries, respectively [4]. In Korea, however, duodenal injuries are mainly caused by blunt abdominal trauma because of the very rare occurrence of gunshot injuries [5]. Most intramural duodenal hematomas are caused by blunt trauma, but uncommon non-traumatic causes include anticoagulant therapy, bleeding disorders, pancreatitis, and endoscopic interventions [6]. Although intramural hematoma caused by abdominal trauma can occur in the intestinal wall anywhere in the gastrointestinal tract, it most frequently develops in the duodenal wall, especially in the second and third portions of the duodenum [7]. The duodenum is a frequent site of hematoma because it is vulnerable to blunt abdominal trauma due to its fixed location in front of the spine, its lack of a mesentery, and its proximity to the spine (especially of the horizontal portion) [8]. In addition, because of the abundance of blood vessels in the duodenum, a hematoma in the subserosa layer of the duodenum can easily be formed by slow bleeding from small vessels when they are injured [5]. In our case, we assume that the intramural hematoma in the third and fourth portions of the duodenum, which were compressed between the abdominal wall and the spine, occurred after a violent tackle during a game of soccer.
Most patients with an intramural duodenal hematoma present with nonspecific symptoms, including abdominal pain that persists immediately after the trauma and vomiting that occurs approximately 1 to 2 days after the trauma. Furthermore, epigastric abdominal tenderness usually occurs 2 to 3 days before admission, and an obstruction of the duodenum or small bowel develops as hematoma gradually grows because the liquefaction of the hematoma results in increased osmotic pressure [9]. The presence of an intestinal obstruction induces several secondary complications, including pancreatitis, cholangitis, and sepsis, which can lead to death. Other symptoms include dehydration, mild fever and tachycardia, palpable mass, uncommon hematemesis or hematochezia, and occasionally anemia or hypovolemic shock when bleeding is profuse [7]. In our case, the patient complained of sudden acute abdominal pain and bilious vomiting roughly 7 days after trauma. Although an obstruction was identified, there was no secondary pancreatitis or cholangitis from the intestinal obstruction.
Because of the nonspecific clinical symptoms and the retroperitoneal position of intramural hematoma, the diagnosis is difficult and is frequently delayed, especially when the second and third portions of the duodenum are injured. For many years, an upper gastrointestinal series was widely used for the diagnosis of intramural duodenal hematoma. “Coil-spring” signs of partial intussusception of the small bowel are found towards the distal end of an intramural hematoma, but this modality is no longer routinely used to evaluate trauma patients due to its low sensitivity (19%) [7]. Abdominal CT is the primary imaging modality for diagnosing intramural duodenal hematoma, with its characteristic findings including duodenal wall thickening, heterogeneous attenuation in the wall, periduodenal fluid, fluid in the pararenal space, and various degrees of obstruction [10]. However, it is sometimes difficult to distinguish an intramural duodenal hematoma from duodenal perforation, since extraluminal air is not always identified in cases of traumatic duodenal perforation. In addition, extraluminal fluid collection without solid organ injury can occur in both duodenal perforation and duodenal hematoma [8]. Abdominal US is useful for diagnosing duodenal hematoma and is also suitable for following up patients who receive conservative management [11]. It has recently been reported that esophagogastroduodenoscopy (EGD) or magnetic resonance imaging (MRI) can be used to establish the location, size, and relationship with surrounding organs of a duodenal hematoma [12]. Because the diagnostic accuracy of traumatic duodenal injury is low, it may be diagnosed by means of an exploratory laparotomy if a high degree of suspicion of duodenal injury continues. Because of the special anatomy of the duodenum, the rate of misdiagnosis during surgery can be 20% or more, so open laparotomy is needed rather than diagnostic laparoscopy [13]. In this case, the patient showed no evidence of duodenal perforation, including periduodenal fluid and extraluminal air, except for the intramural duodenal hematoma on abdominal CT. However, we conducted an exploratory laparotomy because we could not rule out duodenal perforation, given the delayed manifestation of symptoms and the acute deterioration of abdominal pain and physical examination findings.
The primary recommended treatment option is conservative management, which includes nasogastric decompression, bowel rest, analgesia, and supportive therapy with intravenous fluids and parenteral nutrition [1,5,7]. Although the time required for liquefaction of a hematoma varies, most duodenal hematomas resolve spontaneously within 5 to 14 days after injury [10]. If an intestinal obstruction persists for more than 7 to 10 days after trauma, surgery may be necessary because of the proliferation of fibrous tissue around the hematoma. Early reports have proposed that hematoma evacuation with or without a bypass procedure may be an appropriate treatment for duodenal intramural hematoma. However, the current consensus is that surgical treatment should be considered if the hematoma is partially absorbed after 5 days or not completely absorbed after 10 days of conservative therapy, and exploratory laparotomy is required if duodenal perforation is suspected [14]. An intramural duodenal hematoma is resolved by the following surgical steps: incision of the serosa without violating the mucosal layer of the duodenum, evacuation of the intramural hematoma, and primary repair of the bowel wall, which results in rapid improvement of the intestinal obstruction. Complex duodenal injuries may require a pyloric exclusion and gastrojejunostomy to allow healing of the duodenal repair and prevent complications [15]. The mortality rates for traumatic duodenal injuries range from 6% to 25%, and the incidence rates of complications, such as intra-abdominal abscess, enteroenteric or enterocutaneous fistula, respiratory failure, sepsis, and acute renal failure, range from 30% to 60% [8]. Missed injuries or delayed diagnoses lead to many complications, and surgical therapy becomes more difficult if the injury is recognized late. In our case, the duodenal perforation was not found in the first operation, so we performed hematoma evacuation. In the second operation, there was proximal jejunal tearing with active bleeding distal to the Treitz ligament. We assumed that the recurrent bleeding was caused by a delayed pancreaticoduodenal perforating arterial hemorrhage. The following limitations should be considered regarding our case. First, although the patient’s symptoms acutely worsened, short-term abdominal CT or EGD should have been considered to recheck or confirm whether duodenal perforation was present because he was hemodynamically stable. Second, after confirming that the duodenum was not perforated, we should have considered conservative therapy, not hematoma removal in the first operation. Finally, due to a lack of clinical experience with traumatic duodenal injury, we did not consider performing a pyloric exclusion and gastrojejunostomy as damage control surgery.
We report a rare case of delayed manifestation of an isolated intramural hematoma of the duodenum following blunt abdominal trauma. In a patient with blunt abdominal trauma presenting with epigastric pain, nausea, and persistent bilious vomiting, an intramural hematoma should be ruled out. If diagnosis is inconclusive, a serial or additional exam, such as EGD, abdominal CT, US, or MRI, should be performed. Exploratory laparotomy remains the final diagnostic test if a high suspicion of duodenal injury continues after additional examinations are performed.