Comparison of Magnetic Resonance Imaging and Operation Waiting Times in Patients Having Traumatic Cervical Spinal Cord Injury; with or without Bony Lesions
Article information
Abstract
Purpose
To compare the time intervals to magnetic resonance imaging (MRI) and surgical treatment in patients having traumatic cervical spinal cord injury (SCI) with and without bony lesions.
Methods
Retrospectively analyzed adult patients visited Kyungpook National University Hospital and underwent surgical treatment for cervical SCI within 24 hours. The patients who were suspected of having cervical SCI underwent plain radiography and computed tomography (CT) upon arrival. After the initial evaluation, we evaluated the MRI findings to determine surgical treatment. Waiting times for MRI and surgery were evaluated.
Results
Thirty-four patients were included. Patients’ mean age was 57 (range, 23-80) years. Patients with definite bony lesions were classified into group A, and 10 cases were identified (fracture-dislocation, seven; fracture alone, three). Patients without bony lesions were classified into group B, and 24 cases were identified (ossification of the posterior longitudinal ligament, 16; cervical spondylotic myelopathy, eight). Mean intervals between emergency room arrival and start of MRI were 93.60 (±60.08) minutes in group A and 313.75 (±264.89) minutes in group B, and the interval was significantly shorter in group A than in group B (p=0.01). The mean times to surgery were 248.4 (±76.03) minutes in group A and 560.5 (±372.56) minutes in group B, and the difference was statistically significant (p=0.001). The American Spinal Injury Association scale at the time of arrival showed that group A had a relatively severe neurologic deficit compared with group B (p=0.046). There was no statistical significance, but it seems to be good neurological recovery, if we start treatment sooner among patients treated within 24 hours (p=0.198).
Conclusions
If fracture or dislocation is detected by CT, cervical SCI can be easily predicted resulting in MRI and surgical treatment being performed more rapidly. Additionally, fracture or dislocation tends to cause more severe neurological damage, so it is assumed that rapid diagnosis and treatment are possible.
INTRODUCTION
The incidence of traumatic spinal cord injuries (SCIs) in the United States is approximately 54 per million people; around 17,700 cases, excluding those that involve deaths at the scene of the accident, occur annually [1].
Damage at the level of the cervical spine is the most common type of SCI and is associated with a high mortality rate [2]. The development of computed tomography (CT) and magnetic resonance imaging (MRI) has aided in the diagnosis and evaluation of SCIs [3]. Among adult patients with SCIs, 75% were reported to have fracture dislocation, dislocation only, or a burst fracture, and 25% of patients had only minor fractures without definite lesions (including compression fracture), SCI without radiological abnormality, and SCI without obvious radiological evidence of trauma [4]. In the presence of cervical spinal stenosis, traumatic SCI may occur without fracture or dislocation [5]. The most common cause of cervical spinal stenosis is cervical ossification of the posterior longitudinal ligament (OPLL) and cervical spondylotic myelopathy (CSM) [6–8]. In cervical spinal stenosis, the anteroposterior diameter of the spinal canal is a significant risk factor for the development of SCI [8–10].
If cervical SCI occurs, surgical treatment within 24 hours is reported to improve the prognosis [11–13]. The role of MRI in diagnosing and treating SCI is very important [14,15]; in particular, if there is cervical spinal stenosis without bony fracture or dislocation, MRI plays an essential role in deciding the mode of surgical treatment. In this study, we retrospectively compared the time intervals to MRI and surgical treatment in patients with a cervical SCI with and without definite bony lesions detected using CT. We hypothesized that MRI imaging and treatment would be delayed in patients with spinal cord injuries that are not readily diagnosed by CT.
METHODS
We retrospectively analyzed patients who had been diagnosed with SCI and underwent surgical treatment from 2012 to 2018 in Kyungpook National University Hospital. The inclusion criteria were adult patients aged between 18 and 80 years and a neurological level of injury between C2 and T1. The exclusion criteria were patients with a high degree of instability in whom it was impossible to use MRI, those in whom it was difficult to perform an accurate neurological examination (e.g., patients with concomitant brain hemorrhage, a history of previous neurological deficit, and combined fracture of the extremity), those who were transferred to Kyungpook National University Hospital after radiological evaluation, and those in whom surgical treatment within 24 hours could not be performed.
If patients were suspected of having cervical SCI, CT was performed immediately in the emergency room followed by a neurological examination. The neurological status at the time of arrival to the emergency room was evaluated using the American Spinal Injury Association (ASIA) impairment scale. If cervical SCI was suspected, MRI was performed preoperatively. CT and MRI findings were analyzed using the Picture Archiving and Communication System (π view; Infinitt, Seoul, Korea).
The time interval between arrival to the emergency room and initiation of the MRI and emergency operation was calculated from the medical records. Patients were divided into two groups, those with definite bony lesions (with fracture-dislocation or fracture only detected by CT) and those without definite lesions.
This study was approved by Kyungpook National University Hospital Institutional Review Board (IRB No. 2018-12-014).
Statistical analysis
For statistical analysis, SPSS 17.0 (SPSS, Inc., Chicago, IL, USA) was used. Data was tested for normality and the independent t-test was used to analyze differences between the two patient groups. A p-value <0.05 was considered statistically significant.
RESULTS
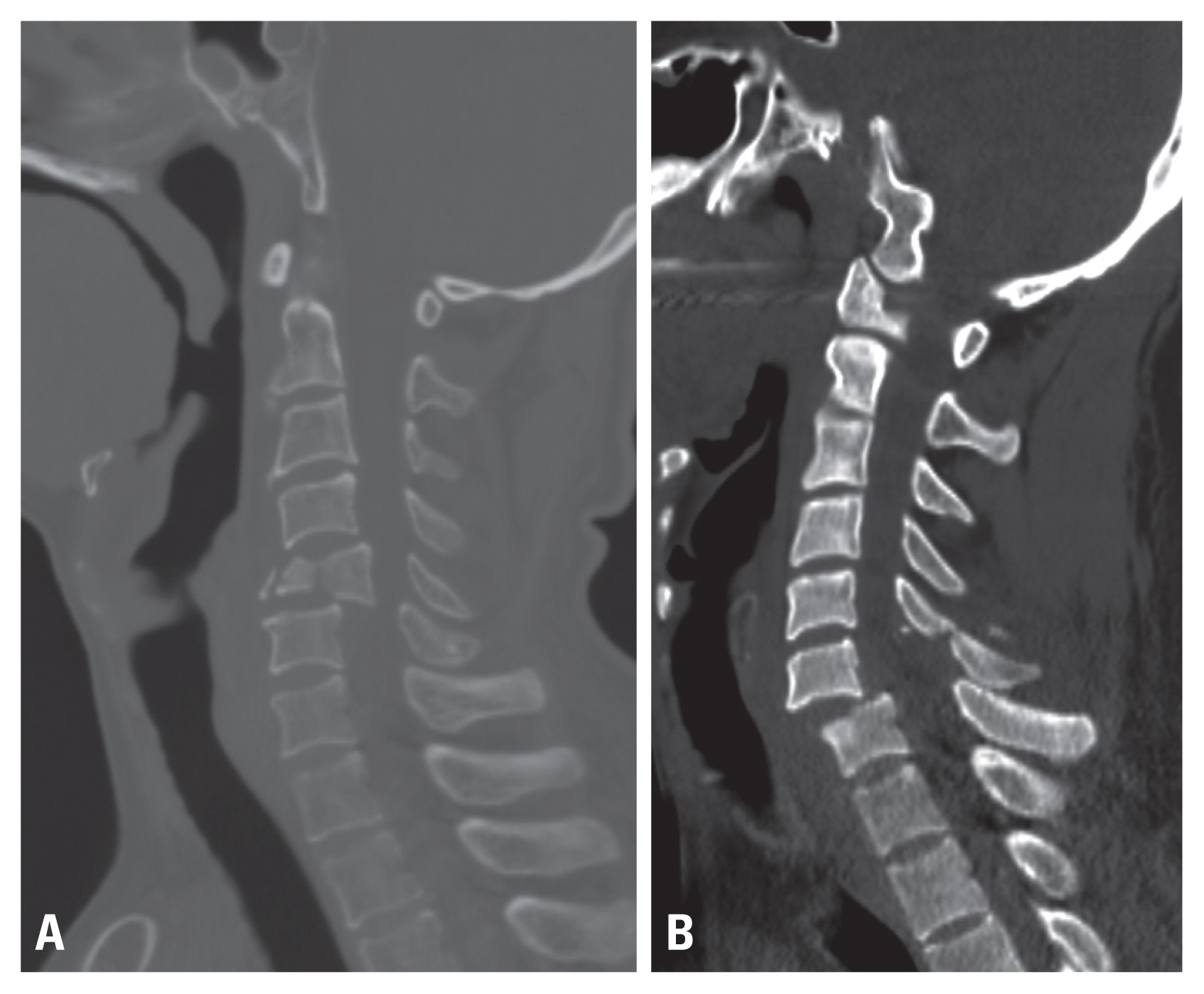
Thirty-four patients were included in the study. The patients’ mean age at the time of injury was 57 (range, 23–80) years, and the male-to-female ratio was 31:3. Ten patients with definite bony lesions (fracture-dislocation, seven; fracture only, three) were identified and classified into group A (Fig. 1). Twenty-four patients without bony lesions (OPLL, 16; CSM, eight) were identified and classified into group B (Fig. 2). The time intervals from arrival to the emergency room to the time of MRI were 93.60 (±60.08) mins in group A and 313.75 (±264.89) mins in group B. The time to MRI was significantly shorter in group A than in group B (independent t-test, p=0.01). The times to surgery were 248.40 minutes (±76.03) in group A and 560.50 minutes (±372.56) in group B. The time to start of surgical treatment was significantly shorter in group A than in group B (independent t-test, p=0.001). In both groups, the times to MRI and surgical treatment followed a normal distribution (Table 1).
Computed tomography images of spinal cord injury with bony lesion (A) with burst fracture. (B) With fracture-dislocation injury.

Computed tomography images of spinal cord injury without bony lesion (A) with cervical spondylotic myelopathy. (B) With ossification of the posterior longitudinal ligament.
The ASIA impairment scale grades in group A at the time of arrival in the emergency room were A in four patients, B in three patients, C in two patients, and D in one patient. The ASIA impairment scale grades in group B were A in five patients, B in three, C in five, and D in 11. The independent-sample t-test showed that in comparison to patients in group B, those in group A had a statistically significant tendency to have severe neurologic deficits (p=0.0468) (Table 2).
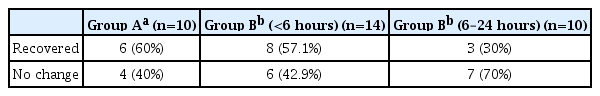
In group A, all patients except one case underwent surgical treatment within 6 hours of arrival (248.40 [±76.03] minutes). In Group B, 14 patients underwent surgical treatment within 6 hours (mean, 264.40±57.54 minutes), and ten patients underwent surgical treatment between 6 and 24 hours (mean, 900.30±287.64 minutes). In group A, six cases (60%) showed postoperative improvement of neurological status, as measured by the ASIA scale; however, the other four cases (40%) remained unchanged. In group B, 11 cases (45.8%) showed recovery of the ASIA scale and 13 cases (54.2%) showed no change. When looking specifically at the 14 cases of surgical treatment within 6 hours in group B, eight cases (57.1%) showed an improvement in the ASIA scale whereas six cases (42.9%) showed no change. However, in the patients who underwent surgical treatment within 6 to 24 hours, the ASIA scale improved in three patients and seven showed no change. Therefore, in group B, there was no significant difference in the recovery of neurological status according to the difference in operative treatment delay time (p=0.198) (Table 3).
DISCUSSION
In order to ensure early surgical treatment SCIs, imaging studies are necessary, followed by an MRI; however, MRI is usually time consuming. In general, MRI evaluation is performed according to the priority of the injury. If MRI is delayed, the time interval to starting surgical treatment tends to be longer.
This study found that the time to perform MRI in the group without bony lesion was significantly longer resulting in surgical treatment being delayed. Although no statistical significance was shown, in the group without bony lesions, surgical treatment within 6 hours tended to result in increased recovery of neurological symptoms. Therefore, our results indicate that outcomes were more favorable if surgical treatment is performed relatively quickly, even within 24 hours.
CT is one of the most common imaging modalities that can be performed immediately in the emergency room. When a bony lesion is detected via CT, it is easy to assume that cervical SCI is present, and the examination is likely to proceed more rapidly. In addition, bony lesions are significantly more likely to be associated with neurological symptoms, which may help to predict cervical SCI. In the absence of bony lesions, cervical SCI occurs mainly when OPLL or CSM is present [5–8].
The Torg-Pavlov ratio is the value of the anteroposterior diameter of the spinal canal at the mid-vertebral level divided by the anteroposterior diameter of the vertebral body at the same level [16,17] (Fig. 3). Normally, the ratio is 1.0, but if the value is smaller, it is possible that cervical spinal stenosis is underway. In particular, when the ratio is less than 0.7, it has been reported that cervical spinal stenosis is related to SCI [18]. Additionally, if the midsagittal canal diameter is less than 13 mm at the C3 to C7 level, cervical spinal stenosis is often suspected [19] (Fig. 4). In patients without bony lesions, such as fracture-dislocation and suspected cervical SCI, the Torg-Pavlov ratio or midsagittal canal diameter should be measured to determine if there is a risk factor for the development of SCI, and MRI should be performed more rapidly so that surgical treatment can be performed early.

Torg-Pavlov ratio: B/A. Anteroposterior diameter of the vertebral body, A. Anteroposterior diameter of the spinal canal, B.
This study has several limitations. First, the level of cervical SCI was not considered. Second, age, sex, neurological status, and underlying disease were not controlled for in the patient groups. Third, there may be a difference in the protocol for evaluating SCI patients in other institutes; therefore, it is difficult to interpret these results as representative of all SCI patients.
CONCLUSION
If fracture or dislocation is detected by CT, cervical SCI can be easily predicted resulting in MRI and surgical treatment being performed more rapidly. Our results suggest that surgical treatment within 6 hours is likely to result in increased neurological symptom recovery, although this finding was not significant. Further studies are required to explore this association further.