Articles
- Page Path
- HOME > J Trauma Inj > Volume 30(4); 2017 > Article
-
Case Report
Common Carotid Artery Laceration Managed by Clamping at Emergency Department - Young Un Choi, M.D.1, Kwangmin Kim, M.D.2, Seongyup Kim, M.D.2, Keumseok Bae, M.D.2, Ji Young Jang, M.D.2, Pil Young Jung, M.D.2, Hongjin Shim, M.D.2, Ki Youn Kwon, M.D.3
-
Journal of Trauma and Injury 2017;30(4):197-201.
DOI: https://doi.org/10.20408/jti.2017.30.4.197
Published online: December 30, 2017
- 19,045 Views
- 92 Download
1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
2Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
3Department of Orthopedic Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
- Correspondence to: Hongjin Shim, M.D., Trauma and Surgical Critical Care, Department of Surgery, Yonsei University College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea, Tel: +82-33-741-0990, Fax: +82-33-741-0574, E-mail: simong3@yonsei.ac.kr
• Received: September 7, 2017 • Revised: December 7, 2017 • Accepted: December 7, 2017
Copyright © 2017 The Korean Society of Trauma
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Common carotid artery laceration is a life-threatening injury by causing hypovolemic shock. Nevertheless the initial management is very difficult until definitive surgery at operation room. Before neck exploration at operation room, arterial bleeding control by compressing the bleeding point is not always effective. We experienced one case with externally penetrating injuries in zone II neck, which was operated after clamping of common carotid artery in the emergency department. Here we report this case.
- Common carotid laceration is lethal and hard to control. Even more that, neck laceration of Zone II is very hard to approach in emergency department (ED). If the condition of patient is in hypovolemic shock by massive bleeding, it makes worse causing coagulopathy with hypothermia and acidosis [1]. In this situation, bleeding control and patient management are very hard.
- We report the case that common carotid artery laceration with cardiac arrest managed by clamping at ED.
INTRODUCTION
- A 25-year-old man presented with hypovolemic shock after being stabbed in the left neck with a knife. The manual compression to injury site was applied until he was transported to trauma center. Interval time from accident to ED was 17 minutes, but the bleeding from injury site was severe. Even though pushing the injury site, there was cardiac arrest due to hypovolemic shock and manual cardiac massage was applied on arrival. At the same time, neck exploration was done in ED.
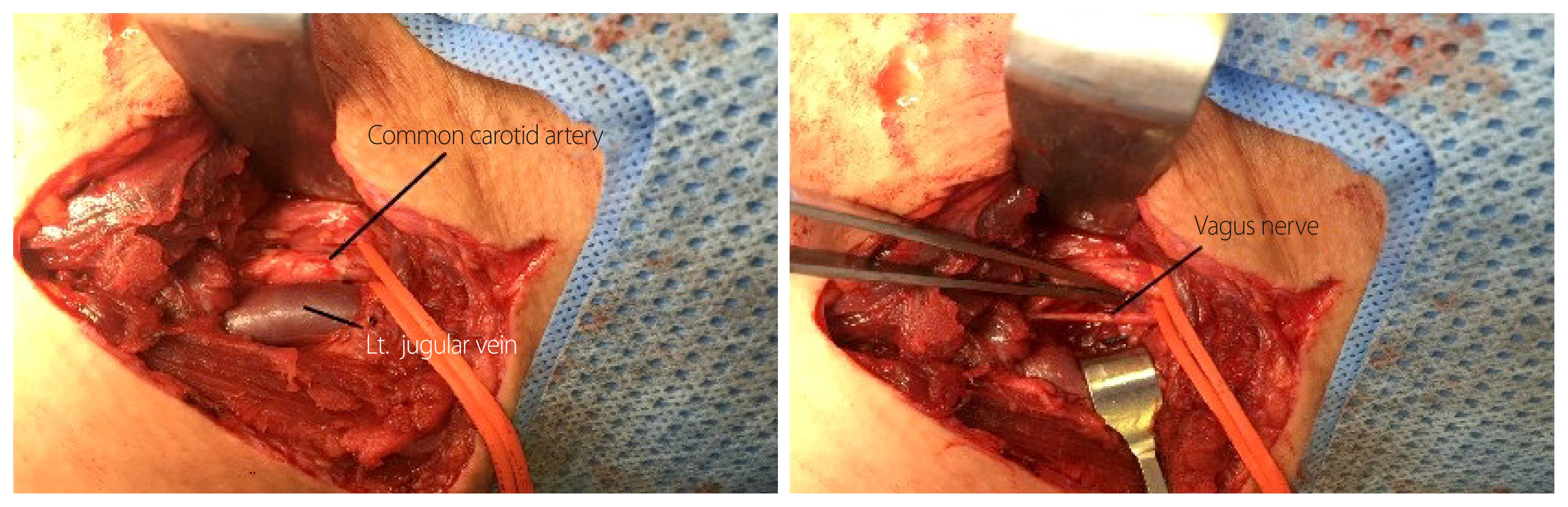
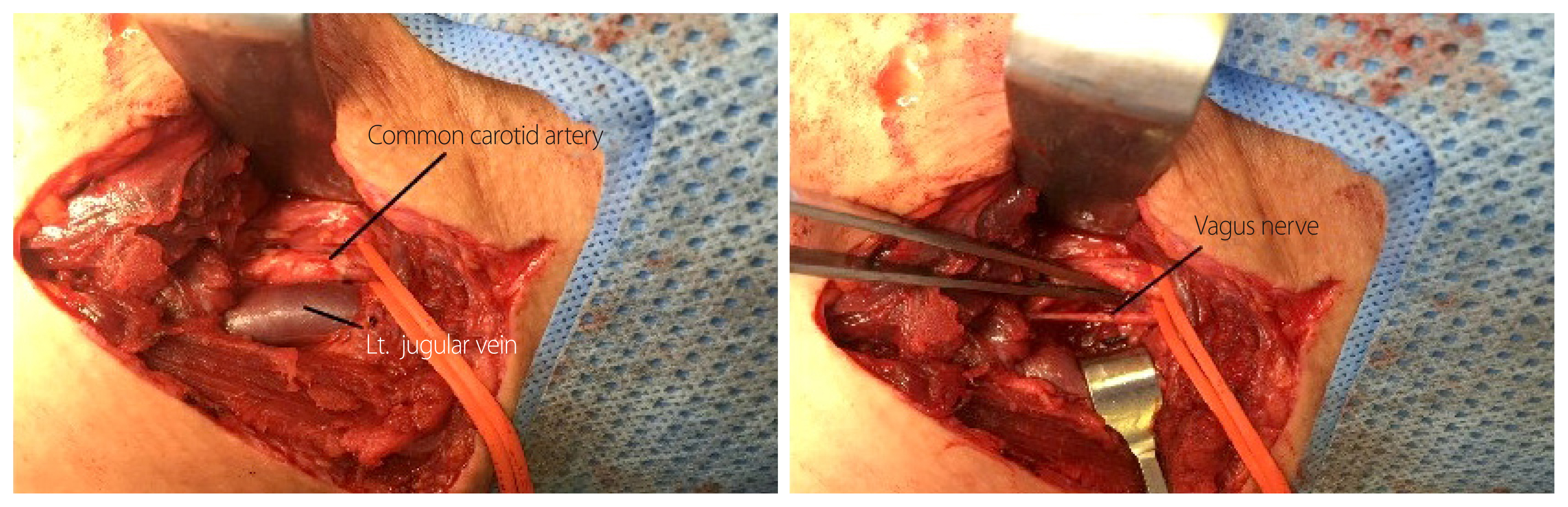
- Oblique skin incision along the anterior margin of left sternocleidomastoid muscle was applied and left common carotid artery was exposed. The left common carotid artery was cut 70% circumferentially and severe bleeding was controlled by clamping the proximal and distal site and then return of spontaneous circulation was accomplished (Fig. 1).
- Then, the patient was sent to operation room. There were common carotid artery laceration and complete rupture of the left vagus nerve. The internal jugular vein was intact. Laceration site was repaired with prolene 6-0 continuous suturing and neurorrhaphy were performed (Fig. 2). The time interval from injury to reperfusion was 40 minutes.
- We supplied eight packs of red blood cell (RBC) (2,000 mL), five packs of fresh frozen plasma (805 mL) and crystalloid (normal saline, 5,000 mL) at the ED and two packs of RBC and crystalloid (Hartmann’s solution, 2,450 mL) at operation room.
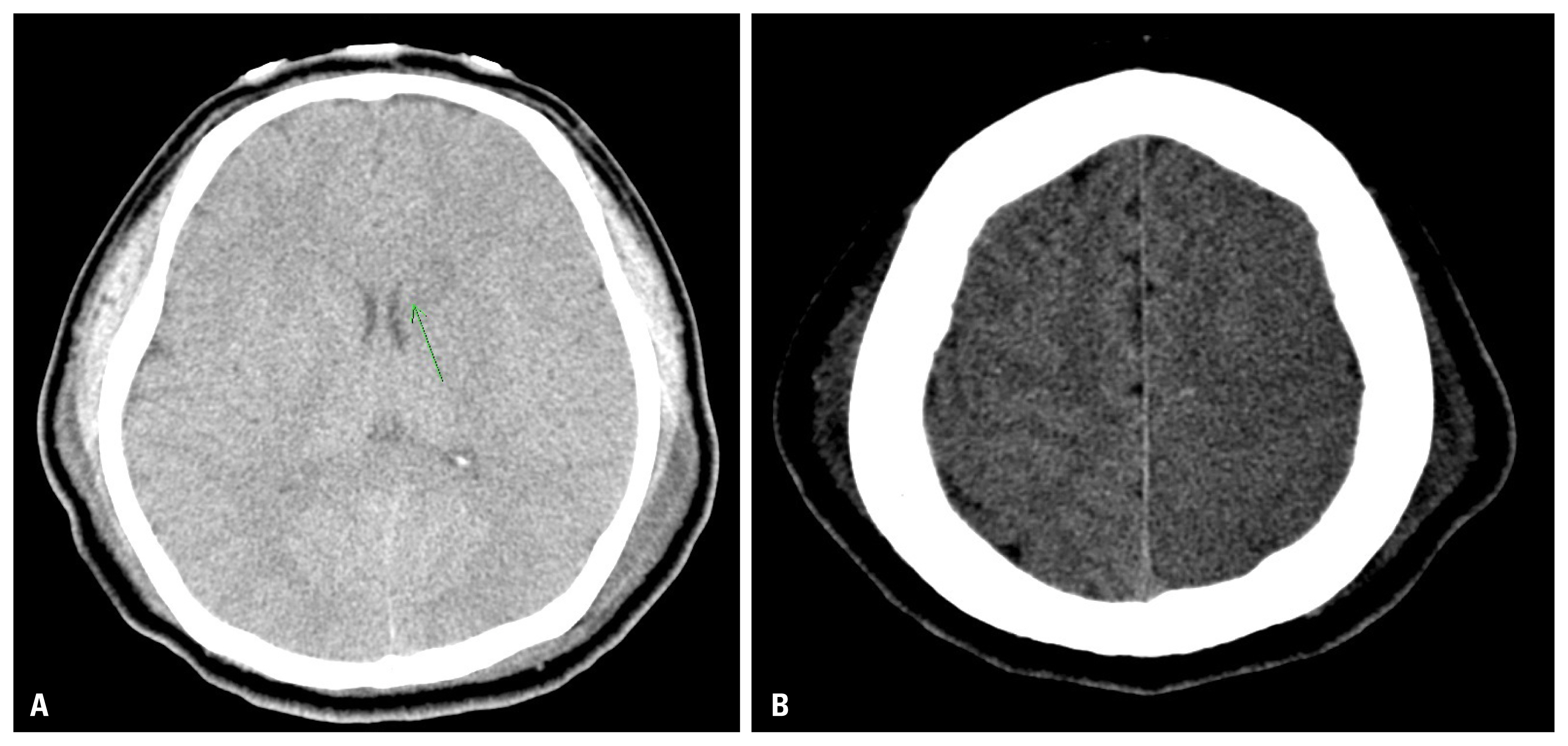
- After operation, the patient was moved to the trauma intensive care unit with intubated status and vital signs became stable. But mental status was coma and therapeutic hypothermia (<33°C) after cardiac arrest was applied for 2 days. After 48 hours, brain computed tomography (CT) with angiography scan showed c (Fig. 3). The patient showed right hemiplegia.
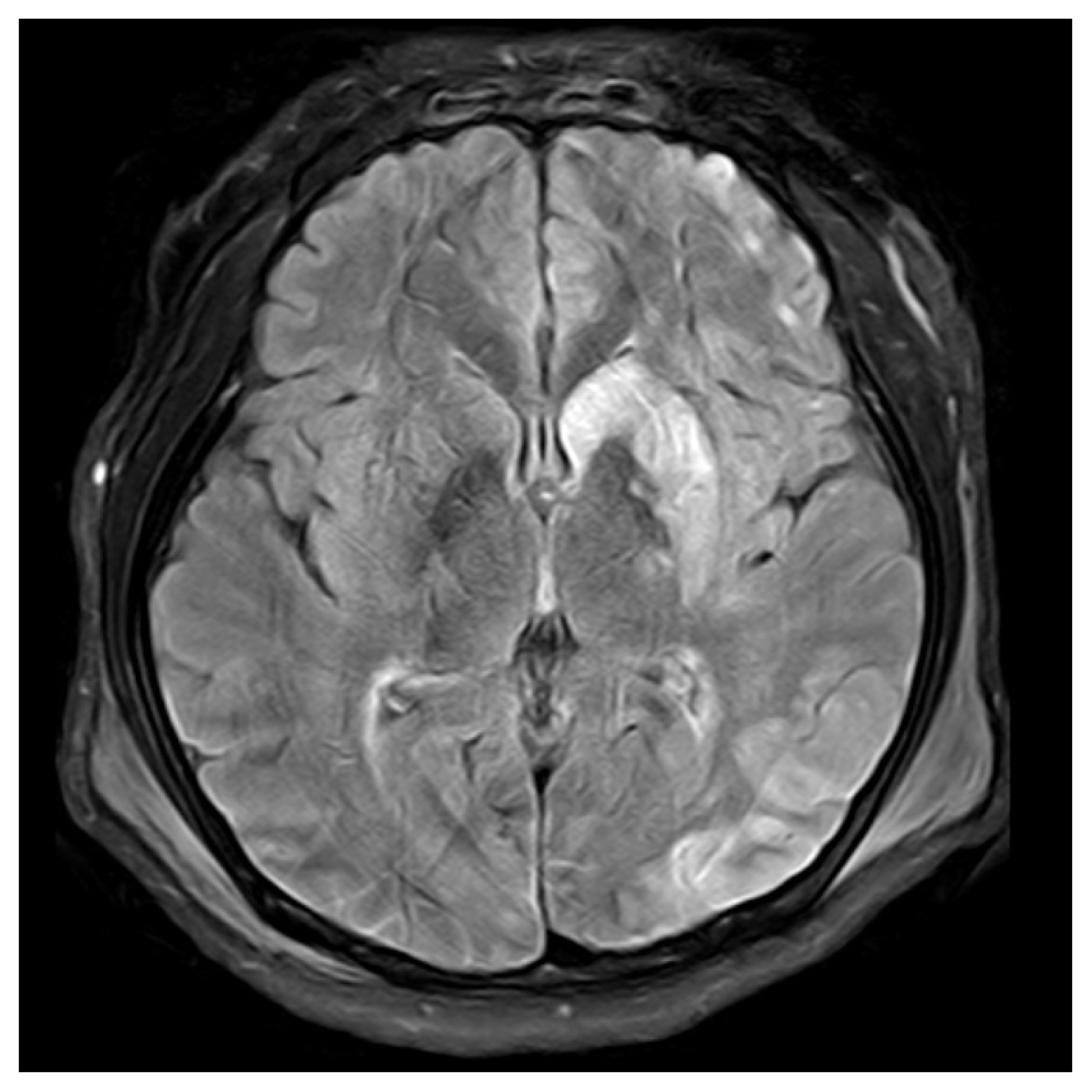
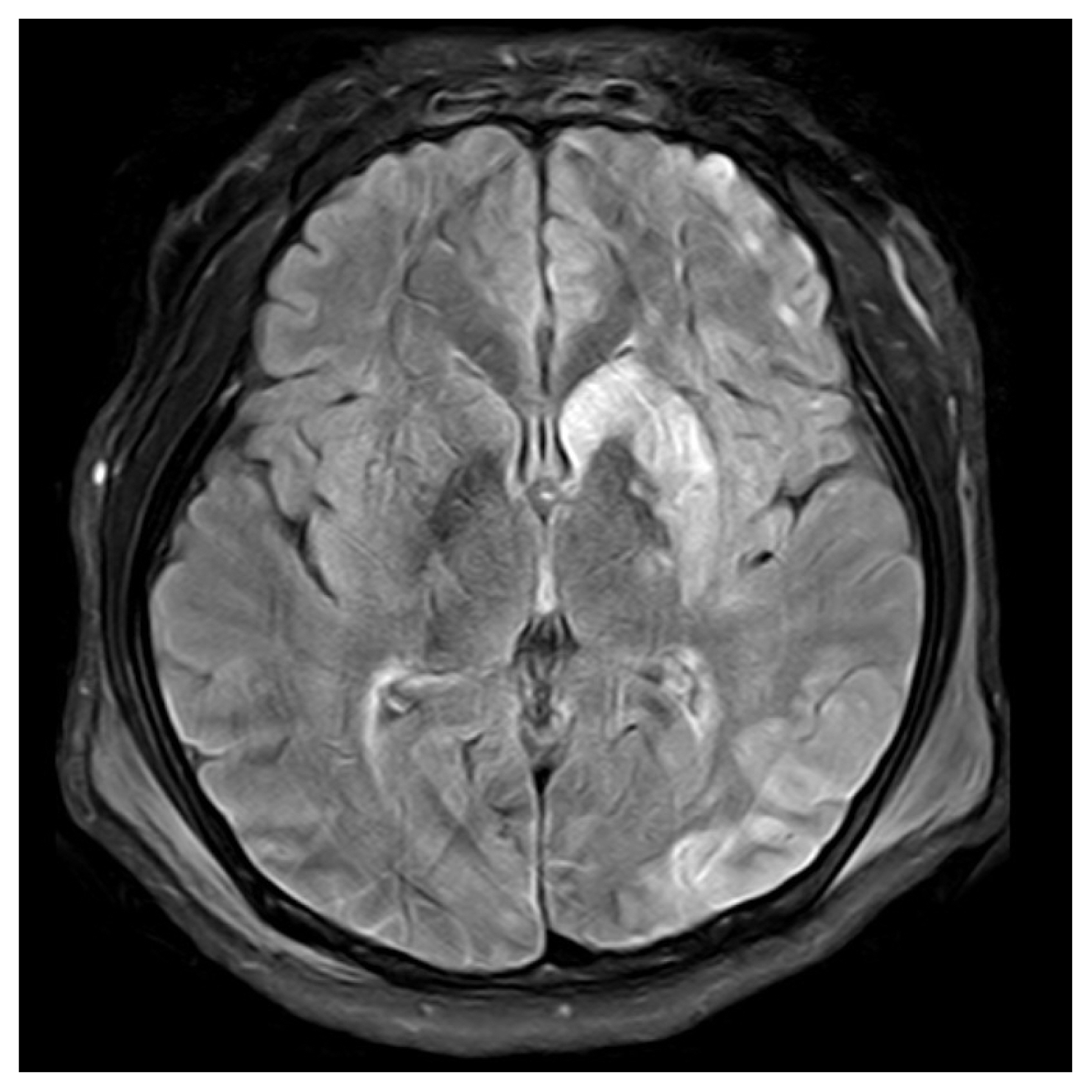
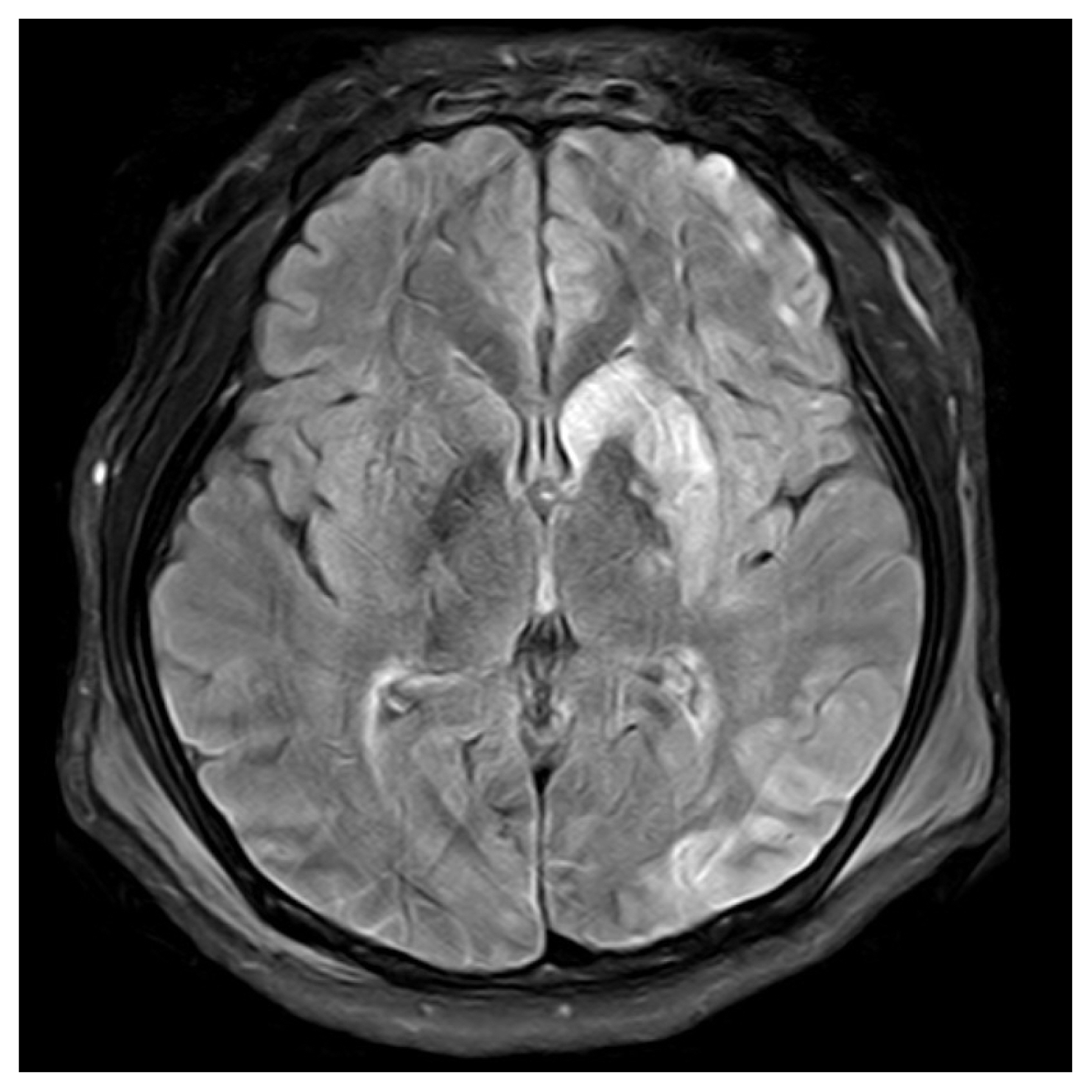
- Therapeutic hypothermia and sedative drugs were stopped. On postoperative day (POD) 3, the patient’s mentality changed to drowsy and it changed to alert in the next day. Brain magnetic resonance imaging scan on POD 4 showed same pattern with CT (Fig. 4). The patient was transferred to general ward on POD 9 and transferred to rehabilitation department on POD 18 for comprehensive rehabilitation including gait training, speech therapy and dysphagia management. On manual muscle test, right hemiplegia got better 12 days later from transferring. Shoulder, elbow and forearm, wrist, hip, knee and ankle level changed from zero to good or fair.
- On POD 45, follow-up carotid ultra sonography showed 50% stenosis and flow limitation (peak systolic velosity 216.2 cm/s) on anastomosis site which is not indicated for intervention and no new or worsening of neurologic deficit occurred.
CASE REPORT
- Major vascular injuries in the neck are frequently originated from penetrating trauma. Carotid artery injuries occur in about 17% of patients with penetrating neck trauma and the survival rate of penetrating carotid injuries is very low due to active arterial bleeding [2]. As it supplies major circulation for brain, the injury of carotid artery can induce a brain ischemia even though a small circulation of vertebral artery.
- In our case, the oblique skin incision along the anterior margin of left sternocleidomastoid muscle was applied and left common carotid was exposed. Bleeding control before exploration was manual compression with gauze and bleeding control after exploration at ED was clamping. Foley catheter insertion for temporary bleeding control has many advantages such as rare damage to vessel and convenience to apply and immediateness and so on. It can be applied when the wound is small or surgical approach is difficult.
- However that method can have some problems like migrating or even spontanous removing. Moreover the effective compression cannot be accomplished in case of major artery like this case.
- This case is neck zone II injury and surgical approach was possible. And the surgeon was at the emergency room field when the patient was transferred and the length of wound was over 10 cm. So, the Foley catheter insertion was decided to be inadequate method. The injury site was big (70% of circumference) and was exposed easily and shortly. That is why direct clamping was applied early.
- Patients with symptomatic zone II neck injuries should be undergone early operation for neck exploration [3]. In carotid artery injuries ligations, primary repair and interposition with saphenous vein/PTFE graft can be considered [4]. If technically possible, keeping vascular continuity is recommended in every patient without neurologic deficit [5]. But if the repair is impossible, vessel ligation would be chosen in spite of expected neurologic sequelae [6,7]. Vessel ligation can be applied in case of external carotid injuries and interposition with saphenous vein/PTFE graft can be applied in case of internal carotid injuries. Common carotid artery injuries can be managed by a combination of either a primary repair or interposition graft. Temporary shunt can be thought as an option, but shunt does not result in a decreased mortality rate or neurologic deficit reduction in patients with severe carotid artery injuries. Therefore carotid artery repair can be a choice [5]. In this case, laceration margin was so clear that PTFE graft was not indicated [8]. Moreover, massive bleeding from injury site and cardiac arrest due to hypovolemia made it impossible to perform a preoperative evaluation and to check neurologic deficit.
- The exploration, attempted suture and clamping of the vessel should be avoided in the field, and should not be undertaken until appropriate vascular surgical supports in general vessel injuries [9]. But the situation was urgent due to cardiac arrest and immediate surgical clamping of common carotid artery in ED was the only choice and it worked for hemostasis and ROSC. In case of devascularization to brain due to the injury of carotid artery, central neurologic deficit is a main concern after operation and revascularization may cause stroke as well. In the penetrating extracranial carotid artery trauma patients, mortality was 21.2% and stroke rate after survival was 15.1% [10]. Of course, the collateral circulation between vertebral artery and subclavian artery is well known [11]. However, it has many variations so that it is dangerous to trust the collateral and sacrifice common carotid artery. While common carotid artery occlusion, vertebrocarotid anastomosis distal to the bification of common carotid artery would keep the low flow to brain, however it is not enough. Moreover, contralateral blood flow can replace the lacking flow at the Wili’s circle [12]. But there are many kind of anastomosis variations and confirming the existence of variation before surgical management was impossible due to urgent situation. In general, the ligation of common carotid artery as a salvage procedure is recommended if the patient has a neurologic defect [13]. However, in the arrest situation, the ROSC time is the only clue of neurologic defect.
- After repair of carotid artery, brain ischemia was highly worried about because of the cardiac arrest due to hypovolemic shock in this case. However it seemed that thrombotic emboli were the main cause of cerebral infarction rather than hypoperfusion in the brain CT scan (Fig. 3). In this case, suturing the left common carotid artery, back flow from the distal artery was not enough when de-clamping. We suspect that it caused thromboembolism not to eliminate out of the vessels and distribute to distal-cerebral arteries. In the carotid endarterectomy operation, most strokes are induced by immediate postoperative thrombosis and embolus or delayed postoperative embolus than by the technical errors during placement of a shunt, endarterectomy, or carotid artery reconstruction [14]. We used prophylactic heparinization in operating room but stroke event was developed.
- Not only resuscitation but also control of bleeding focus is important in the acute management. Hisashi et al. point out the dogmatic custom that ‘The surgical operation must be done in the operation room (OR)” can lead very unfortunate result. Because there are multidisciplinary reasons such as coagulopathy due to time delay, operation room needing completion of several unavoidable hospital procedures, impossibility of patient’s transportation to OR and so on [13]. It means that urgent resuscitative surgery can be used in the urgent situation as a bridge technique if the ED is set for ED procedure.
- Therefore, when a patient is in lethal status including hypovolemic shock or cardiac arrest, ED exploration and clamping bleeder can be a bridge option for resuscitation and definitive operation.
DISCUSSION
Fig. 3(A) Brain CT with angiography scan: diffuse low density along the left cerebral hemisphere in is seen and indicator shows the low density along the left basal ganglia and left head of caudate nucleus with suspicious high density along the caudate nucleus. (B) Brain CT, followed with (A). CT: computed tomography.
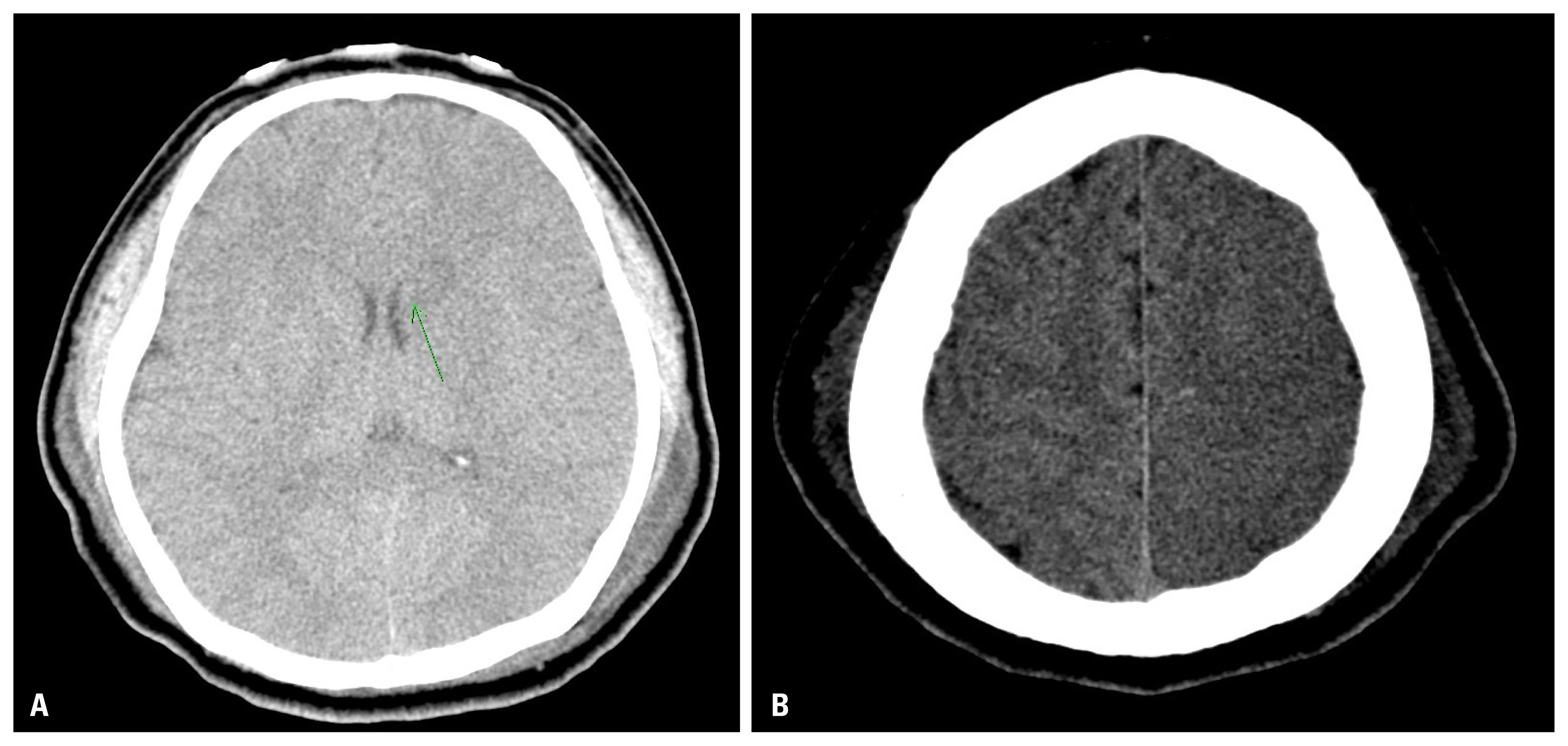
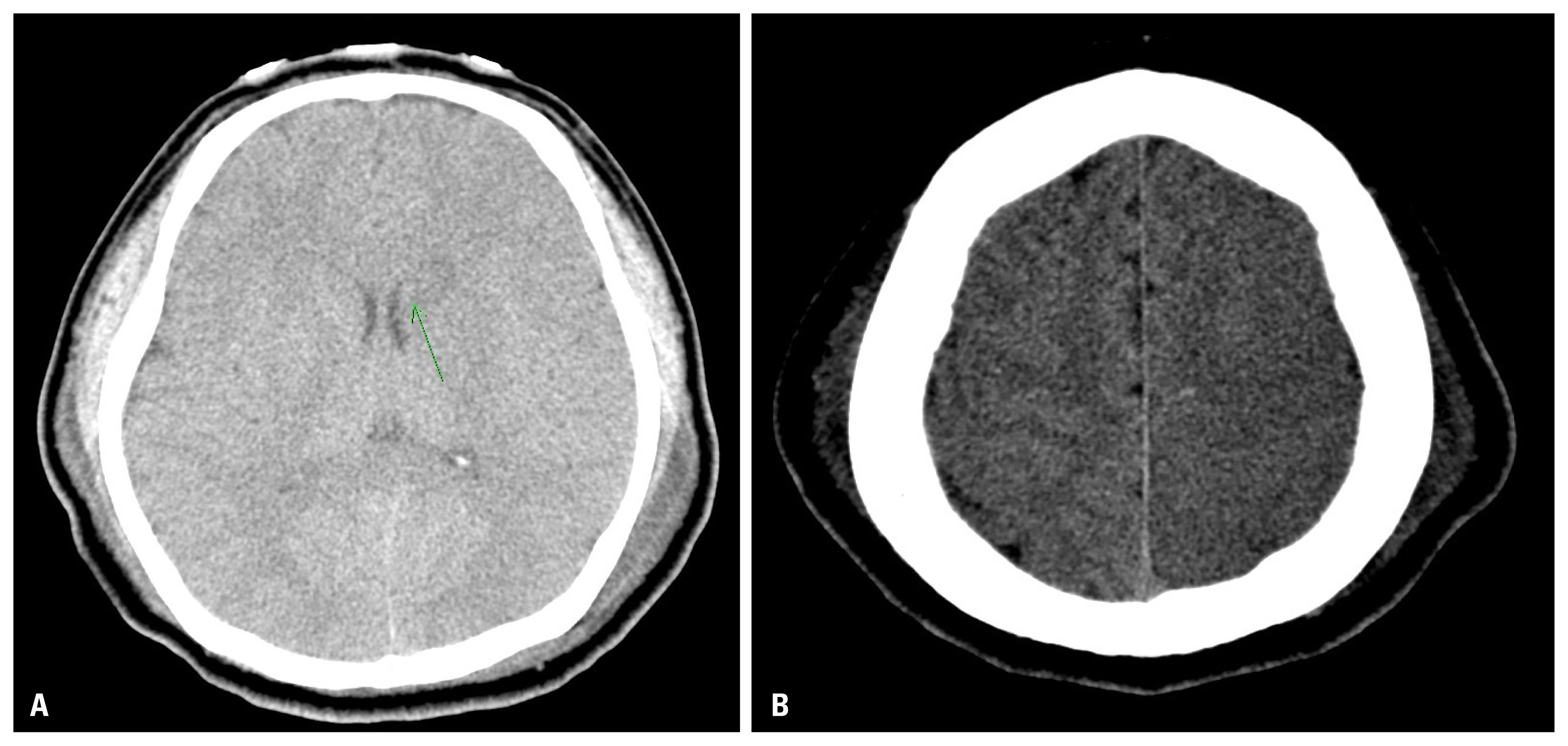
Fig. 4Brain magnetic resonance imaging scan on postoperative day 4, which showed high-signal intensity along the left frontotemporoparietal including occipital cortex and left caudate nucleus including left basal ganglia whose impression is a recent infarction.
- 1. Brohi K, Cohen MJ, Ganter MT, Schultz MJ, Levi M, Mackersie RC, et al. Acute coagulopathy of trauma: hypoperfusion induces systemic anticoagulation and hyperfibrinolysis. J Trauma 2008;64:1211–7; discussion 1217, ArticlePubMed
- 2. Mittal VK, Paulson TJ, Colaiuta E, Habib FA, Penney DG, Daly B, et al. Carotid artery injuries and their management. J Cardiovasc Surg (Torino) 2000;41:423–31. PubMed
- 3. Sperry JL, Moore EE, Coimbra R, Croce M, Davis JW, Karmy-Jones R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg 2013;75:936–40.ArticlePubMed
- 4. Navsaria P, Omoshoro-Jones J, Nicol A. An analysis of 32 surgically managed penetrating carotid artery injuries. Eur J Vasc Endovasc Surg 2002;24:345–55.Article
- 5. Livingstone AS. Vascular injuries in the head and neck. Otolaryngol Clin North Am 1983;16:671–8.ArticlePubMed
- 6. Khoury G, Hajj H, Khoury SJ, Basil A, Speir R. Penetrating trauma to the carotid vessels. Eur J Vasc Surg 1990;4:607–10.ArticlePubMed
- 7. Ramadan F, Rutledge R, Oller D, Howell P, Baker C, Keagy B. Carotid artery trauma: a review of contemporary trauma center experience. J Vasc Surg 1995;21:46–56; discussion 55–6, ArticlePubMed
- 8. Hara Y, Yamashita H, Ohta K, Kozawa S, Nakamura M. Emergent surgical repair for penetrating injury of the cervical carotid artery associated with shock. Neurol Med Chir (Tokyo) 2009;49:300–2.ArticlePubMed
- 9. Reva VA, Pronchenko AA, Samokhvalov IM. Operative management of penetrating carotid artery injuries. Eur J Vasc Endovasc Surg 2011;42:16–20.ArticlePubMed
- 10. du Toit DF, van Schalkwyk GD, Wadee SA, Warren BL. Neurologic outcome after penetrating extracranial arterial trauma. J Vasc Surg 2003;38:257–62.ArticlePubMed
- 11. Alcocer F, David M, Goodman R, Jain SK, David S. A forgotten vascular disease with important clinical implications. Subclavian steal syndrome. Am J Case Rep 2013;14:58–62.ArticlePubMedPMC
- 12. Bacci D, Valecchi D, Sgambati E, Gulisano M, Conti AA, Molino-Lova R, et al. Compensatory collateral circles in vertebral and carotid artery occlusion. Ital J Anat Embryol 2008;113:265–71. PubMed
- 13. Matsumoto H, Hara Y, Yagi T, Saito N, Mashiko K, Iida H, et al. Impact of urgent resuscitative surgery for life-threatening torso trauma. Surg Today 2017;47:827–35.ArticlePubMedPDF
- 14. Riles TS, Imparato AM, Jacobowitz GR, Lamparello PJ, Giangola G, Adelman MA, et al. The cause of perioperative stroke after carotid endarterectomy. J Vasc Surg 1994;19:206–14; discussion 215–6, ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite