Articles
- Page Path
- HOME > J Trauma Inj > Volume 30(4); 2017 > Article
-
Original Article
Quality Improvement in the Trauma Intensive Care Unit Using a Rounding Checklist: The Implementation Results - Ye Rim Chang, M.D., M.S.1, Sung Wook Chang, M.D., M.S.2, Dong Hun Kim, M.D., M.S.1, Jeongseok Yun, M.D., Ph.D.1, Jung Ho Yun, M.D., M.S.3, Seok Won Lee, M.D.1, Han Cheol Jo, M.D., M.S.1, Seok Ho Choi, M.D., Ph.D.1
-
Journal of Trauma and Injury 2017;30(4):113-119.
DOI: https://doi.org/10.20408/jti.2017.30.4.113
Published online: December 30, 2017
- 6,995 Views
- 254 Download
1Department of Surgery, Trauma Center, Dankook University Hospital, Cheonan, Korea
2Department of Thoracic and Cardiovascular Surgery, Trauma Center, Dankook University Hospital, Cheonan, Korea
3Neurological Surgery, Trauma Center, Dankook University Hospital, Cheonan, Korea
- Correspondence to: Sung Wook Chang, M.D., M.S., Department of Thoracic and Cardiovascular Surgery, Trauma Center, Dankook University Hospital, 201 Manghyangro, Dongnam-gu, Cheonan 31116, Korea, Tel: +82-41-550-7119, Fax: +82-41-550-0039, E-mail: changsw3@naver.com
• Received: August 22, 2017 • Revised: October 9, 2017 • Accepted: October 12, 2017
Copyright © 2017 The Korean Society of Trauma
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Despite the numerous protocols and evidence-based guidelines that have been published, application of the therapeutics to eligible patients is limited in clinical settings. Therefore, a rounding checklist was developed to reduce errors of omission and the implementation results were evaluated.
-
Methods
- A checklist consisting of 12 components (feeding, analgesia, sedation, thromboembolic prophylaxis, head elevation, stress ulcer prevention, glucose control, pressure sore prevention, removal of catheter, endotracheal tube and respiration, delirium monitoring, and infection control) was recorded by assigned nurses and then scored by the staff for traumatized, critically ill patients who were admitted in the trauma intensive care unit (ICU) of Dankook University Hospital for more than 2 days. A total of 170 patients (950 sheets) between April and October 2016 were divided into 3 periods (period 1, April to June; period 2, July to August; and period 3, September to October) for the analysis. Questionnaires regarding the satisfaction of the nurses were conducted twice during this implementation period.
-
Results
- Record omission rates decreased across periods 1, 2, and 3 (19.9%, 12.7%, and 4.2%, respectively). The overall clinical application rate of the checklist increased from 90.1% in period 1 to 93.8% in period 3. Among 776 (81.7%) scored sheets, the rates of full compliance were 30.2%, 46.2%, and 45.1% for periods 1, 2, and 3, respectively. The overall mean score of the questionnaire regarding satisfaction also increased from 61.7 to 67.6 points out of 100 points from period 1 to 3.
-
Conclusions
- An ICU rounding checklist could be an effective tool for minimizing the omission of preventative measures and evidence-based therapy for traumatized, critically-ill patients without overburdening nurses. The clinical outcomes of the ICU checklist will be evaluated and reported at an early date.
- Numerous protocols and guidelines are continually being established to improve the outcomes of critically ill patients. However, they are useful only when implemented for those meeting the appropriate criteria. Compared to errors of commission, which are obvious and visible, errors of omission are associated frequently with a failure to consider routine intensive care unit (ICU) intervention practices that may be forgotten in the face of more acute issues [1,2]. According to a recent report, ‘best practice’ therapeutics were implemented in just 56 % of ICU patients who were eligible [3].
- To deter errors of omission, checklists consisting of short mnemonics to highlight some key aspects in the general care of all critically ill patients was suggested [4]. Since ‘FAST HUG’ was introduced by Vincent [4], many centers have developed and applied checklists that are suitable for each center.
- In this regard, our trauma center developed a rounding checklist to reduce errors of omission and encourage the application of the latest guidelines and protocols, and here we report the results of implementation.
INTRODUCTION
- A rounding checklist was developed to decrease the omission of 12 components in the trauma ICU: feeding, analgesia, sedation, thromboembolic prophylaxis, head elevation, stress ulcer prevention, glucose control, pressure sore prevention, removal of catheter, endotracheal tube and respiration, delirium monitoring, and infection control (Fig. 1). The traumatized, critically-ill patients who were admitted to trauma surgeons of trauma ICU of Dankook University Hospital between April and October 2016 for more than 2 days were included in this study. The patients who were declared brain dead, who did not want to be resuscitated, or whose family member refused further treatment were excluded from the cohort. The checklist was recorded by assigned nurses, then reviewed and scored by the multidisciplinary team of trauma surgeons. Omitted or erroneous medical practice was intervened and corrected using this rounding checklist.
- Basic patient characteristics, record omission rates, rates of scored rounding checklists to total rounding checklists, and scores of the checklist according to each component and period that indicates clinical application rate were obtained throughout the implementation period. Interim analysis of these parameters and quality improvement activities by multidisciplinary team meetings were performed in June and August. Therefore, the implementation results were divided into 3 periods for the analysis: April to June (period 1), July to August (period 2), and September to October (period 3). A questionnaire was performed after periods 1 and 3 in regards to satisfaction of the ICU nurses, consisting of 56 items that could be categorized into general satisfaction, comprehension of the protocol and checklist, satisfaction regarding the work burden, contents of the checklist, usefulness of the checklist in patient management, satisfaction regarding communication and application, and satisfaction regarding education. Each item was graded on a 5-point scale (1, very unsatisfied; 2, unsatisfied; 3, fair; 4, satisfied; 5, very satisfied), which was converted to 100 points and median scores of each category were calculated.
- Continuous variables were compared by paired t tests and categorical variables by chi-square tests. p values <0.05 were considered statistically significant. All statistical analyses were performed using PASW Statistics 19 (IBM Corp., Somers, NY, USA).
METHODS
- During the implementation period, a total of 950 sheets from 114 patients were obtained. The mean age was 56.5±17.5 years and males consisted of 76.3%. The median injury severity score (ISS) was 22.0±10.0 and the ISS of 89 patients (78.1%) exceeded 15. Operative management was performed in 80.7% of the patients. The median lengths of ICU stay and hospital stay was 6.0 days and 27.0 days, respectively (Table 1).
- Record omission rates decreased across periods 1, 2, and 3 (19.9%, 12.7%, and 4.2%, respectively). The most significant improvement was shown in the record omission rates of assigned nurses (from 71.1% to 4.0%). The record omission rates of sedation also greatly decreased from 55.1% to 5.9%. The record omission rate of feeding decreased to 0.9% in period 3, which was the lowest among the parameters (Fig. 2).
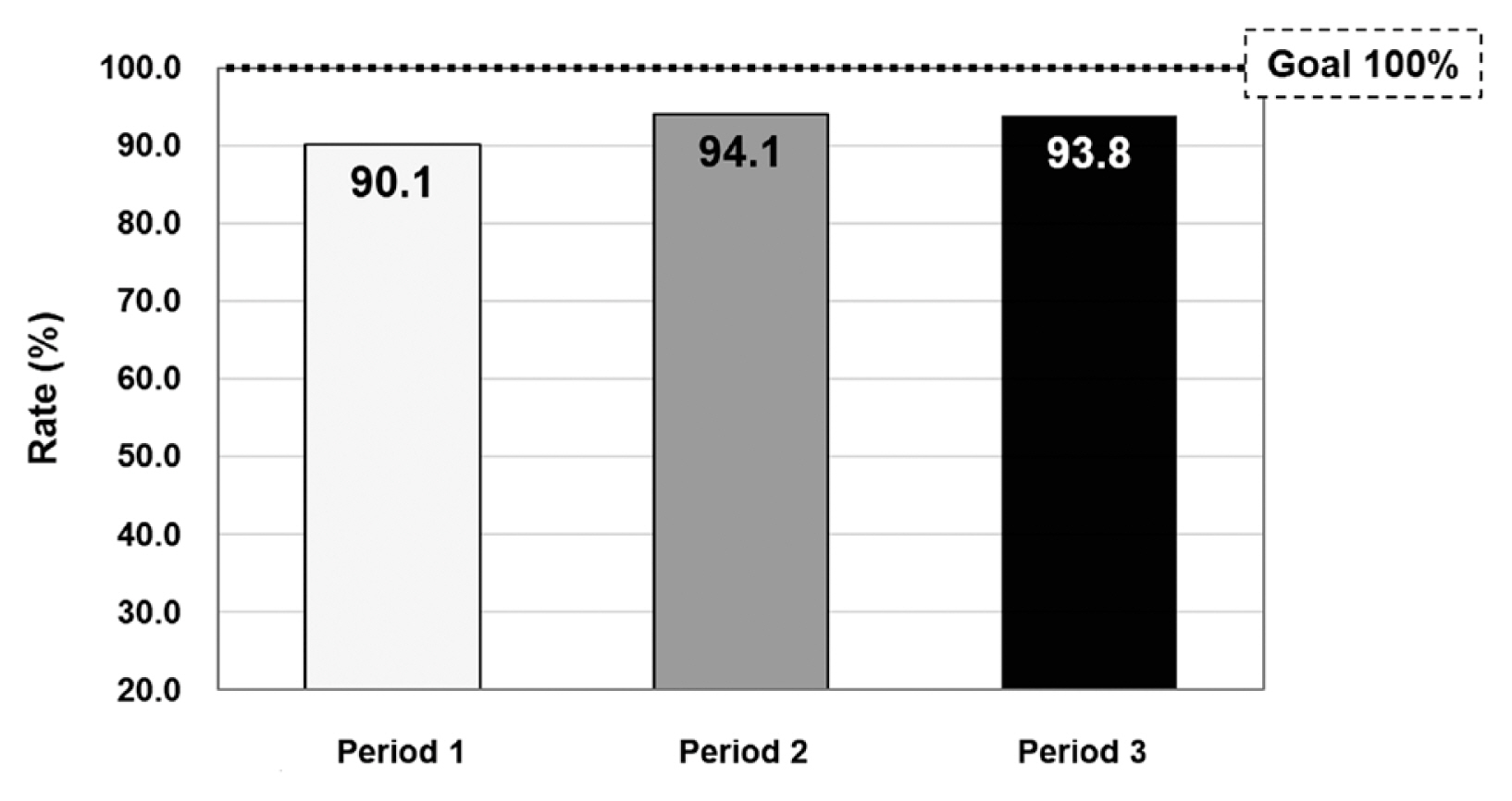
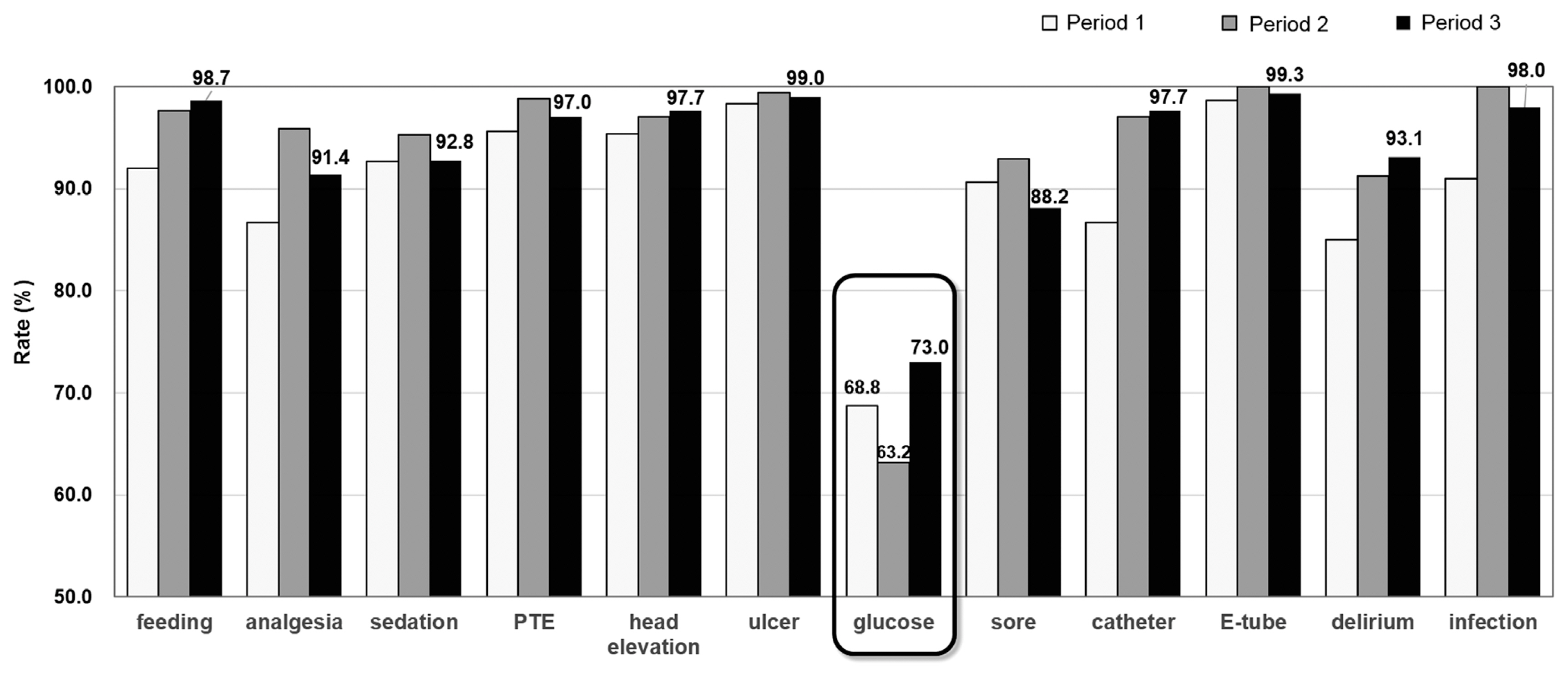
- The rates of scored rounding checklists to total rounding checklists recorded by nurses increased from 68.7% (301/438) to 93.8% (304/324) (Table 2). Overall clinical application rates of the checklist increased from 90.1% in period 1 to 93.8% in period 3 (Fig. 3). Among the 12 components, glucose control showed the lowest application rate, which only increased to 73.0% in period 3 (Fig. 4). Table 3 shows the distribution of the checklist scores. Among 776 (81.7%) scored sheets, the rates of full compliance (score 12) consisted of 30.2%, 46.2%, and 45.1% for periods 1, 2, and 3, respectively.
- Regarding the satisfaction among the ICU nurses, the overall mean score of the questionnaire increased from 61.7 to 67.6 points out of 100 points in the second survey compared to the primary survey. The mean scores of all categories increased; the mean score of category B (comprehension of the protocol and checklist) was the highest among the categories and category C (satisfaction regarding the work burden) increased the most. The general satisfaction score (category A) increased from 64.9 to 69.1 points (Fig. 5).
RESULTS
- Medical errors are common and do persist even when evidence-based therapies are available. Checklists that can implement a wide range of protocols are proposed [4] and being applied to decrease errors of omission [2,5–12].
- For the development of a rounding checklist, numerous guidelines, latest clinical study results, and checklists of other centers were thoroughly reviewed and 12 components, which are considered to be essential for critically ill patients, were adopted. Goals of therapy and standards of care for each component were set through several consensus meetings involving the center staff physicians 3 months before implementation.
- An important factor to consider during the development of a checklist was a strategy to translate detecting omissions to actual changes in the therapies given to the patients [12]. To accomplish this goal, every component was graded according to its criteria, and comments for the correction were recorded in a separate column (Fig. 1), and added or modified management plans were given to assigned nurses.
- Since excessive documentation burden associated with the checklist may contribute to a ‘checklist burnout’ and may result in impact loss or even worsening of patient outcomes according to a previous report [8], conciseness must be considered for the sustainability of the checklist. Therefore, the recording was minimized as much as possible during the development and modification of the checklist without compromising the information that must be provided. For example, some of the components were checked once a day (Fig. 1).
- After accomplishing the primitive form, the checklist was modified and updated 12 times through repeated discussions and feedback from staff physicians and nurses. Interim analyses regarding the record omission rates, application rates, and questionnaire results were performed and followed by quality improvement activities according to possible causes and measures at the end of each period. One of the activities was establishment of a continuous insulin infusion protocol. Since application rates of glucose control were poor in the interim evaluation, the protocol was developed and educated. The checklist was also modified to be concise to record and clear to communicate through these processes.
- The next step for effective implementation of this checklist included an understanding of the goals of therapy among nursing staff as well as staff physicians. Four educational sessions were conducted during the initial period in regards to patient assessment (e.g., Confusion Assessment Method for the ICU flowsheet [13], Richmond Agitation-Sedation scale [14]), current guidelines and protocols for each component, and goals of therapy for traumatized, critically ill patients. Two additional supplementary educations for modified contents were also given to the ICU nurses periodically.
- To ensure the checklist was not overburdening the ICU nurses and was being successfully implemented, questionnaires regarding satisfaction, comprehension of the protocol and checklist, and usefulness of the checklist in patient management were conducted. Increases in the mean scores of overall and individual categories in the second survey indicated that the checklist did not significantly alter nursing workloads. An understanding of the goals of therapy, which brought active participation in patient management, was achieved among the ICU nurses through the use of the checklist and education.
- Through these efforts, record rates and overall application rates increased during the implementation period. The rates of full compliance (i.e., the rates of full marks), as well as each score of the checklist components, improved. The checklist, therefore, contributed in reducing omissions of preventative measures and evidence-based therapy without altering nursing workloads. Competency, communication among the physicians and ICU nurses, and satisfaction of the nurses improved as well as the application rates.
DISCUSSION
- In conclusion, an ICU rounding checklist could be an effective tool to reduce errors of omission and encourage application of the latest guidelines and protocols for traumatized, critically ill patients without overburdening nurses. This study is confined to the results of implementation, while the actual improvement in the outcomes of the ICU patients, which is an ultimate purpose of this checklist, was not analyzed in the study. Clinical outcomes of the patients after implementation of the checklist will be evaluated and reported at an early date.
CONCLUSION
Fig. 1Rounding checklist. The checklist consisting of 12 components was recorded by assigned intensive care unit (ICU) nurses. Six components (marked with an asterisk) were recorded 3 times per day. Recorded checklists were then reviewed and scored by the trauma surgeons. Omitted or erroneous medical practice was intervened and corrected using this rounding checklist. p-TPN: peripheral total parenteral nutrition, c-TPN: central total parenteral nutrition, NRS: numerical rating scale, CPOT: critical-care pain observation tool, RASS: richmond agitation-sedation scale, SAT: spontaneous awakening trial, IPC: intermittent pneumatic compression, BST: blood sugar level, med: medication, RI: regular insulin, c-line: central line, PICC: peripherally inserted central catheter, e-tube: endotracheal tube, t-tube: tracheostomy tube, SBT: spontaneous breathing trial, CAM-ICU: confusion assessment method for the ICU flowsheet, TICU: trauma intensive care unit, CNS: central nervous system, N/A: not applicable.
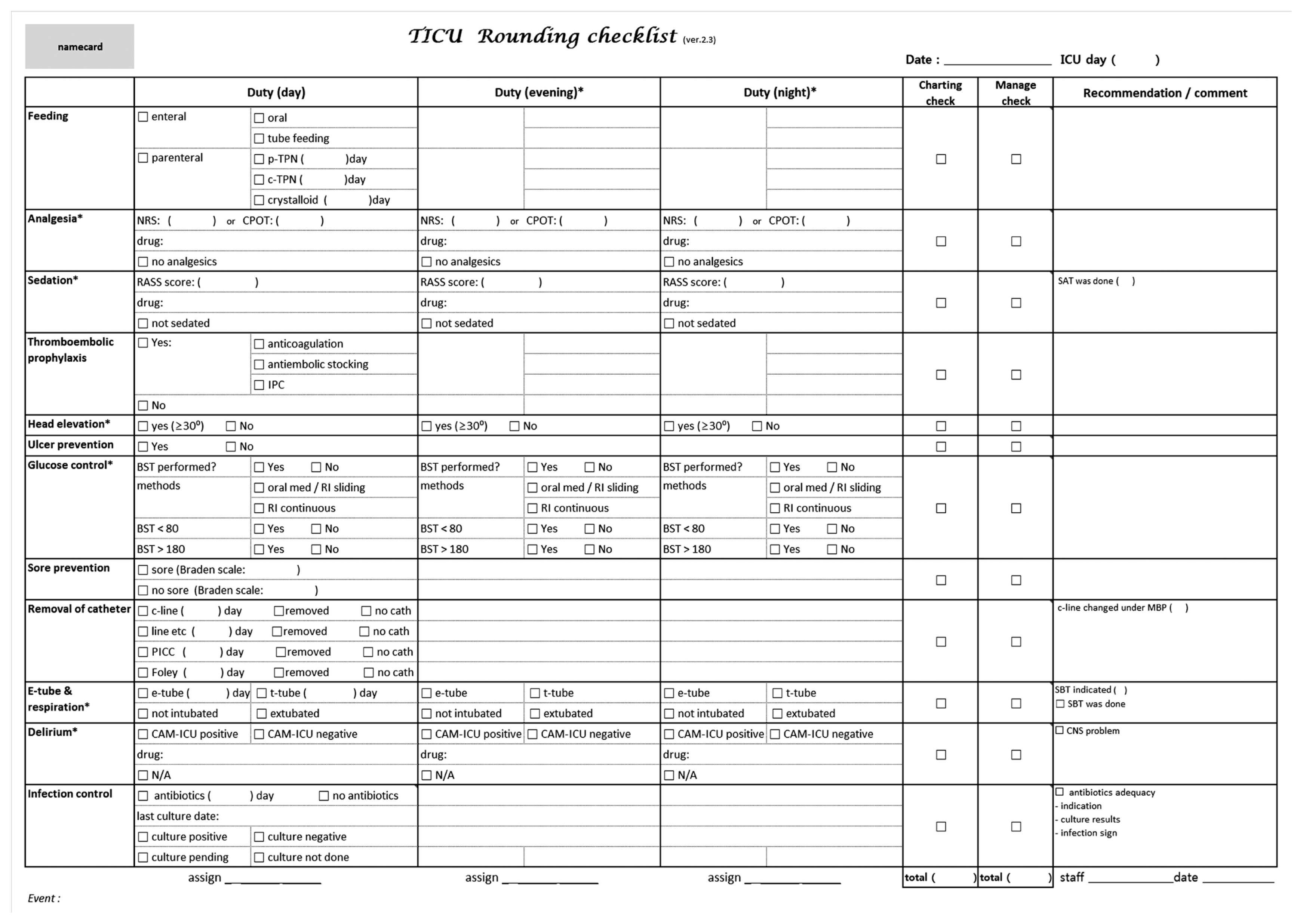
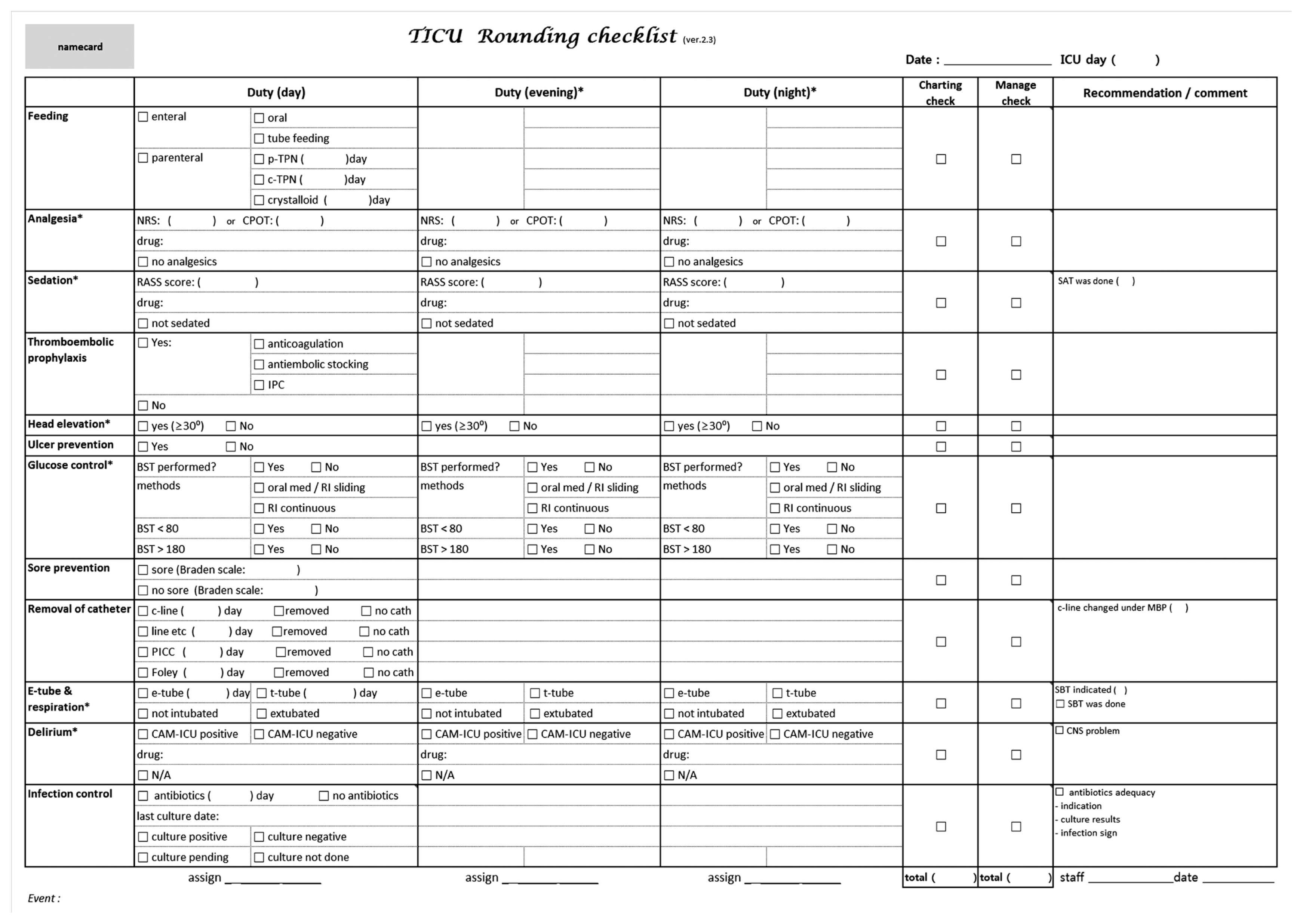
Fig. 2Record omission rates. Record omission rates decreased across periods. PTE: pulmonary thromboembolism, E-tube: endotracheal tube.
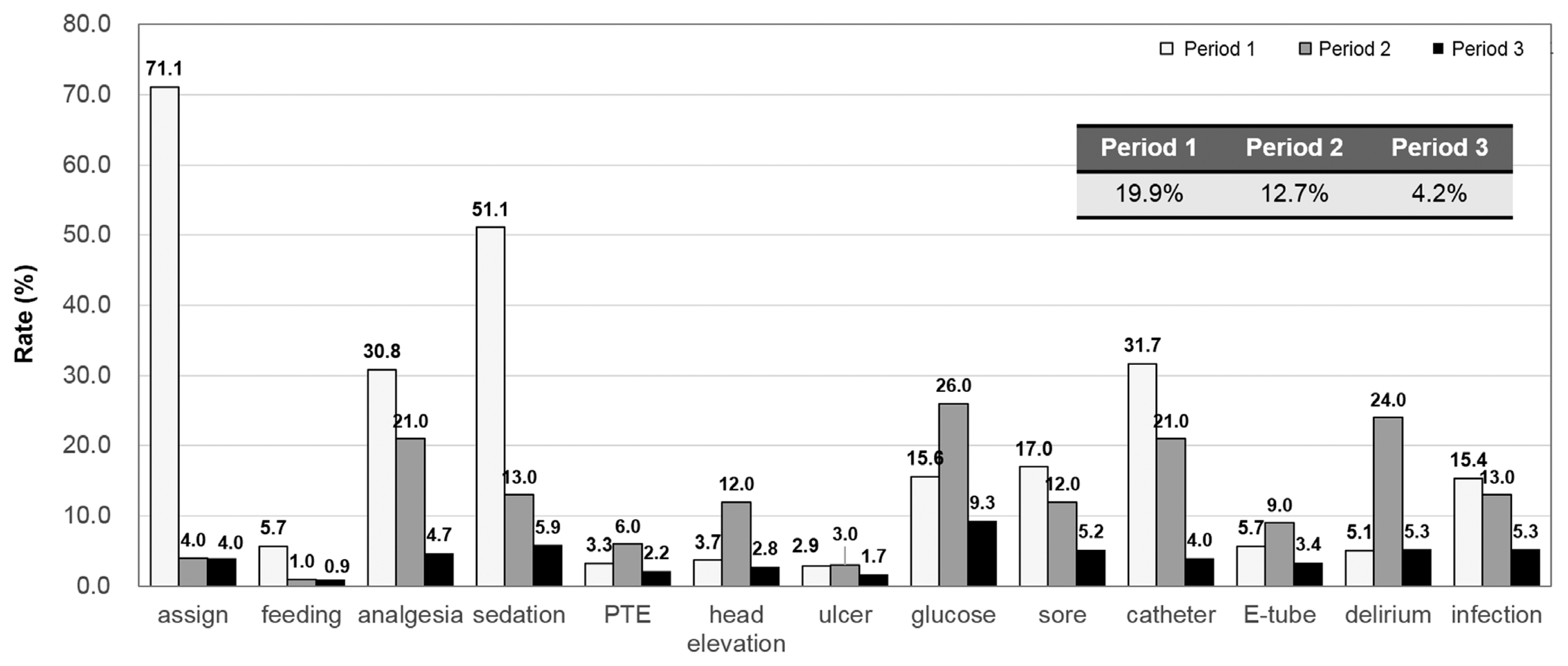
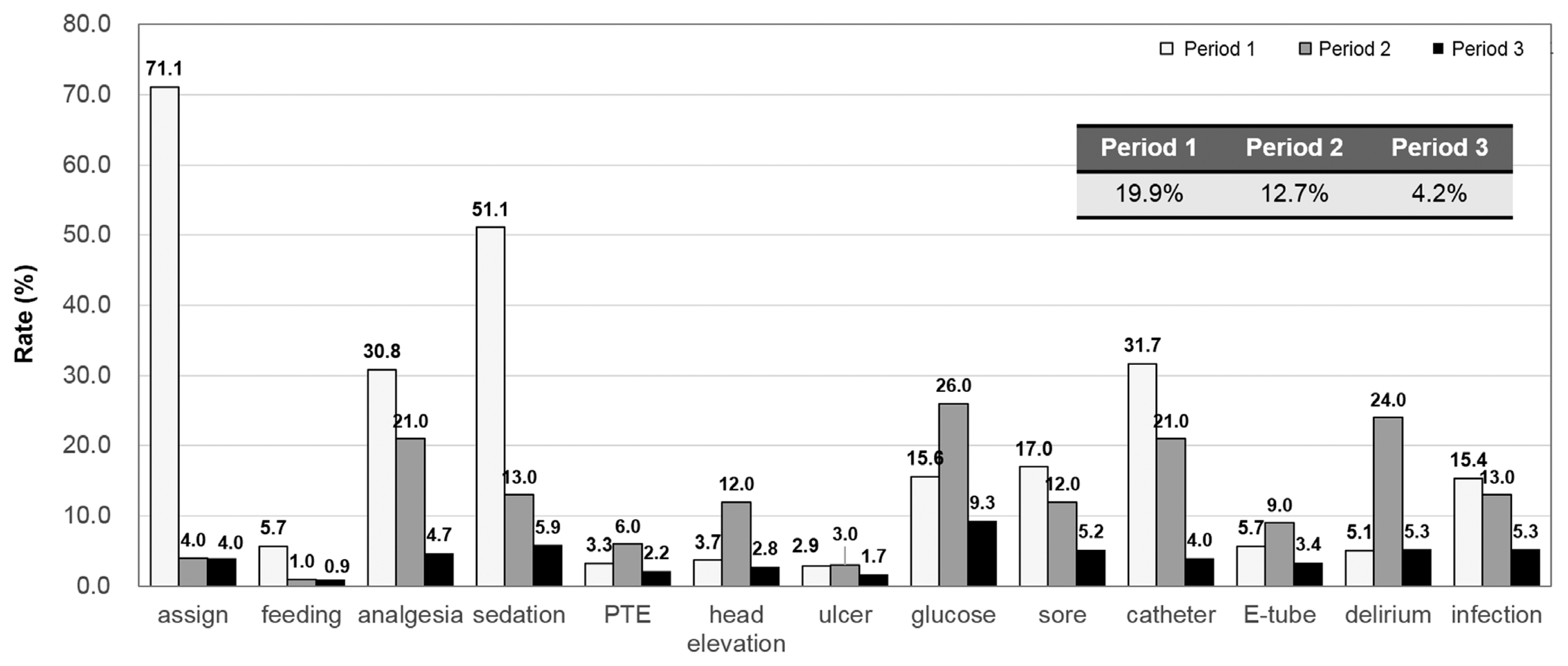
Fig. 3Clinical application rates. Overall clinical application rates of the checklist increased from 90.1% in period 1 to 93.8% in period 3.
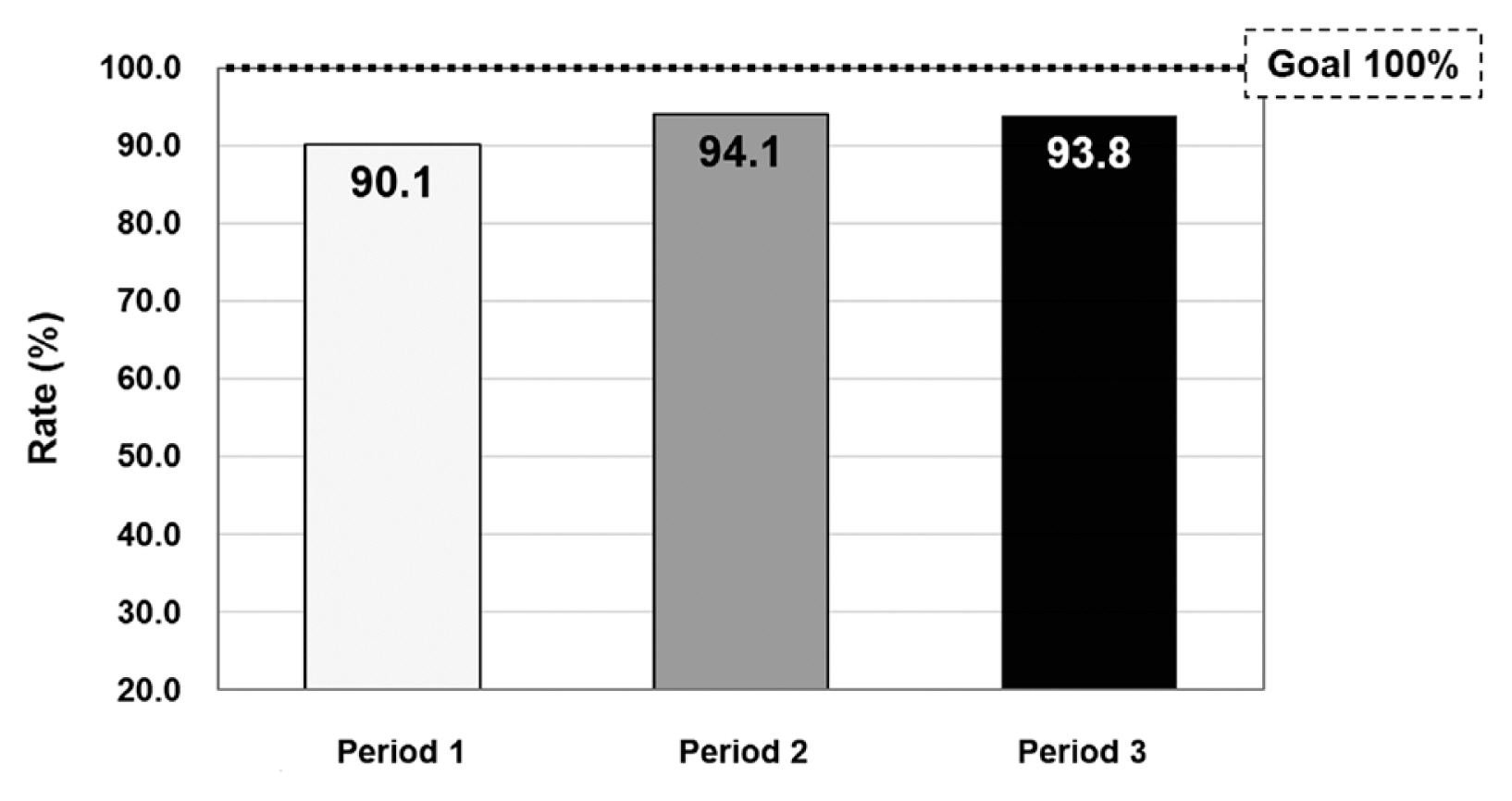
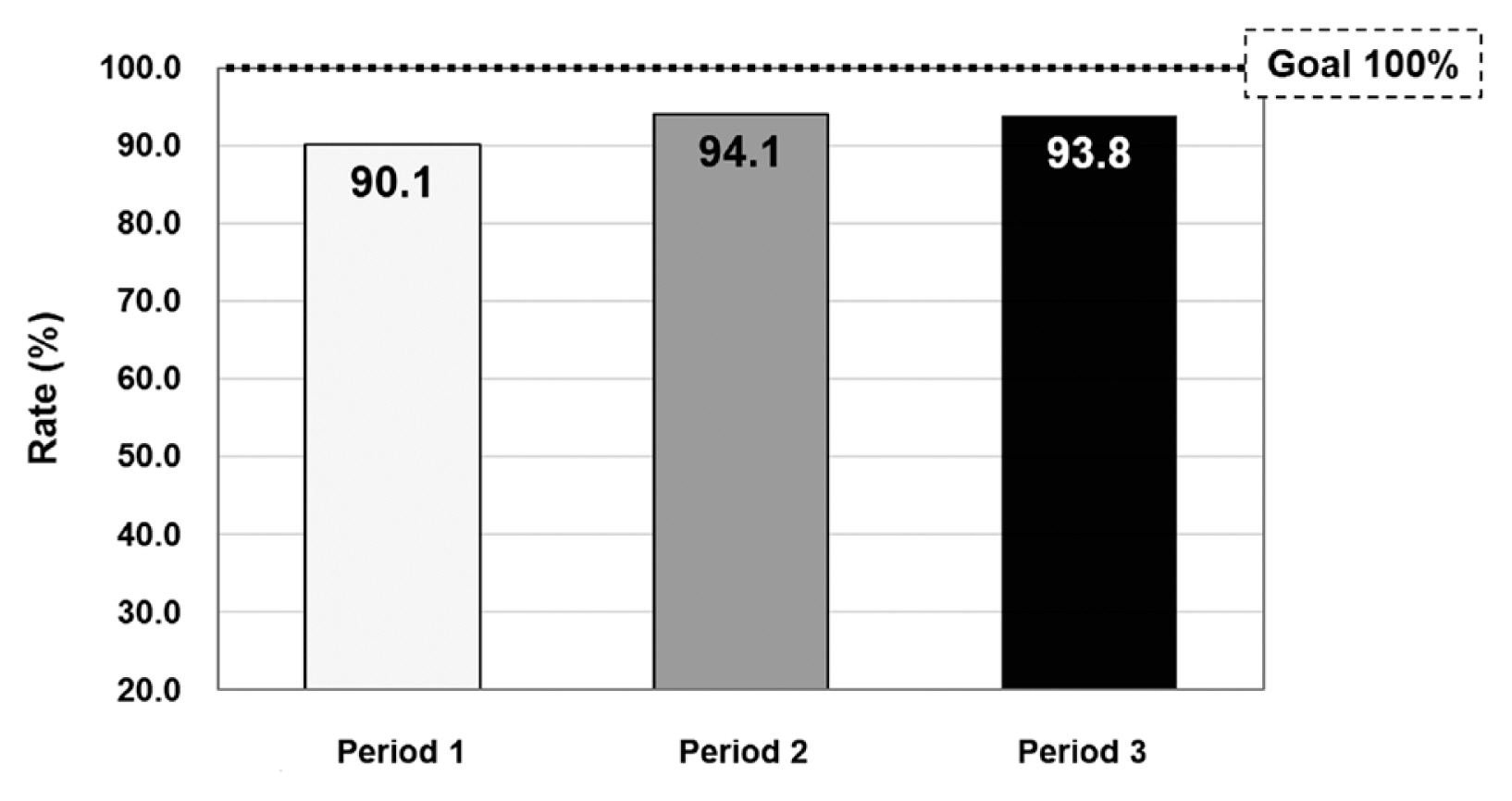
Fig. 4Clinical application rates according to each component. Clinical application rates for all components increased in period 3 compared to period 1. Glucose control showed the lowest application rate among the components. A continuous insulin infusion protocol was developed and applied based on these results. PTE: pulmonary thromboembolism, E-tube: endotracheal tube.
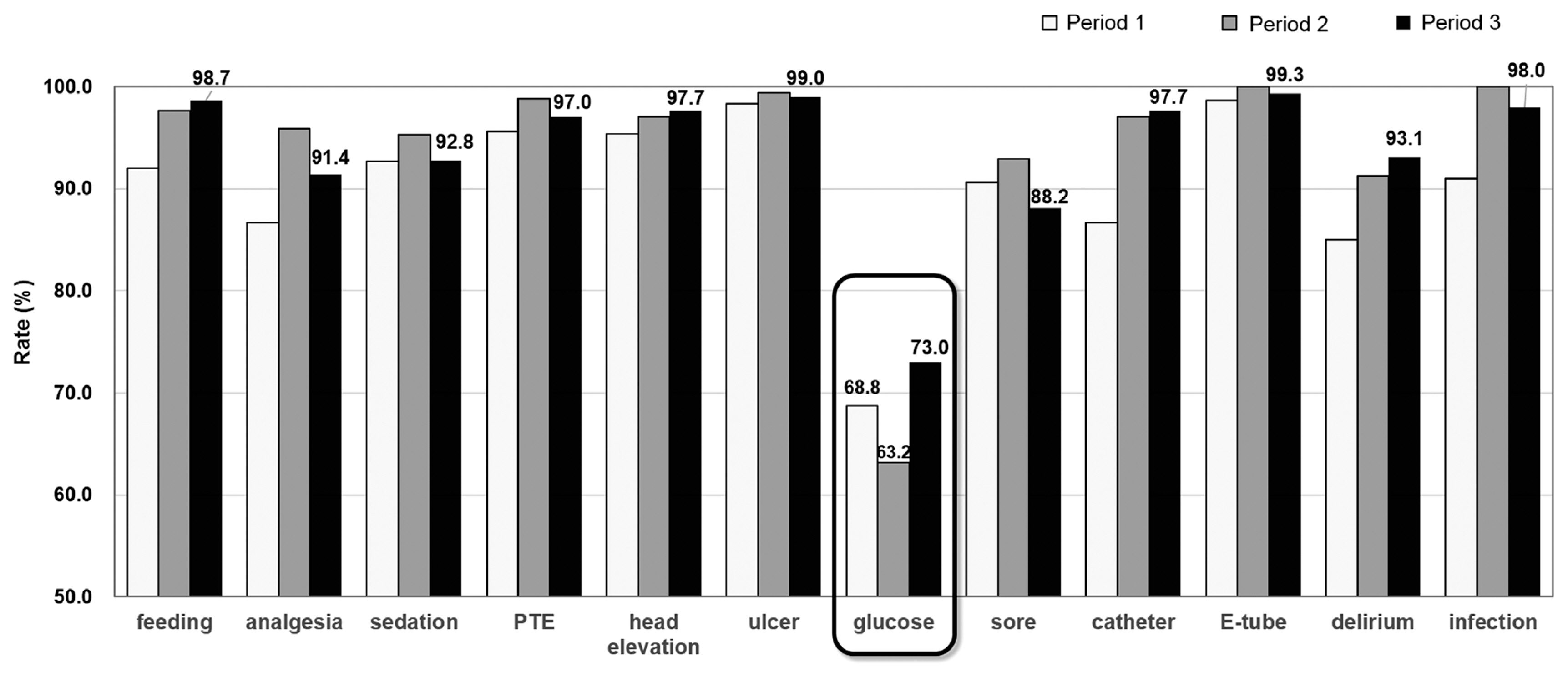
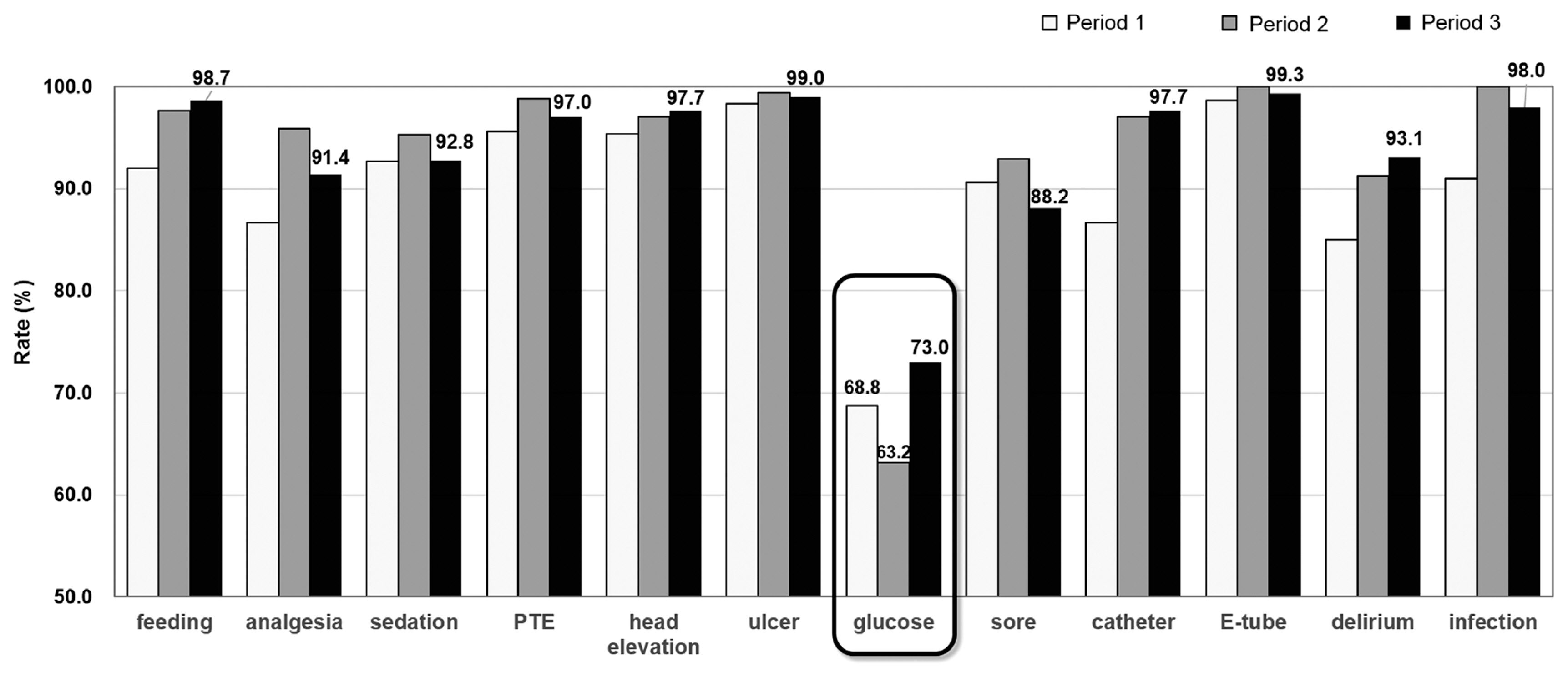
Fig. 5The scores of the questionnaire regarding satisfaction of the nurses. (A) General satisfaction. (B) Comprehension of the protocol and checklist. (C) Satisfaction regarding the work burden. (D) Contents of the checklist. (E) Usefulness of the checklist in patient management. (F) Satisfaction regarding communication and application. (G) Satisfaction regarding education.
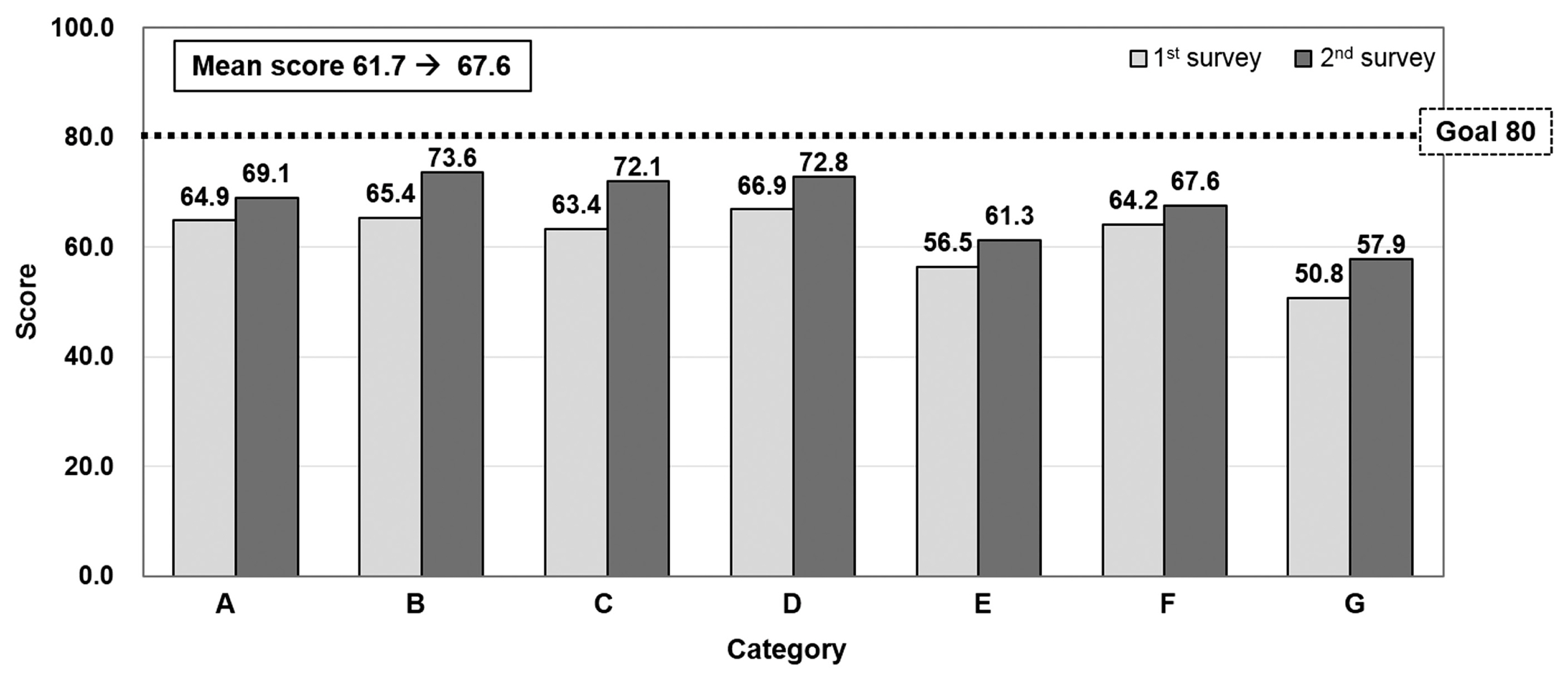
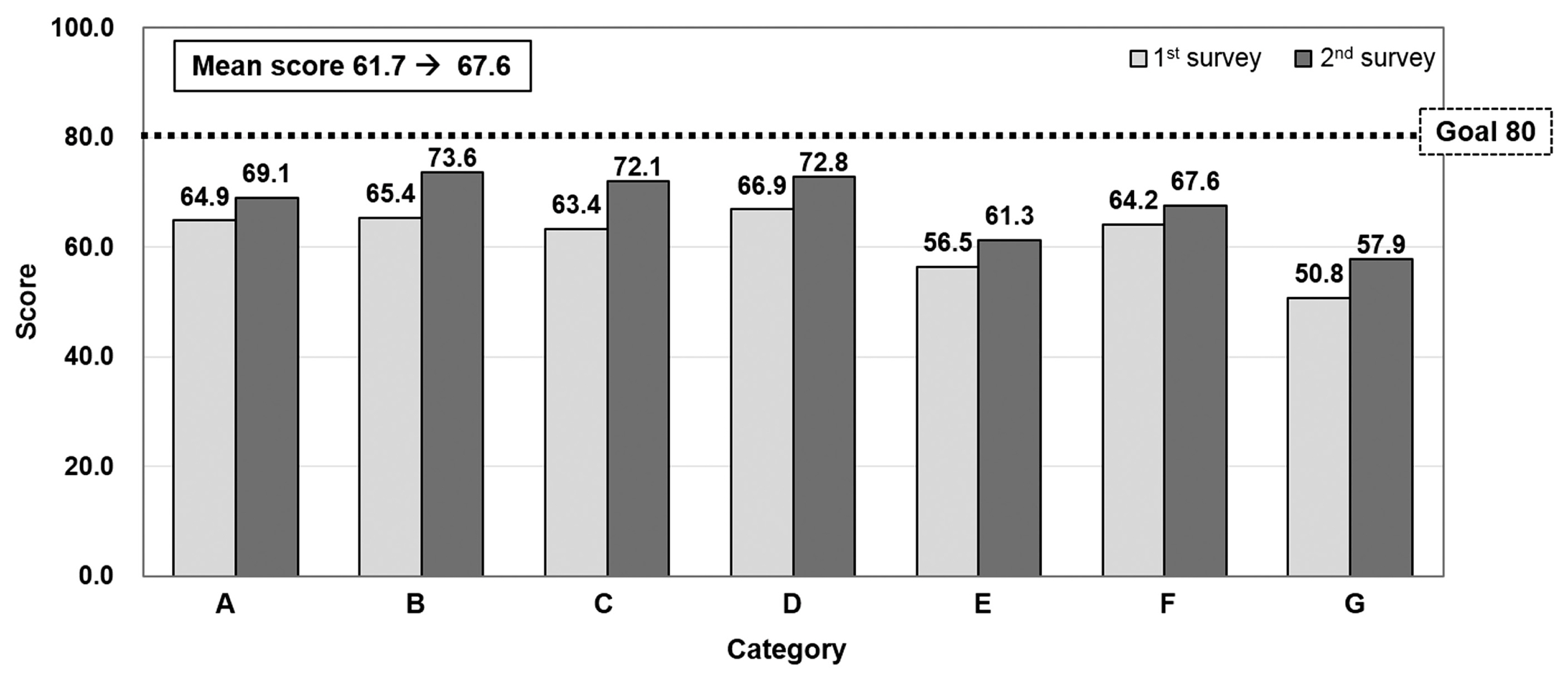
Table 1Patient characteristics
Table 2The rate of scored rounding checklists to total recorded rounding checklists
| Total number of sheet | Number of scored sheet | Rate (%) | |
|---|---|---|---|
| Period 1 | 438 | 301 | 68.7 |
| Period 2 | 188 | 171 | 91.0 |
| Period 3 | 324 | 304 | 93.8 |
| Total | 950 | 776 | 81.7 |
Table 3The distribution of the checklist scores
- 1. Weingart SN, Wilson RM, Gibberd RW, Harrison B. Epidemiology of medical error. BMJ 2000;320:774–7.ArticlePubMedPMC
- 2. Byrnes MC, Schuerer DJ, Schallom ME, Sona CS, Mazuski JE, Taylor BE, et al. Implementation of a mandatory checklist of protocols and objectives improves compliance with a wide range of evidence-based intensive care unit practices. Crit Care Med 2009;37:2775–81.ArticlePubMed
- 3. Ilan R, Fowler RA, Geerts R, Pinto R, Sibbald WJ, Martin CM. Knowledge translation in critical care: factors associated with prescription of commonly recommended best practices for critically ill patients. Crit Care Med 2007;35:1696–702.ArticlePubMed
- 4. Vincent JL. Give your patient a fast hug (at least) once a day. Critical Care Med 2005;33:1225–9.Article
- 5. Vincent WR 3rd, Hatton KW. Critically ill patients need “FAST HUGS BID” (an updated mnemonic). Crit Care Med 2009;37:2326–7; author reply 2327, Article
- 6. DuBose JJ, Inaba K, Shiflett A, Trankiem C, Teixeira PG, Salim A, et al. Measurable outcomes of quality improvement in the trauma intensive care unit: the impact of a daily quality rounding checklist. J Trauma 2008;64:22–7; discussion 27–9, ArticlePubMed
- 7. Dubose J, Teixeira PG, Inaba K, Lam L, Talving P, Putty B, et al. Measurable outcomes of quality improvement using a daily quality rounds checklist: one-year analysis in a trauma intensive care unit with sustained ventilator-associated pneumonia reduction. J Trauma 2010;69:855–60.ArticlePubMed
- 8. Teixeira PG, Inaba K, Dubose J, Melo N, Bass M, Belzberg H, et al. Measurable outcomes of quality improvement using a daily quality rounds checklist: two-year prospective analysis of sustainability in a surgical intensive care unit. J Trauma Acute Care Surg 2013;75:717–21.ArticlePubMed
- 9. Simpson SQ, Peterson DA, O’Brien-Ladner AR. Development and implementation of an ICU quality improvement checklist. AACN Adv Crit Care 2007;18:183–9.ArticlePubMedPDF
- 10. Papadimos TJ, Hensley SJ, Duggan JM, Khuder SA, Borst MJ, Fath JJ, et al. Implementation of the “FASTHUG” concept decreases the incidence of ventilator-associated pneumonia in a surgical intensive care unit. Patient Saf Surg 2008;2:3, ArticlePubMedPMC
- 11. Hewson KM, Burrell AR. A pilot study to test the use of a checklist in a tertiary intensive care unit as a method of ensuring quality processes of care. Anaesth Intensive Care 2006;34:322–8.ArticlePubMed
- 12. Idahosa O, Kahn JM. Beyond checklists: using clinician prompts to achieve meaningful ICU quality improvement. Crit Care 2012;16:305, ArticlePubMedPMC
- 13. Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001;29:1370–9.ArticlePubMed
- 14. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The Richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002;166:1338–4.ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite