Submental intubation using laparoscopic trocar in zygomaticomaxillary complex fracture surgery in Korea: a case report
Article information
Abstract
Submental intubation is an effective alternative technique for airway management in patients with maxillofacial trauma. Compared with tracheostomy, it is less invasive, but has risks associated with potential airway compromise such as hypoxia due to tube obstruction, collapse, and kinking. To shorten procedure time and ensure a reinforced tube lumen, we used a laparoscopic trocar as a new device for submental intubation. A 54-year-old male patient sustained a zygomaticomaxillary complex fracture and was scheduled to undergo open reduction and internal fixation. We performed intraoral intubation and made a small 1-cm incision at the submandibular midline. After dissection of the tissue from the incision site, a reinforced tube was passed using a 12-mm laparoscopic trocar. The procedure took about 5 minutes, and apnea time from disconnecting the breathing circuit and passing through the internal lumen of the trocar until it was reconnected to the ventilator was 1 minute 5 seconds. Using a laparoscopic trocar for submental intubation can reduce the time required for dissection, prevent luminal occlusion complications due to soft tissues or blood clots in the endotracheal tube, and decrease soft tissue damage.
INTRODUCTION
Submental intubation is a technique wherein the endotracheal tube protrudes through the anterior floor of the mouth, not through the mouth opening, which allows free intraoperative access to the oral cavity and nasal pyramid without compromising the airway in patients with skull base trauma. The reason for performing submental intubation is that facial trauma patients may also have a fracture at the base of the skull, and it is important to determine dental malocclusion during oral surgery. In addition, nasotracheal intubation is not possible in patients with basilar fracture, and in zygomaxillary complex fracture surgery, the surgeon and anesthesiologist share the intraoral space, making it difficult to manage the airway through the mouth during surgery [1]. Therefore, after securing an airway by orotracheal intubation, airway management is performed through submandibular intubation or tracheostomy. Submental intubation can be used for short-term airway control as an alternative to tracheostomy but with minimal complications [2].
Although it has been modified in various ways since it was first proposed by Altemir [3] in 1986, no published modification or specific type of reinforced tubing has been universally demonstrated to be superior. Since then, other complementary techniques using the tracheostomy kit have been proposed, but even this method could not prevent blockage of the internal lumen of the endotracheal tube by blood clot and soft tissue and caused trauma to surrounding soft tissue [4–6]. Various efforts have been introduced to reduce or address complications that occur in the process of exteriorization [7–9].
The proposed method using a laparoscopic trocar is part of that effort. This is a method that can be easily and simply mounted without blood clots and soft tissues entering the endotracheal tube, while also reducing the soft tissue trauma that occurs during the exteriorization process.
CASE REPORT
A 54-year-old male patient sustained a zygomaticomaxillary complex fracture after a 5-m fall. The patient was scheduled to undergo open reduction and internal fixation and intermaxillary fixation including a closed reduction for nasal bone fracture.
Instead of nasal intubation or tracheostomy, we decided to perform submental intubation using a 12-mm laparoscopic trocar. Before the procedure, we checked that the reinforced endotracheal tube (internal diameter, 7.0 mm) passed through the trocar’s internal lumen. The connector part of the reinforced tube was removed.
Then, the tube change was performed using a videoscope with a reinforced tube prepared from the conventional tube the patient had received. Subsequently, the oral and maxillofacial surgeon placed an incision of about 1 cm in the submental space and dissected it with Kelley forceps to reach the mouth floor (Figs. 1, 2). Upon dilation of the open penetrating site from the skin to the mouth floor, a laparoscopic trocar was inserted from the skin to the mouth floor. After confirming that the tip of the trocar has passed through to the mouth floor, the trocar stylet was removed, and the Kelly forceps was inserted through the trocar.
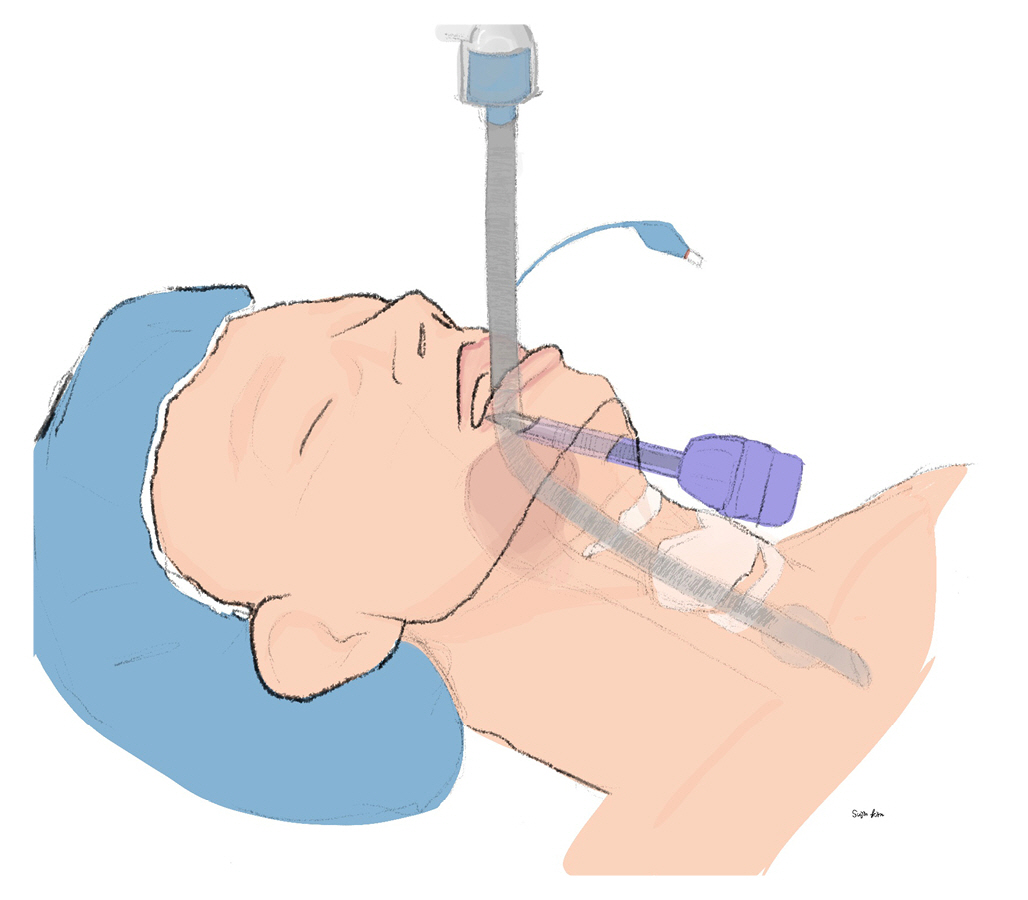
The conventional tube is changed by reinforced tube and a skin incision and soft tissue dissection were performed. A laparoscopic trocar was inserted from the skin to the mouth floor. Illustration by Sujin Kim.

After checking the mandible and midline, a surgeon makes a skin incision. The patient provided written informed consent for publication of the research details and clinical images.
First, the pilot balloon was passed into the trocar lumen and then the end of the reinforced tube with the connector removed was inserted into the trocar lumen (Figs. 3, 4). The reinforced tube was withdrawn toward the skin incision, and a connector and a breathing circuit were connected for ventilation. The airway pressure of the ventilator was checked for signs of blockage due to blood clots or soft tissue in the tube lumen. The tube depth was confirmed through capnography and auscultation, and after checking the patient's ventilation, the tube was fixed with a skin suture (Fig. 5). The patient’s apnea time from disconnecting the breathing circuit and passing through the internal lumen of the trocar until it was reconnected to the ventilator was 1 minute 5 seconds. After surgery, the reinforced tube is pulled back into the oral cavity and the incision is sutured (Fig. 6).
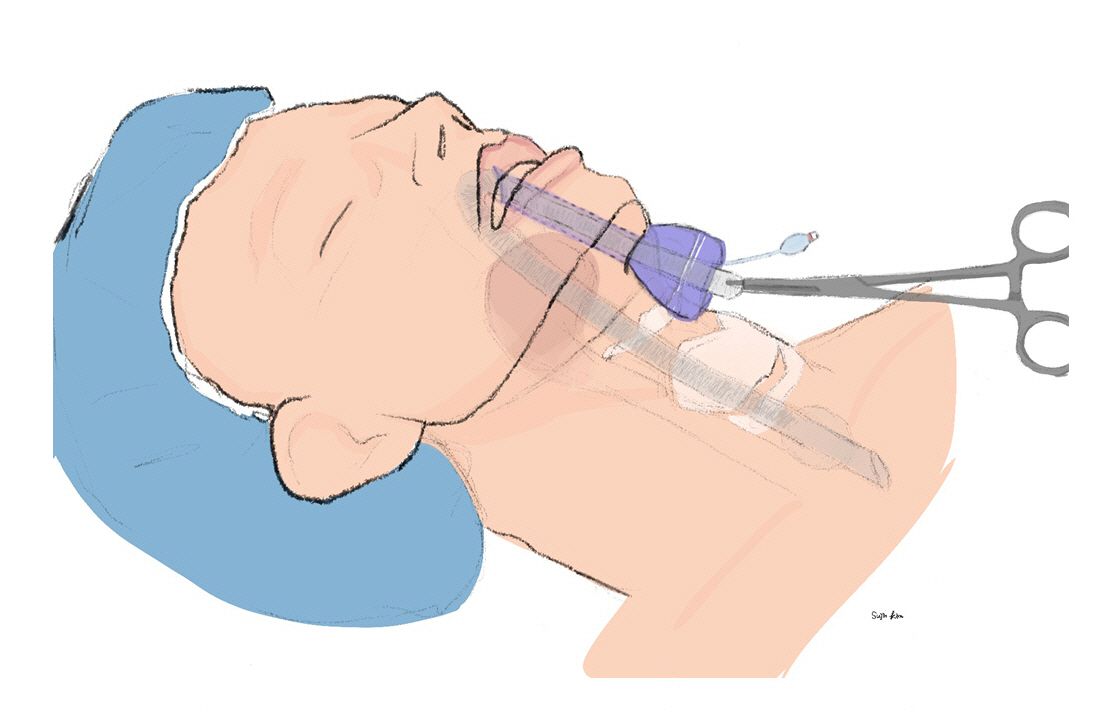
After the trocar stylet was removed, and the Kelly forceps was inserted through the trocar. The pilot balloon was passed into the trocar lumen, and then the end of the reinforced tube with the connector removed was inserted into the trocar lumen. Illustration by Sujin Kim.

A 12-mm trocar is placed from the skin to the mouth floor, and the end of the reinforced endotracheal tube is inserted into the trocar lumen in the mouth. The patient provided written informed consent for publication of the research details and clinical images.

A surgeon stabilizes the reinforced endotracheal tube with skin suture. The patient provided written informed consent for publication of the research details and clinical images.

After surgery, the reinforced tube is disconnected, and the end of the tube is pulled into the oral cavity. The reinforced tube is reconnected with the ventilator, and the submental incision is sutured. The patient provided written informed consent for publication of the research details and clinical images.
Ethics statements
This case was conducted with the approval of the Institutional Review Board of Wonju Severance Christian Hospital (No. CR322318). The patient provided written informed consent for publication of the research details and clinical images.
DISCUSSION
Submental intubation has been an effective alternative technique for airway management in patients with maxillofacial trauma since first published in 1986 [3]. Compared with tracheostomy, this method facilitates airway management in patients with skull base fracture during zygomaticomaxillary complex fracture surgery. Tracheostomy also facilitates airway management but is more invasive and has complications such as surgical emphysema, tracheal erosion, hemorrhage, dysphagia, decannulation, and scarring [2,10].
The complication associated with submental intubation is potential airway compromise. Obstruction, collapse, kinking, or displacement of endotracheal tube could lead to fatal hypoxia. Other complications include potential risk of skin infection, abscess in the mouth floor, and injury of the marginal mandibular and lingual nerves and of salivary glands [1,11]. A reinforced tube is used to prevent kinking and collapse of the endotracheal tube. Displacement of the endotracheal tube is prevented by stabilizing through skin sutures as the last step. Obstruction by blood clot or soft tissue interferes with the procedure and increases the risk of hypoxia due to apnea when an endotracheal tube is disconnected from the breathing circuit and passes through the mouth floor.
In previous studies using conventional methods, the mean time to complete the procedure was about 10 minutes [12], on the other hand, our procedure required only 5 minutes. In particular, the apnea time was about 1 minute 5 seconds, because it was the first trial using a trocar, but it is thought that this time can be shortened to about 30 to 40 seconds if physicians become skilled. A laparoscopic trocar through small incision (<2 cm) easily and quickly passes through the mouth floor and minimizes blunt trauma to surrounding tissues. Also, the probability of occlusion is low because the stylet retains its inner diameter while passing through the mouth floor. Compared with the conventional method, using a laparoscopic trocar can reduce the time required for dissection, as well as prevent luminal occlusion complications due to soft tissues or blood clots in the endotracheal tube; less surrounding tissue damage is also a benefit.
Recently, a case of submental intubation using a laparoscopic trocar like this case has been reported [13]. It is similar in methods and tools, However, in the previous case, only skin incision was performed before the passage of the laparoscopic trocar, and dissection occurred by the laparoscopic trocar stylet that passed through the bottom of the mouth. On the other hand, in our case, a laparoscopic trocar probe passes through the gap after a slight dissection of the soft tissue with forceps after skin incision. This can further reduce the soft tissue damage caused by the stylet in the previous case.
One point requiring emphasis during this procedure is sufficient space for passage between the reinforced tube and the trocar. We used a reinforced tube with an inner diameter of 7.0 mm and a 12-mm trocar, which is common use in laparoscopic surgery. Since these tools are generally used in the operating room, a trocar during submandibular intubation in patients undergoing zygomaticomaxillary complex fracture surgery is easy, safe, quick, and may cause minimal complications.
In conclusion, submental intubation is an alternative technique for airway management in maxillofacial trauma. Using a laparoscopic trocar can reduce the time required for dissection, as well as prevent luminal occlusion complications due to soft tissues or blood clots in the endotracheal tube; less soft tissue damage is another benefit. Since no definitive approach of submental intubation has been established, a large-scale study comparing existing methods including the trocar is required.
Notes
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Data sharing statement
Not applicable.
Author contributions
Conceptualization: HD, CL, HKL; Data curation: HD, HDH, HH, SK; Supervision: HKL, SK; Writing–original draft: HD, HDH, HH; Writing–review & editing: CL, HKL, SK. All authors read and approved the final manuscript.
