Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(4); 2022 > Article
-
Case Report
Experience and successful treatment of craniocerebral gunshot injury at a regional trauma center in Korea: a case report and literature review -
Mahnjeong Ha, MD
 , Seunghan Yu, MD
, Seunghan Yu, MD , Jung Hwan Lee, MD
, Jung Hwan Lee, MD , Byung Chul Kim, MD
, Byung Chul Kim, MD , Hyuk Jin Choi, MD
, Hyuk Jin Choi, MD
-
Journal of Trauma and Injury 2022;35(4):277-281.
DOI: https://doi.org/10.20408/jti.2022.0057
Published online: November 22, 2022
- 1,792 Views
- 55 Download
Department of Neurosurgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea
- Correspondence to Hyuk Jin Choi, MD Department of Neurosurgery, Pusan National University Hospital, 179 Gudeok-ro, Seo-gu, Busan 49241, Korea Tel: +82-051-240-7257 E-mail: csfdiver@naver.com
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Craniocerebral gunshot injuries is gradually increasing in the civilian population with a worse prognosis than closed head trauma. We experienced a case of craniocerebral gunshot injury which a bullet penetrating from the submandibular area into the clivus of a patient. The patient did not show any symptom. However, serial laboratory findings showed an increase in blood lead level. We removed foreign bodies without any problems using an endoscopic transnasal transclival approach. Due to the extremely low frequency, guidelines for definitive management of gunshot injuries have not been presented in Korea yet. We introduce our surgical experience of a craniocerebral gunshot injury with an unusual approach for removing intracranial foreign bodies.
- Gunshot injuries have occurred frequently in the military, but not in the civilian population, in the past. However, they are gradually increasing in the civilian population as a recent global trend [1,2]. Craniocerebral gunshot injuries (CGI) have a worse prognosis than a closed head trauma [1,3]. Even with advances in medical and surgical techniques, CGI is known to have an extremely low survival rate [4,5]. Reported survival rate of CGI is only 7% to 15% [6]. However, gunshot injuries are extremely rare in Korea where individual firearm ownership is restricted. Thus, it is seldom experienced by clinicians in Korea. Due to this special situation in Korea, there is no standard for treating gunshot injuries. Although the incidence rate of gunshot injuries is low in Korea, regional trauma centers should prepare for CGI. We report on an extremely rare CGI case with bullets in the clivus removed under a microscope view using an endoscopic transnasal transclival approach.
INTRODUCTION
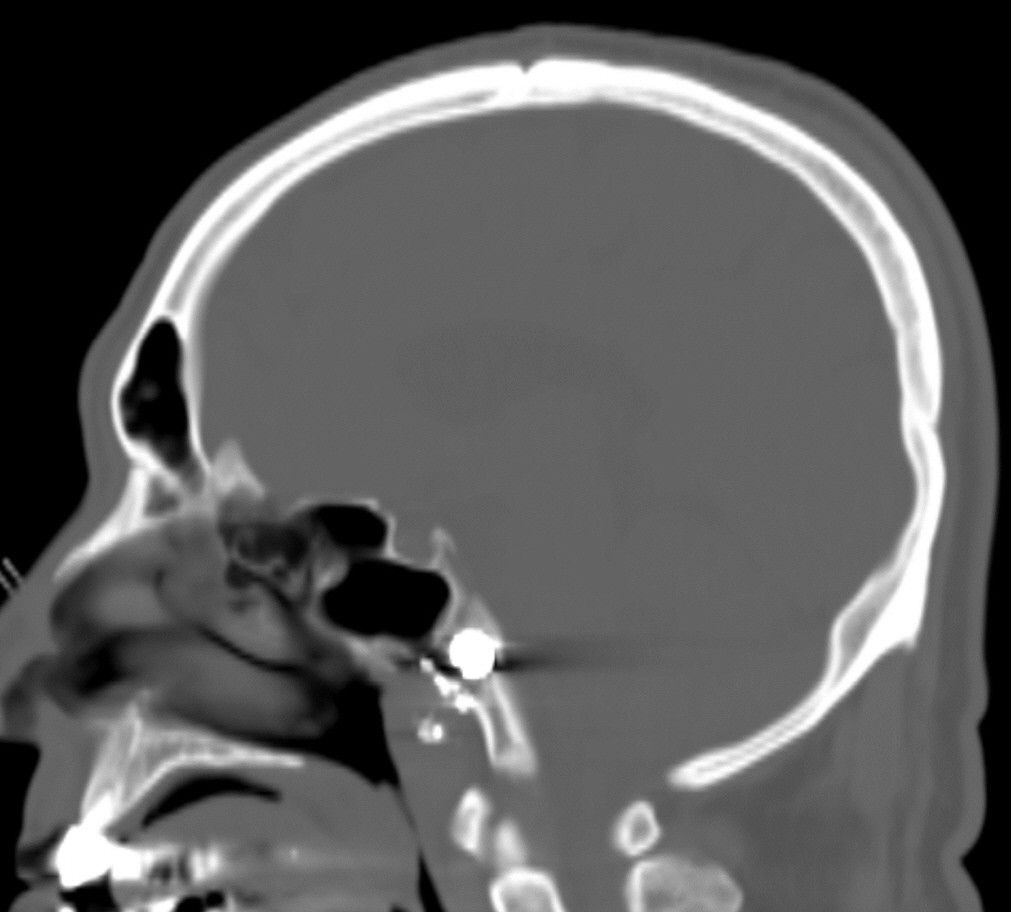
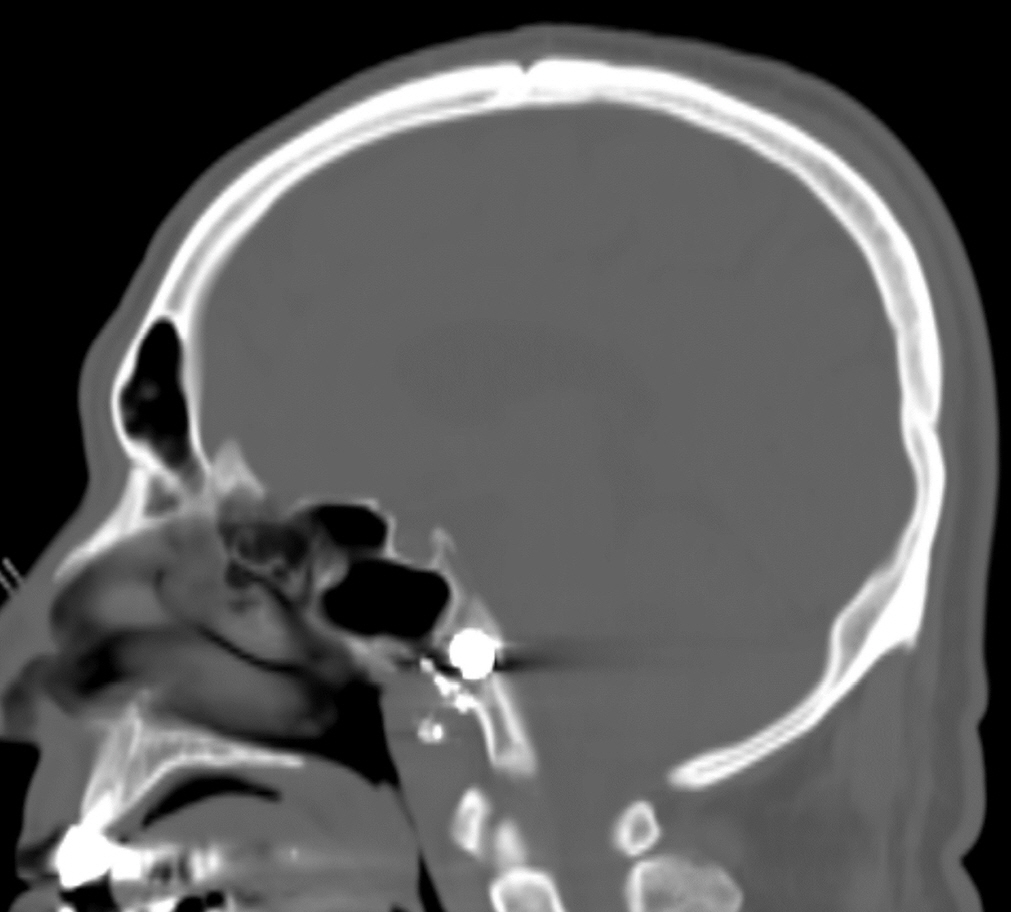
- A 59-year-old male patient with CGI was transferred to our hospital. The patient said that he aimed a shotgun under his chin and fired it with the intention of committing a suicide at around 5:30 AM. After being transferred to a nearby hospital, he was transferred to our regional trauma center. Regarding the initial patient status, the patient's level of consciousness was clear. There were no specific neurological symptoms. Otorhinolaryngological evaluation was performed immediately. There were no problems with airway or vocal cord functions. A number of foreign bodies were identified in the nasopharyngeal space and the clivus on the computed tomography (CT) scan (Fig. 1). The foreign material was a lead bullet. The patient showed no specific symptoms. After he was hospitalized, conservative treatment was performed. Considering cerebrospinal fluid leakage and central nervous system infection, tetanus vaccination and empirical antibiotics were administered. Intravenous injections of vancomycin 1 g and ceftazidime 1 g were administered three times per day.
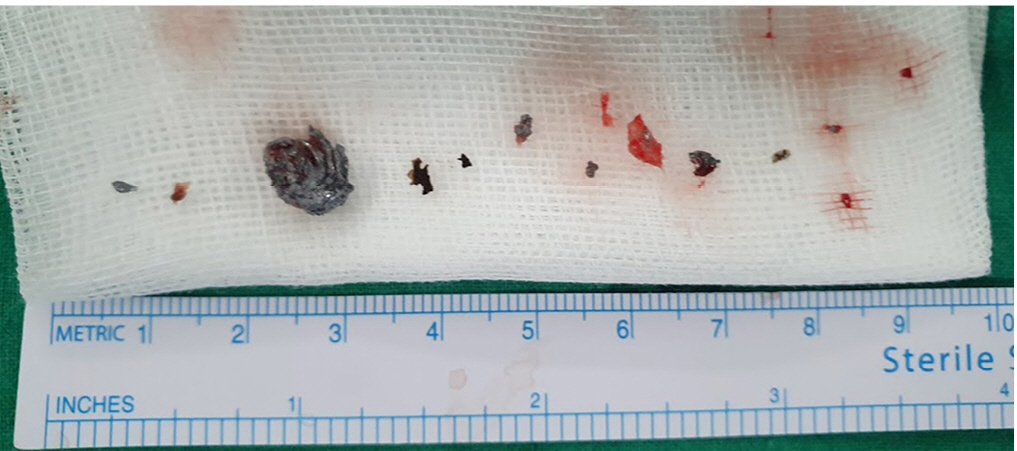
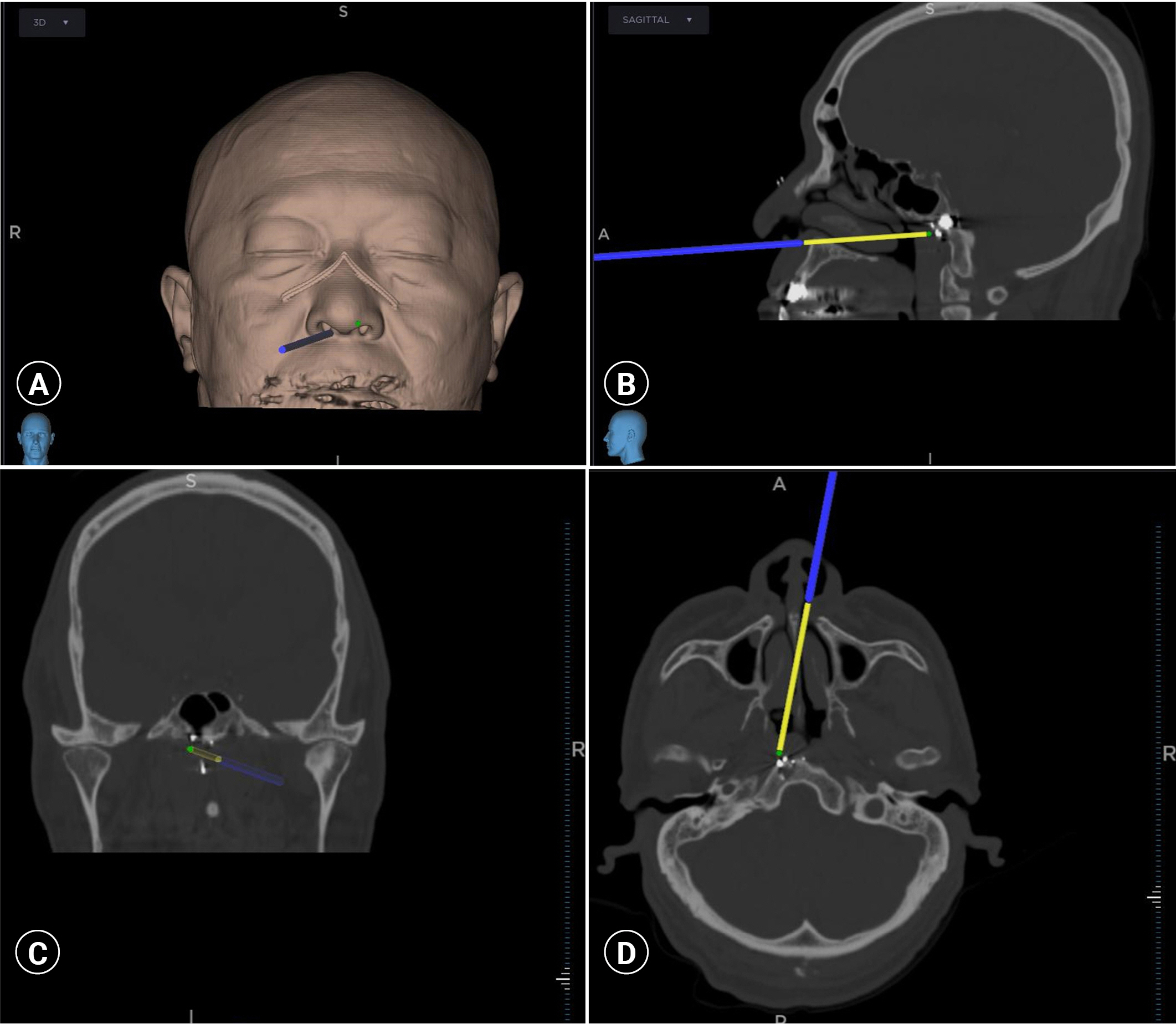
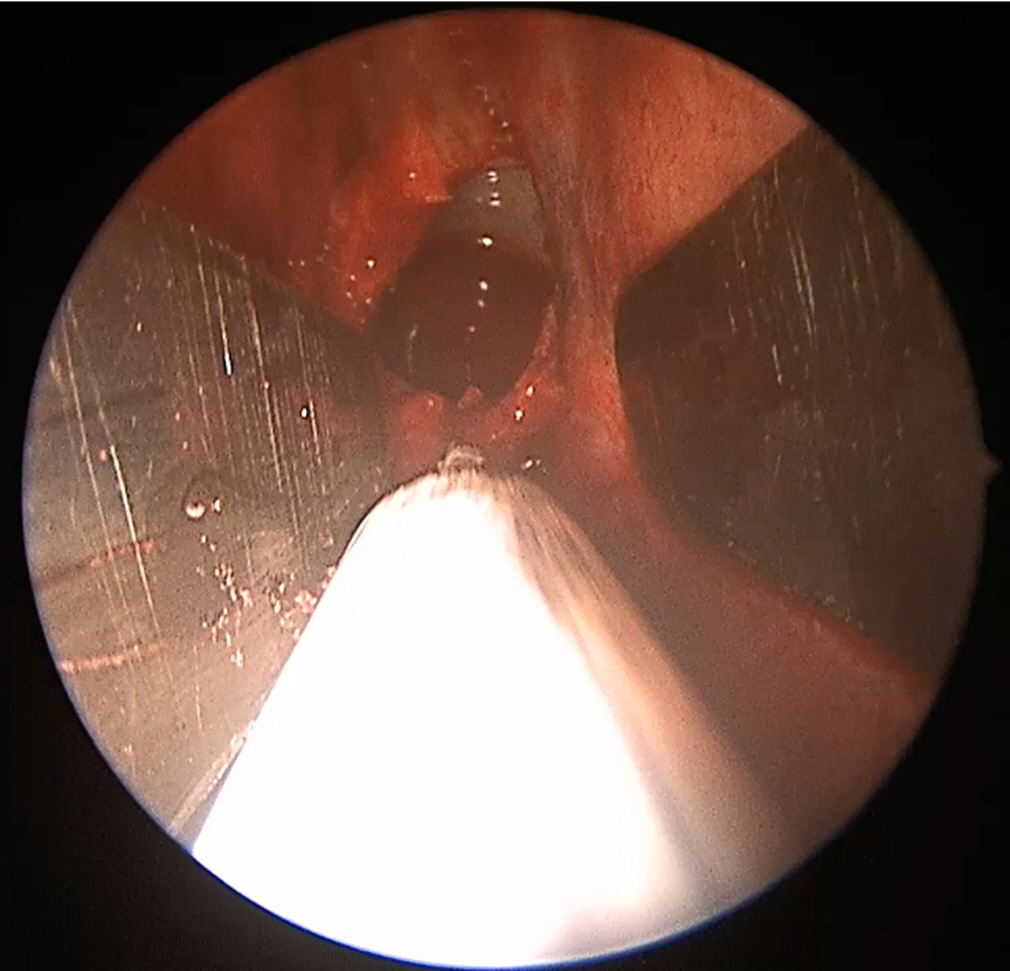
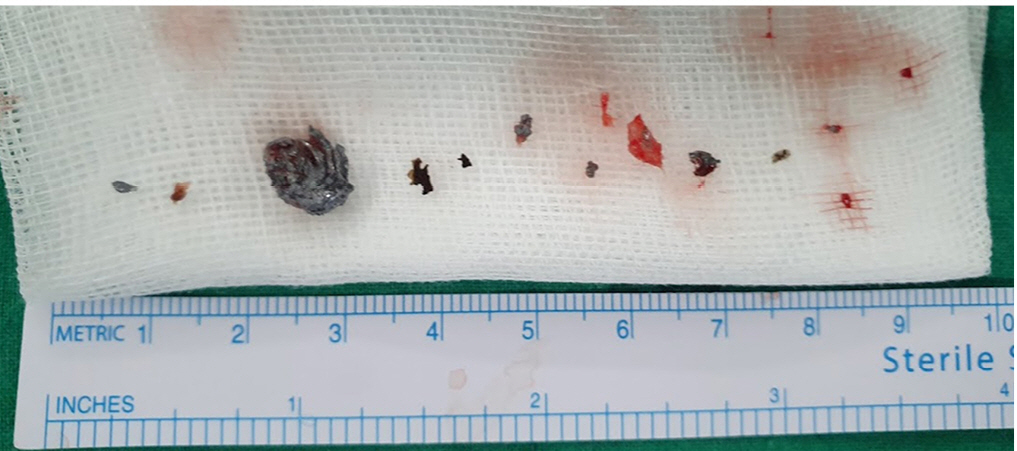
- He had no specific symptoms. On the 6th day after admission, a blood test was performed to check lead level in the blood. His blood lead level was found to be 2.9 μg/dL. Lead bullets were present in bone, a highly vascular tissue. It was forecasted that his blood lead level would increase. We made a plan to remove bullets through surgical treatment. On the day of the surgery, his blood lead level was 3.5 μg/dL. Since many foreign bodies were identified in the clivus, it would be very difficult to access foreign bodies with a general craniotomy. Thus, we planned to remove them through an endoscopic transnasal transclival approach. The location of foreign bodies was confirmed using navigation during preoperative preparation and surgery (Fig. 2). We had access to the clivus under both microscopic and endoscopic fields of view. The endoscope was entered by accessing the mucosal layer through the nose. We confirmed that it was easy to remove foreign bodies using both hands by securing sufficient corridor (Fig. 3). Since the bullet was made of lead, the strength was weak. When it was removed with pituitary forceps, it was crushed. It was judged that the main bullet had to be removed through en bloc. Thus, dissection was performed to expose foreign bodies more fully. Foreign bodies could be removed under a microscopic view (Fig. 4). A bullet with a size of 1 cm was removed. In addition, small foreign bodies identified in the surgical field were removed as much as possible (Fig. 5). Postoperative radiologic findings confirmed that there were almost no foreign bodies left. His blood lead level was found to be 3.8 μg/dL on postoperative 2nd day and 3.6 μg/dL on postoperative 7th day. On the 19th day of admission, the patient was discharged without any signs or specific neurological symptoms. On the 67th day of the accident, blood lead level performed at the outpatient clinic showed no further increase to 3.7 μg/dL. The patient had no specific symptoms.
- This study was approved by the Institutional Review Board of Pusan National University Hospital as a retrospective investigator-initiated trial (No. 2209-018-119). The Institutional Review Board waived the need for informed consent due to the retrospective nature of the study.
CASE REPORT
- Bullets can cause thermal and penetrating injuries due to impact velocities greater than 120 m/sec. Injuries by bullets have higher morbidity and mortality than normal penetrating wounds [7]. When a patient has a CGI, they should be quickly transported to an institution where appropriate treatment can be performed. After hospitalization, neurological evaluations including vital sign check and correction should be performed without any delay. Entry-exit points of the bullet must be checked through a physical examination. After the patient's state is stable, a neuroimage workup should be performed to determine whether and how to perform surgical treatment. Through radiologic findings, damage to the brain parenchyma, hemorrhage, the location and trajectory of the bullet, fracture of the skull, bone fragments penetrated into the brain, and vessels injuries should be checked. In emergency situations, CT and CT angiography are appropriate [8]. However, there are restrictions on the use of magnetic resonance imaging because movement of ferromagnetic materials by magnetic resonance imaging can cause additional damages [9].
- Treatment goals of CGI include immediate lifesaving through bleeding and cerebral decompression, prevention of infection through extensive removal of contaminated, damaged, or ischemic tissue, preservation of nervous tissue through prevention of meningocerebral scars, and anatomical structure restoration through sealing of dura mater and scalp [8]. Tsuei et al. [10] have proposed an algorithm for treating CGI based on Glasgow Coma Scale (GCS), pupillary reflexes, and results of CT scan to determine whether or not to operate.
- In this case, the patient's level of consciousness was alert with GCS 15. He had no symptoms such as infection or cerebrospinal fluid leakage. Bullets were fixed within a solid strong bone structure, clivus. We were contemplated about whether to remove it. After hospitalization, blood lead level should be checked. If it is increased, the decision to remove bullets should be made. In the United States, blood lead level of normal adults is known to be 0.92 μg. Blood lead level is recommended to be less than 5 μg [11]. It was confirmed that his blood lead level was increased compared to his initial level. Thus, it was determined that surgical removal was necessary. A potential complication of remaining bullet fragments is lead poisoning defined as blood lead level above 3.5 μg/dL [12]. There are several case reports suggesting lead poisoning due to remaining bullet fragments in the soft tissue [13,14]. Since it has been reported that remaining bullets could cause lead poisoning, we decided that removal of bullets was absolutely necessary in this case. It is known that remaining bullets within highly vascular tissues such as bone are more likely to cause lead poisoning [15].
- Since the clivus is located deep without intracranial foreign body, hematoma, or injuries, it was judged that an endoscopic transnasal transclival approach was better than a general craniotomy approach. We performed surgery under the navigation to determine the more precise location of small fragments. Based on class III evidence, surgical debridement of the projectile trajectory is not recommended [3]. The major bullet was removed through a microscopic view and an endoscopic view. Even small fragments were removed by maximal curettage at a position that could be confirmed by navigation.
- We report a case of surgical treatment of a CGI caused by lead bullets. This is the first report about a missile injury from the submandibular area to clivus. Since CGI is generally accompanied by neural damage due to anatomical location, a careful evaluation of accompanying intracranial injuries such as hematoma and vascular system along with an appropriate surgical method is required. In particular, multidisciplinary treatment is recommended to safely remove foreign body and minimize complications and neurological sequelae. For a CGI caused by a bullet, serum lead level must be checked. If it is elevated, surgical removal is required. In addition, foreign body of the clivus should be removed vigorously under an endoscopic transnasal transclival approach.
DISCUSSION
-
Ethical statements
This study was approved by the Institutional Review Board of Pusan National University Hospital as a retrospective investigator-initiated trial (No. 2209-018-119). The Institutional Review Board waived the need for informed consent due to the retrospective nature of the study.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: HJC; Data curation: MH, JHL; Methodology: SY, HJC, BCK; Visualization: SY, JHL, BCK; Writing–original draft: MH, HJC; Writing–review & editing: MH, SY, JHL, BCK.
All authors read and approved the final manuscript.
ARTICLE INFORMATION
- 1. Alvis-Miranda HR, M Rubiano A, Agrawal A, et al. Craniocerebral gunshot injuries: a review of the current literature. Bull Emerg Trauma 2016;4:65–74. PubMedPMC
- 2. DeCuypere M, Muhlbauer MS, Boop FA, Klimo P Jr. Pediatric intracranialgunshot wounds: the Memphis experience. J Neurosurg Pediatr 2016;17:595–601. ArticlePubMed
- 3. Part 1. Guidelines for the management of penetrating brain injury. Introduction and methodology. J Trauma 2001;51(2 Suppl):S3–6. PubMed
- 4. Ambrosi PB, Valenca MM, Azevedo-Filho H. Prognostic factors in civiliangunshot wounds to the head: a series of 110 surgical patients and brief literature review. Neurosurg Rev 2012;35:429–35. ArticlePubMedPDF
- 5. Qi H, Li K. Civilian gunshot wounds to the head: a case report, clinical management, and literature review. Chin Neurosurg J 2021;7:12. ArticlePubMedPMCPDF
- 6. Selden BS, Goodman JM, Cordell W, Rodman GH Jr, Schnitzer PG. Outcome of self-inflicted gunshot wounds of the brain. Ann Emerg Med 1988;17:247–53. ArticlePubMed
- 7. Zyck S, Toshkezi G, Krishnamurthy S, et al. Treatment of penetrating nonmissile traumatic brain injury. Case series and review of the literature. World Neurosurg 2016;91:297–307. ArticlePubMed
- 8. Alvis-Miranda HR, Adie Villafane R, Rojas A, Alcala-Cerra G, Moscote-Salazar LR. Management of craniocerebral gunshot injuries: a review. Korean J Neurotrauma 2015;11:35–43. ArticlePubMedPMC
- 9. Esposito DP, Walker JB. Contemporary management of penetrating brain injury. Neurosurg Q 2009;19:249–54. Article
- 10. Tsuei YS, Sun MH, Lee HD, et al. Civilian gunshot wounds to the brain. J Chin Med Assoc 2005;68:126–30. ArticlePubMed
- 11. The National Institute for Occupational Safety and Health (NIOSH). Adult Blood Lead Epidemiology and Surveillance (ABLES) [Internet]. Atlanta: Centers for Disease Control and Prevention (CDC); 2022 [cited 2022 Aug 16]. Available from: https://www.cdc.gov/niosh/topics/ables/default.html.
- 12. Long B, April MD. Are patients with retained bullet fragments at greater risk for elevated blood lead levels? Ann Emerg Med 2020;75:365–7. ArticlePubMed
- 13. James J, Fitzgibbon J, Blackford M. Nausea, vomiting, and weight loss in a young adult patient with a history of a gunshot wound. Pediatr Emerg Care 2016;32:616–8. ArticlePubMed
- 14. Weiss D, Lee D, Feldman R, Smith KE. Severe lead toxicity attributed tobullet fragments retained in soft tissue. BMJ Case Rep 2017;2017:bcr2016217351. ArticlePubMedPMC
- 15. Cristante AF, de Souza FI, Barros Filho TE, Oliveira RP, Marcon RM. Lead poisoning by intradiscal firearm bullet: a case report. Spine (Phila Pa 1976) 2010;35:E140–3. PubMed
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Emergency department laparotomy for patients with severe abdominal trauma: a retrospective study at a single regional trauma center in Korea
- One year of treating patients with open fractures of the lower extremity in a new military trauma center in Korea: a case series
- Experience of surgical treatments for abdominal inferior vena cava injuries in a regional trauma center in Korea
- Delayed diagnosis of popliteal artery injury after traumatic knee dislocation in Korea: a case report
- Endovascular treatment of traumatic iliac venous injury combined with phlegmasia cerulea dolens in Korea: a case report
 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite