A case report of field amputation: the rescue of an entrapped patient through the "doctor car" system
Article information
Abstract
In certain circumstances, invasive procedures such as creation of a surgical airway, insertion of a chest drain, intraosseous puncture, or amputation in the field are necessary. These invasive procedures can save lives. However, emergency medical service teams cannot perform such procedures according to the law in Korea. The upper arm of a 29-year-old male patient was stuck in a huge machine and the emergency medical service team could not rescue the patient. A doctor-car team was dispatched to the scene and the team performed the filed amputation to extricate the patient. He was brought to the trauma center immediately and underwent formal above-elbow amputation. Here we describe a case of field amputation to rescue a patient through a “doctor car” system, along with a literature review.
INTRODUCTION
Prehospital care of patients who have suffered trauma is provided by emergency medical service (EMS) teams in Korea, but the procedures and the usage of medicine by EMS teams are strictly regulated by the law. Therefore, physicians could be needed on the scene in certain cases. In several studies, the presence of physician-staffed helicopters reduced both the time until contact with a physician and the transport time [1–3]. However, the use of physician-staffed helicopters is limited by the cost of operation and is affected by factors such as weather, time, and place. Physician-staffed ambulances (known as “doctor cars” in Korea) were introduced to overcome the limitations of the helicopter in Incheon, Korea. The doctor car is used only for injured patients. The medical team in a doctor car comprises a trauma surgeon, a nurse, a paramedic, and a driver. Doctor cars are equipped with instruments for surgery (e.g., emergency thoracotomy and amputation), medications, and monitoring devices. We report a case of above-elbow amputation in the field in which a doctor car was used to rescue the patient. Written informed consent for publication of the research details and clinical images was obtained from the patient.
CASE REPORT
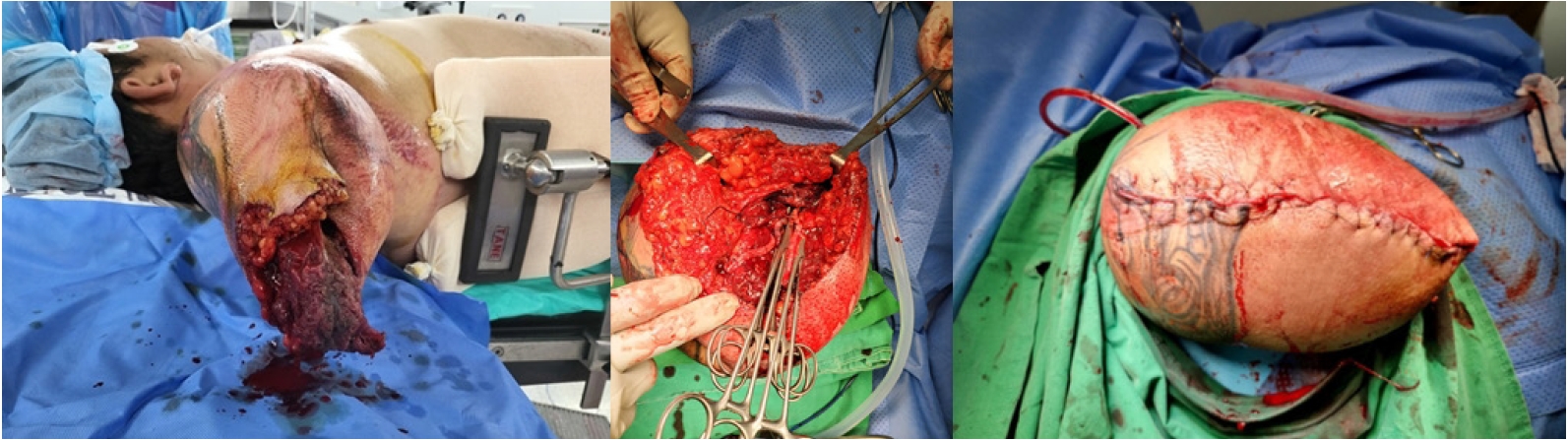
The arm of a 29-year-old male patient was stuck in a huge industrial machine. The EMS team that arrived at the scene found that the patient’s arm was almost completely severed above the elbow, and the remaining part of the arm was trapped between the rollers of the machine (Fig. 1). The EMS team called the regional trauma center and reported that they could not rescue the patient because the machine was too heavy to lift; moreover, they were concerned about a potential massive bleeding after rescue. The patient was alert, and his vital signs were stable; the EMS team found no arterial bleeding. Because the scene was only 17 km away from a regional trauma center and the estimated time of ground transport was approximately 30 minutes, a doctor car, rather than a helicopter, was dispatched by the trauma center to the scene. The trauma team in the car comprised a trauma surgeon, an emergency medicine resident, a trauma nurse, and a driver.
After arrival, the trauma team contacted the patient and confirmed that his vital signs were stable and that he was alert. Tramadol was administered intravenously in the noninjured arm. In the injured arm, the humerus was crushed and severed; only the part of the arm containing the triceps muscle and the brachial vessels and nerve was trapped between the rollers (Fig. 2). The trauma team explained the situation to the patient, and he agreed to undergo immediate amputation. A local anesthetic was administered, the brachial vessel and nerve were clamped and severed, and several minutes later, the part of the arm containing the triceps muscle and remaining skin was divided from the severed part of the arm by a scalpel (Fig. 2). After the procedure, the patient was extricated from the machine. No massive bleeding occurred after amputation, and the trauma team applied compression dressing. The patient was brought to the trauma center in a doctor car; his vital signs remained stable, and he was cooperative during transportation.

The upper arm of the patient was entrapped between rollers and the arm was nearly amputated. Written informed consent for publication of the research details and clinical images was obtained from the patient.
Upon arrival at the trauma center, the patient’s blood pressure was 198/96 mmHg, and his pulse rate was 101 beats/min. After the imaging workup, the patient was brought to the operating room for bleeding control and debridement (Fig. 3). The skin was repaired in a second operation 2 days later. His recovery was uneventful, and he was transferred to the rehabilitation ward.
DISCUSSION
Several reports about successful field amputation and the problems present during physician involvement in rescues have been published [4]. Physicians’ discomfort with fieldwork, poor communications, hierarchy structure, media interaction, and crowd or rescue personnel control are considered problems in at-the-scene amputation [4]. Therefore, a protocol for traumatic amputation is necessary to avoid confusion. However, because of differences in medical practice and situations in different countries, establishing a universal protocol and case scenarios is difficult.
Kampen et al. [5] reported several field amputations: half of the amputations were performed by trauma surgeons, a third by emergency physicians, and the rest by paramedics or other medical professionals. In Korea, paramedics are never allowed to perform any surgical procedures. Because emergency physicians may lack surgical training, experienced trauma surgeons may be the physicians best qualified to perform field amputation in Korea. In circumstances in which airway management, anesthesia, and resuscitation are required, emergency physicians and nurses are the staff best qualified to perform those tasks. Therefore, in situations involving field amputation, the dispatch team should include a trauma surgeon, an emergency physician (or another trauma surgeon), and a trauma nurse.
In 1992, Foil et al. [6] discussed informed consent for field amputation. If the patient is conscious, the situation should be explained, and the risks, benefits, and alternatives should be described; then, with the patient’s consent, the amputation can be performed. If the patient is unconscious and cannot communicate, and if the patient cannot be extricated or otherwise rescued without further trauma, the procedure can be performed with the consent of two physicians. The patient in this report was conscious and immediately agreed to amputation after the trauma surgeon explained the situation; thus, no legal problem regarding the procedure arose.
In this case, equipment such as Gigli saws and bone saws were not needed, but such equipment should be available for field amputation. In addition, opiates and benzodiazepine could not be used because no appropriate protocol for bringing such medications to the field existed. Regulations for prehospital patient care and for the management of opiates should be revised so that doctor cars can be equipped with anesthetics, opiates, and even blood products as medications in the future.
To the best of our knowledge, this is the first report of field amputation in Korea. The procedures that physicians perform at the scene of trauma can save lives. An appropriate protocol concerning trauma team members, equipment, medication, and informed consent for the procedure should be established.
Notes
Ethical statements
Written informed consent for publication of the research details and clinical images was obtained from the patient.
Conflicts of interest
Gil Jae Lee is the Editor-in-Chief, Min A Lee is the Associate Editor, and Kang Kook Choi, Jayun Cho, Seung Hwan Lee are Editorial Board members of Journal of Trauma and Injury, but were not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: all authors; Methodology: GJL, MAL, YCY, SHL; Project administration: JL; Visualization: YCY, KKC, SHL; Writing–original draft: BY; Writing–review & editing: BY, JL, GJL, MAL, JC, YP, JG.
All authors read and approved the final manuscript.