Very large haematoma following the nonoperative management of a blunt splenic injury in a patient with preexisting liver cirrhosis: a case report
Article information
Abstract
The spleen is the most commonly injured organ after blunt abdominal trauma. Nonoperative management (NOM) is the standard treatment for blunt splenic injuries in haemodynamically stable patients without peritonitis. Complications of NOM include rebleeding, new pseudoaneurysm formation, splenic abscess, and symptomatic splenic infarction. These complications hinder the NOM of patients with blunt splenic injuries. We report a case in which a large haemorrhagic fluid collection that occurred after angio-embolisation was resolved by percutaneous drainage in a patient with liver cirrhosis who experienced a blunt spleen injury.
INTRODUCTION
The spleen is the most commonly injured organ after blunt abdominal trauma, mainly because of its highly vascularised parenchyma and anatomic location. Nonoperative management (NOM) is currently the standard treatment for blunt splenic injuries (BSIs) in haemodynamically stable adults and children with no signs of peritonitis [1-3]. NOM includes serial physical examinations, frequent haematocrit measurements, bed rest, and limited oral intake, and it aims to avoid unnecessary surgery and decrease the risk of overwhelming post-splenectomy sepsis [4,5]. With advances in NOM, angio-embolisation (AE) has been introduced to help reduce the need for splenectomy, especially in patients with severe spleen injuries [6,7]. The complications of NOM with AE include rebleeding, new pseudoaneurysm formation, splenic abscess, and symptomatic splenic infarction; the occurrence of these complications may necessitate late splenectomy or radiological intervention [8]. Patients with BSIs who have liver cirrhosis (LC) have higher risks of NOM failure and mortality than those without LC [9]. We report a case in which a very large haematoma occurred in a patient with BSI and alcohol-associated cirrhosis undergoing NOM with AE. The patient was successfully treated with percutaneous drainage alone and did not require surgical intervention.
CASE REPORT
A 42-year-old male patient was transferred to Chonnam National University Hospital via a local hospital 6 hours after a car accident. He had been receiving medication for diabetes and alcohol-associated hepatitis for the last 8 years and had Child-Turcotte-Pugh class A cirrhosis. On arrival, he was alert and his blood pressure was 80/40 mmHg, heart rate was 116 beats per minute, respiratory rate was 20 breaths per minute, body temperature was 36.7°C, and peripheral oxygen saturation was 97%. Transfusion of two units of packed red blood cells had been performed at another hospital. After resuscitation, his blood pressure was 120/80 mmHg. On palpation, the abdomen was soft but mildly distended. He had no concomitant abdominal injury, abdominal tenderness, or signs of peritonitis. Focused assessment with sonography in trauma showed fluid collection in the Morrison’s pouch, splenorenal pouch, and pelvis. Abdominal computed tomography (CT) showed a laceration injury with extravasation of contrast material from the spleen and a large haemoperitoneum (Fig. 1). Celiac arteriography revealed active bleeding in the spleen. The splenic artery branches were embolized using micro-coils and gelatin sponges (Fig. 2). Subsequently, he was admitted to the intensive care unit for close observation. After 3 days in intensive care unit, he was transferred to the general ward because all his vital signs were stable and there were no changes in the laboratory test results and physical examination findings. Abdominal CT performed after 2 weeks of hospitalization showed a very large collection of liquefied haemorrhagic fluid (17×10 cm) in the left subphrenic area that extended up to the area of the splenic injury (Fig. 3). There were no changes in haematocrit levels and abdominal physical examination findings, and the patient’s vital signs were stable. Therefore, we performed percutaneous drainage on the following day, and a significant amount of old blood was drained. Subsequently, a considerable amount of bloody fluid continued to be drained. Abdominal ultrasonography performed after 5 weeks of hospitalization showed improvement of the haematoma in the left subphrenic area, and the percutaneous drain was removed. The patient was discharged on the following day.
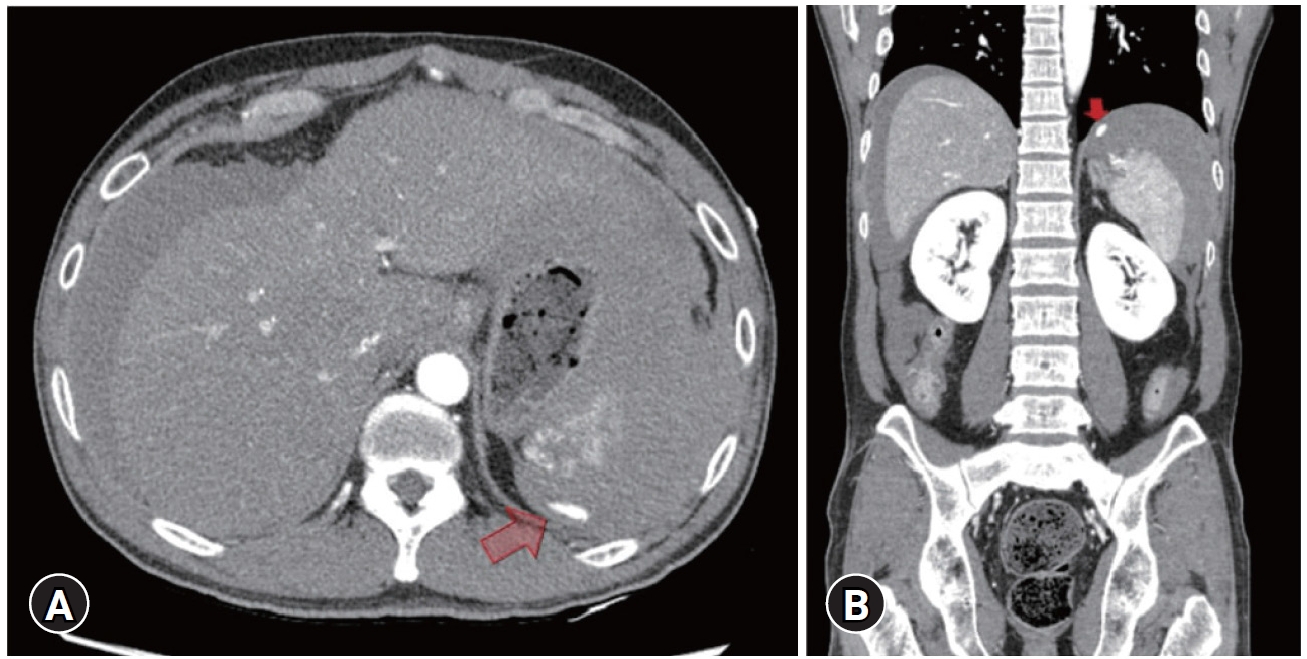
Abdominal computed tomography of (A) axial and (B) coronal view showed a laceration injury with extravasation (arrows) of contrast material in the spleen and a large amount of haemoperitoneum. Written informed consent for the publication of the images was obtained from the patient.

(A) The angiography show active bleeding in the spleen. (B) Embolization of the splenic artery branches using micro-coils and a gelatine sponge was done. Written informed consent for the publication of the images was obtained from the patient.
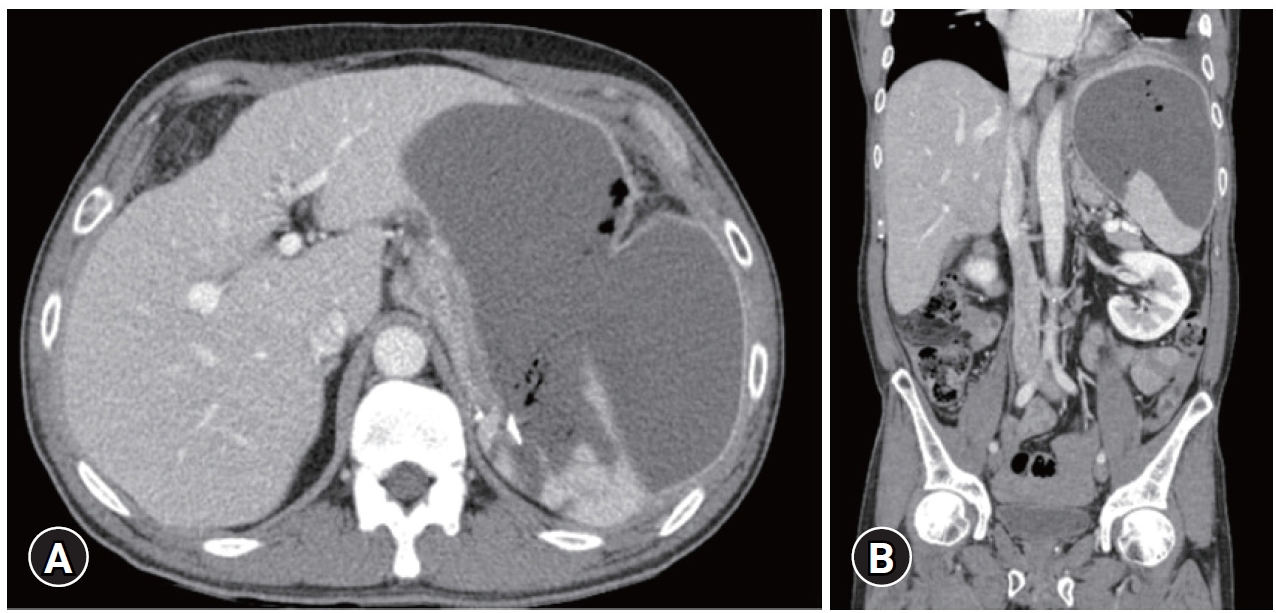
Follow-up computed tomography of (A) axial and (B) coronal view after 2 weeks of hospitalization, showing a large liquefied haemorrhagic fluid collection in the left subphrenic area communicating with the splenic injury. Written informed consent for the publication of the images was obtained from the patient.
DISCUSSION
Over the past 2 decades, NOM has been shown to be an effective option for the management of blunt abdominal injuries in haemodynamically stable patients [1,2]. Recent studies have shown that approximately 65% of adult patients with BSIs received NOM, with the failure rate ranging from 4.2% to 13.0% in appropriately selected cases [10,11]. The predictors of NOM failure include older age, a higher Injury Severity Score, a higher splenic injury grade (grades 4 and 5), need for blood transfusion, CT findings of contrast extravasation or “blush,” and hypotension on admission [12,13]. With the evolution of NOM, AE has been used instead of observation alone in selected patients, especially those with high-grade splenic injuries, to increase the rate of splenic salvage [6,7]. AE seems to be an effective treatment option for patients with CT findings of pseudoaneurysm or contrast extravasation, who have been reported to have the highest risk of ongoing bleeding or subsequent rebleeding. There have been reports of patients developing splenic abscess or symptomatic splenic infarction and requiring late splenectomy or percutaneous intervention [8].
Our patient experienced a grade 3 BSI and showed contrast extravasation on abdominal CT. We performed NOM after AE because the patient became haemodynamically stable after transfusion and resuscitation and had no concomitant extra-abdominal injuries. Abdominal CT performed 2 weeks later showed a large amount of liquefied haemorrhagic fluid in the left subphrenic area. Despite the possibility of rebleeding, the haematoma and necrotic tissue of the spleen seemed to have changed after AE. If abdominal CT had been performed 1 week after AE, this process would have been better seen. Our patient had preexisting alcohol-associated LC (Child-Turcotte-Pugh class A).
Splenomegaly occurs in patients with LC due to portal hypertension-induced venous engorgement, reticuloendothelial cell hyperplasia, fibrogenesis, and increased blood flow through the spleen accompanied by an increased number of peripheral arterioles. Furthermore, most patients with LC have thrombocytopenia and coagulopathy, which have been shown to promote bleeding in both surgical and medical conditions. Moreover, malnutrition, hypoalbuminemia, and hyperbilirubinemia, which are commonly observed in patients with LC, adversely affect the outcomes of patients with various diseases. The effects of LC on patient management and outcomes have not been sufficiently studied. A report published in 2003 analysing 12 patients with BSIs and cirrhosis stated that LC adversely affected both NOM and survival rates, and the NOM salvage rate was only 8% [14]. Another study of 20 patients with BSIs found that LC was associated with high operative rates, low NOM salvage rates (30%), and high surgical morbidity and mortality rates [15]. A recent study (n=160) demonstrated that BSI patients with LC had higher risks of NOM failure (17% vs. 10%) and mortality (23% vs. 6%) than those without LC [9]. Although patients with LC have higher NOM failure rates than those without LC and our patient’s haematoma was very large, considering the benefits of spleen preservation and the risks associated with surgery in patients with LC, we performed percutaneous drainage and collected a large amount of liquefied haemorrhagic fluid. Although the patient was hospitalized for a prolonged time, he recovered and was discharged without any other complications.
In conclusion, clinicians should pay particular attention to NOM failure when performing NOM in patients with LC, even in patients who have low-grade spleen injuries and undergo AE. In the event of complications such as the above case, the risks associated with surgical treatment in patients with LC should be carefully considered.
Notes
Ethical statement
Informed consent was obtained from the patient.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: YJ, YP, JK; Data curation: NL; Methodology: JK; Project administration: NL, HJ; Visualization: HJ; Writing–original draft: EJ; Writing–review&editing: YJ, YP, HJ, NL.
All authors read and approved the final copy of the manuscript.
