Delayed bladder perforation due to screw loosening after pelvic ring injury surgery: a case report
Article information
Abstract
Pelvic ring injuries have high mortality and morbidity rates, and they are difficult to treat because accompanying injuries to the pelvic organs, genitourinary organs, and neurovascular tissues are common. Genitourinary injuries are common comorbid injuries that have been reported to occur in 5% to 6% of all pelvic ring injuries. However, these injuries usually occur simultaneously with the pelvic ring injury, whereas relatively little research has dealt with genitourinary injuries that occur after treatment of a pelvic ring injury. To the best of our knowledge, only three cases of delayed bladder perforation due to screw loosening after symphyseal plate fixation in anterior pelvic ring injury have been reported worldwide, and no such cases have yet been reported in Korea. Since the authors experienced this very rare complication after pelvic ring surgery, we report this case along with a literature review.
INTRODUCTION
Concomitant bladder injuries have been reported to occur in 5% to 6% of pelvic ring injuries [1]; these two injuries usually occur simultaneously. However, relatively little research has investigated delayed genitourinary complications that occur late after surgery. A symphyseal plate is commonly used as a fixation method for anterior pelvic ring injuries. Because it is fixed across the joint, micro-movement occurs, and metal plate breakage or screw loosening is common. To the best of our knowledge, only three cases of bladder perforation due to screw loosening have been reported worldwide [2-4]. Moreover, delayed bladder perforation due to screw loosening after fixation of the symphyseal plate has not been reported in Korea. In this study, we report a case of delayed bladder perforation due to screw loosening after anterior pelvic ring surgery using a symphyseal plate along with a literature review.
CASE REPORT
A 64-year-old male patient was presented to the emergency room after a motorcycle accident. Abdominal pelvic computed tomography showed symphysis pubis diastasis, right superior and inferior ramus fractures, and bilateral anterior and posterior sacroiliac joint injuries (Fig. 1), which corresponded to an anterior posterior compression type III pelvic ring injury. In addition, there was extravasation of the right internal iliac artery branch with hypotension; therefore, emergency angioembolization was performed. Immediately after embolization, orthopedic damage control surgery (supracetabular external fixation) was performed. A Schanz screw was inserted into the supra-acetabular area. The right sacrum, which was more displaced than the left, was reduced using a Schanz screw as a joystick, and a sacroiliac screw was inserted. An external fixation device was then connected.

Initial radiograph showing anterior posterior compression type III pelvic ring injury. (A) A three-dimensional reconstruction view of the pelvis, (B) anteroposterior view of the pelvis, and (C, D) computed tomography axial view. The red circle indicates the crescent fracture. The patient provided written informed consent for publication of the research details and clinical images.
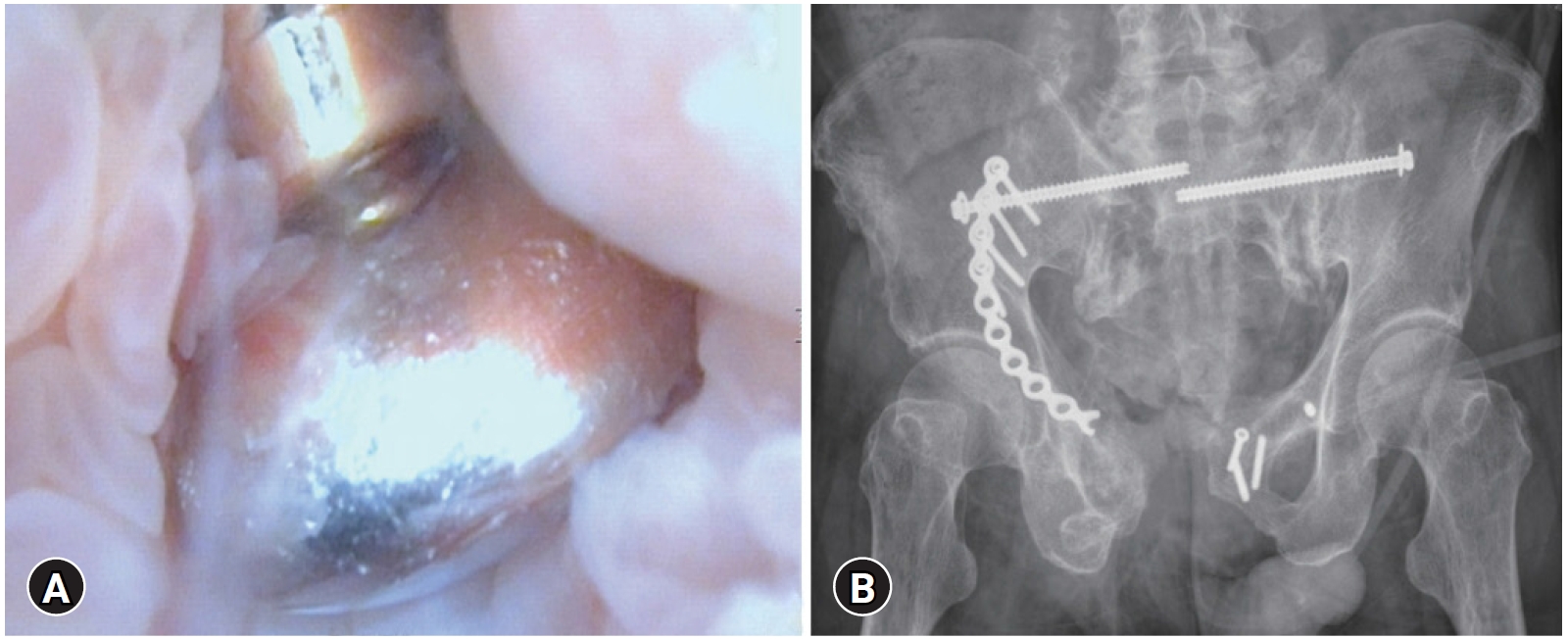
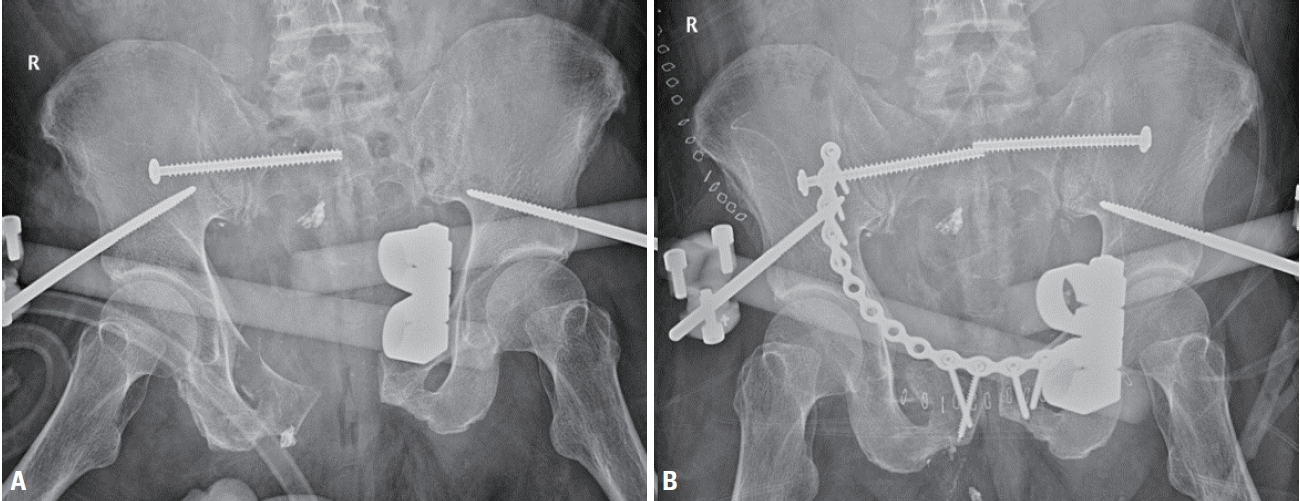
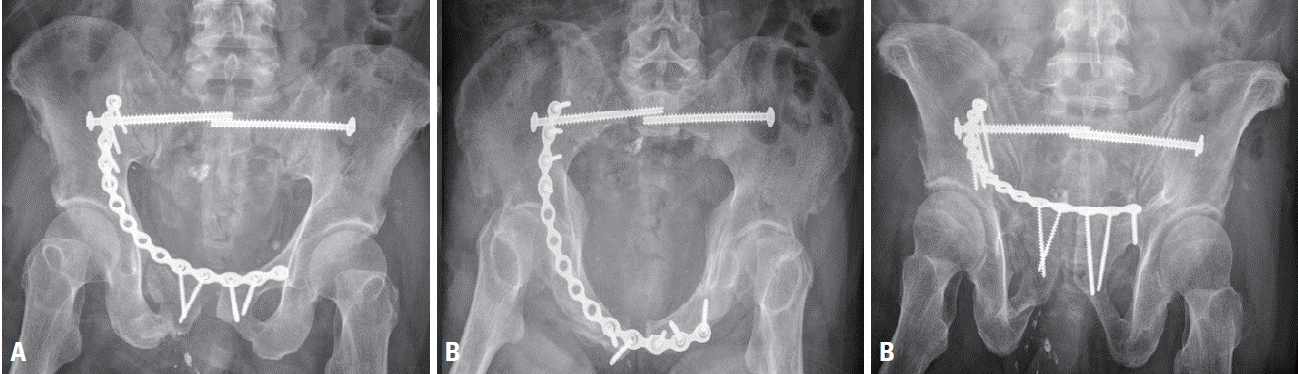
The patient was hemodynamically stabilized, and definitive orthopedic surgery was performed on the 8th day after the injury. Under general anesthesia, the patient was placed in a supine position on a radiolucent table. A sacroiliac screw (7.3 mm cannulated cancellous screw; DePuy Synthes, Raynham, MA, USA) was inserted into the left sacrum. The fracture site was exposed using a modified Stoppa approach. The pubic diastasis was reduced using a bone clamp, and the ramus fracture was naturally reduced due to ligamentotaxis. Fixation was then performed using a symphyseal plate (Matta pelvic plate; Stryker, San Jose, CA, USA). Although there is no significant difference between a conventional plate and a locking plate [5], a conventional plate was used because we assumed that plate breakage was more likely to occur with a locking plate due to the micro-motion of the symphysis pubis. As pubic symphysis diastasis accompanied the ramus fracture, it was fixed with a 14-hole symphyseal plate to obtain sufficient fixation force. The proximal screws were fixed to the ilium through the lateral window (Fig. 2). The external fixator was removed 6 weeks after surgery (Fig. 3) and partial weight-bearing using a walker was started. Loosening of the screw was observed 6 months after surgery, screw breakage and additional loosening were observed 8 months after surgery, and plate breakage was observed 1 year and 5 months after surgery (Fig. 4), but the patient did not complain of any discomfort and was able to walk independently. Hematuria and dysuria occurred 1 year and 10 months after surgery, and the patient visited the urology department. Cystoscopy revealed a screw head. Therefore, after 1 week, under general anesthesia, implant removal and partial cystectomy were performed by an orthopedic surgeon and urology surgeon (Fig. 5). During the procedure, it was found that the symphysis pubis and the bladder were adhered, and an inflammatory reaction was observed. After surgery, hematuria improved, and the patient was able to walk independently.
(A) Eight days after damage control surgery using an external fixator, (B) definitive surgery was performed using a symphyseal plate. The patient provided written informed consent for publication of the research details and clinical images.
After 6 weeks of external fixation, the external fixator was removed. (A) Anteroposterior view of the pelvis, (B) pelvis inlet view, and (C) pelvis outlet view. The patient provided written informed consent for publication of the research details and clinical images.

Symphyseal plate breakage and screw loosening and breakage were observed on (A) pelvis anteroposterior and (B) outlet images 17 months after surgery. The patient provided written informed consent for publication of the research details and clinical images.
DISCUSSION
To the best of our knowledge, only three cases of delayed bladder perforation due to orthopedic implants after pelvic ring injury have been reported worldwide, and this is the first reported case in Korea.
Fridman et al. [2] previously reported a patient with spontaneous voiding of an implant after fixation of the pubic symphysis, which was similar to our case. In the case of Peled et al. [4], there was a bladder injury at the time of injury; therefore, the possibility that the screw entered the injured area could not be excluded. Hosseini et al. [3] also reported a case of delayed bladder perforation due to screw loosening 7 weeks after pelvic surgery, which was treated with cystoscopic screw removal. Unlike the above cases, our case was accompanied by breakage of the symphyseal plate and loosening of the screw, and the presence of a screw in the bladder was confirmed by a cystoscope. Using the previous incision, the broken plate and screws were removed, and the bladder was repaired.
The pubic symphysis is a fibrous joint that connects the pubis, and micromotion occurs during walking. Therefore, when a symphyseal plate is fixed to the anterior pelvic ring, screw loosening, screw breakage, and plate breakage are common [6]. In addition, in this case, a long plate was used because of the diastasis and pubic ramus fracture that caused the unbalanced fixation and likely promoted screw loosening and breakage of the plate. Therefore, we suggest using a 2- or 4-hole-longer plate on the left side to balance the fixation and a dual plate or a ramus screw to increase the strength of fixation.
Although clear timing and indications for symphyseal plate removal have not been established [7], in our case, it is thought that bladder perforation could have been avoided if the plate had been removed at an early stage when screw loosening was observed.
According to the European Association of Urology guidelines [8], hematuria, dysuria, and recurrent urinary tract infections (UTIs) have been suggested as symptoms of unrecognized bladder injury. Kaldenbach and Roth [9] reported hematuria and pain as the main symptoms of delayed bladder injury, which are similar to the symptoms of lower UTIs. The patients in the present case and those in the three cases described above complained of hematuria and dysuria. Therefore, if urinary symptoms appear after orthopedic pelvic surgery, it is necessary to pay close attention to the diagnosis rather than dismiss it as a simple lower UTI.
We report the rare complication of delayed bladder perforation after pelvic ring surgery using a symphyseal plate and suggest that if screw loosening is observed, attention should be paid to urinary symptoms.
Notes
Ethical statement
Informed consent was obtained from the patient.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: HYS; Project administration: JYY; Data curation: JYY, HWK, EJL; Investigation: HYS, JYY, HWK, EJL; Supervision: HYS, JYY, HWK, EJL; Validation : HYS, JYY, HWK, EJL; Writing–original draft: JYY; Writing–review&editing: HYS, JYY, HWK, EJL.
All authors read and approved the final copy of the manuscript.