Articles
- Page Path
- HOME > J Trauma Inj > Volume 34(3); 2021 > Article
-
Original Article
Effects of the Coronavirus Disease 2019 (COVID-19) Pandemic on Outcomes among Patients with Polytrauma at a Single Regional Trauma Center in South Korea -
Sun Hyun Kim, M.D.1,2, Dongyeon Ryu, M.D.1,2, Hohyun Kim, M.D.1,2,3
 , Kangho Lee, M.D.1,2, Chang Ho Jeon, M.D.4, Hyuk Jin Choi, M.D.2,5, Jae Hoon Jang, M.D.2,6, Jae Hun Kim, M.D.1,2,7, Seok Ran Yeom, M.D.2,3,8
, Kangho Lee, M.D.1,2, Chang Ho Jeon, M.D.4, Hyuk Jin Choi, M.D.2,5, Jae Hoon Jang, M.D.2,6, Jae Hun Kim, M.D.1,2,7, Seok Ran Yeom, M.D.2,3,8 -
Journal of Trauma and Injury 2021;34(3):155-161.
DOI: https://doi.org/10.20408/jti.2020.0064
Published online: June 4, 2021
- 3,867 Views
- 120 Download
- 9 Crossref
1Department of Trauma and Surgical Critical Care, Regional Trauma Center, Pusan National University Hospital, Busan, Korea
2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
3Department of Emergency Medicine, Pusan National University School of Medicine, Yangsan, Korea
4Department of Diagnostic Radiology, The Catholic University of Korea Eunpyeong St. Mary’s Hospital, Seoul, Korea
5Department of Neurosurgery, Regional Trauma Center, Pusan National University Hospital, Busan, Korea
6Department of Orthopedic Surgery, Regional Trauma Center, Pusan National University Hospital, Busan, Korea
7Department of General Surgery, Pusan National University School of Medicine, Yangsan, Korea
8Department of Emergency Medicine, Regional Trauma Center, Pusan National University Hospital, Busan, Korea
- Correspondence to Hohyun Kim, M.D. Department of Trauma and Surgical Critical Care, Pusan National University Hospital, 179 Gudeok-ro, Seo-gu, Busan 49241, Korea Tel: +82-51-240-7369 Fax: +82-51-240-7719 E-mail: traumagskhh@gmail.com
Copyright © 2021 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- The coronavirus disease 2019 (COVID-19) pandemic has necessitated a redistribution of resources to meet hospitals’ service needs. This study investigated the impact of COVID-19 on a regional trauma center in South Korea.
-
Methods
- We retrospectively reviewed cases of polytrauma at a single regional trauma center in South Korea between January 20 and September 30, 2020 (the COVID-19 period) and compared them to cases reported during the same time frame (January 20 to September 30) between 2016 and 2019 (the pre-COVID-19 period). The primary outcome was in-hospital mortality, and secondary outcomes included the number of daily admissions, hospital length of stay (LOS), and intensive care unit (ICU) LOS.
-
Results
- The mean number of daily admissions decreased by 15% during the COVID-19 period (4.0±2.0 vs. 4.7±2.2, p=0.010). There was no difference in mechanisms of injury between the two periods. For patients admitted during the COVID-19 period, the hospital LOS was significantly shorter (10 days [interquartile range (IQR) 4–19 days] vs. 16 days [IQR 8–28 days], p<0.001); however, no significant differences in ICU LOS and mortality were found.
-
Conclusions
- The observations at Regional Trauma Center, Pusan National University Hospital corroborate anecdotal reports that there has been a decline in the number of patients admitted to hospitals during the COVID-19 period. In addition, patients admitted during the COVID-19 pandemic had a significantly shorter hospital LOS than those admitted before the COVID-19 pandemic. These preliminary data warrant validation in larger, multi-center studies.
- Coronavirus disease 2019 (COVID-19) has generated serious global public health concerns [1-3]. The COVID-19 outbreak began in Wuhan, China in December 2019, and then rapidly spread worldwide; hence, the World Health Organization declared it a pandemic on March 11, 2020 [4]. In South Korea, the first case was diagnosed on January 20, 2020 [5]. The disruptions caused by the COVID-19 pandemic have necessitated a redistribution of resources to meet hospitals’ service needs.
- The COVID-19 outbreak has posed significant challenges to hospital staff, especially trauma surgeons, who must offer optimal and timely care despite the circumstances [6]. It has been predicted that public adherence to social distancing recommendations made by public health and government officials and avoidance of healthcare institutions and clinics will likely lead to shifts in the epidemiology of severe trauma and other medical conditions [7,8].
- This study examined the effects of the COVID-19 pandemic on outcomes of patients with trauma admitted to a single trauma center in South Korea. We sought to assess differences in hospital length of stay (LOS) for injuries before and during the COVID-19 pandemic. Further, we assessed differences in intensive care unit (ICU) LOS, and mortality before and during the COVID-19 pandemic.
INTRODUCTION
- Study setting
- The regional trauma center at Pusan National University Hospital is the largest trauma center in South Korea, and is a designated level I trauma center. Annually, it receives more than 2,500 trauma-related admissions, including 900–1,000 patients who present with major trauma. The center is equipped with a trauma bay, a 42-bed dedicated trauma ICU, and a trauma angiography suite. Three interventional radiologists and the equipment required for transarterial embolization are available 24 hours a day, 7 days a week.
- We retrospectively reviewed the medical records of patients admitted to this trauma center from January 20 to September 30 between 2016 and 2020. Using the hospital inpatient enquiry system, a total of 7,830 patients with traumatic injuries admitted to Regional Trauma Center, Pusan National University Hospital were selected. This research project received approval from the Research Ethics Board of the Pusan National University Hospital (Approved No. H-2010-015-095) and was therefore performed in accordance with the ethical standards set forth in the 1964 Declaration of Helsinki and its later amendments.
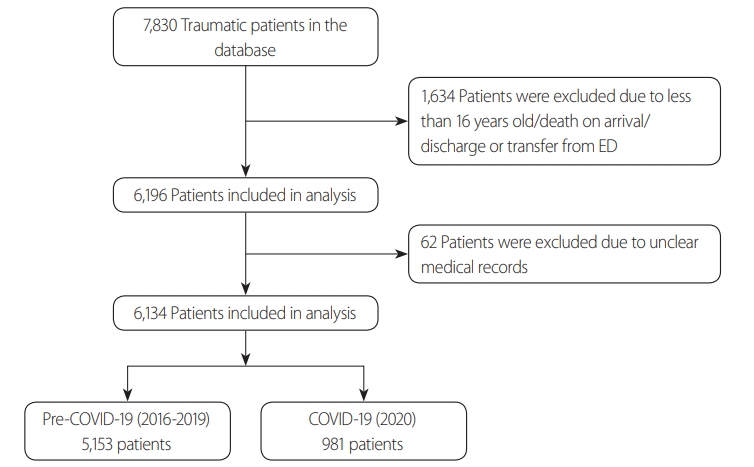
- The exclusion criteria were as follows: patients aged <16 years, those declared dead on arrival, those discharged/transferred from the emergency room, or those with unclear medical records. The final study population included 6,134 patients with traumatic injuries (Fig. 1). Patient demographics, mechanism of injury, and details of injuries were recorded. The available data included age, sex, mechanism of injury, vital signs on arrival, Abbreviated Injury Scale (AIS) score, Injury Severity Score (ISS), Glasgow Coma Scale (GCS) score, Revised Trauma Score (RTS), shock index, length of hospital stay, ICU LOS, and survival status. Patients were compared between the pre-COVID-19 period, which included patients admitted from January 20 to September 30 between 2016 and 2019, and the COVID-19 period, which included patients admitted between January 20, 2020 and September 30, 2020. The first case of COVID-19 was serologically confirmed in South Korea on January 20, 2020; hence, it was considered the start date of the COVID-19 period [9]. The primary transfer time was defined as times from the scene of the injury to the trauma center [10]. Hemodynamic instability was defined as a systolic blood pressure of <90 mmHg and a shock index ≥1.0 on arrival [11].
- Outcome measures
- The objective of this exploratory study was to report the demographic characteristics and clinical outcomes of trauma patients admitted in the pre-COVID-19 and COVID-19 periods. The primary outcome was mortality. The secondary outcomes were the number of daily admissions, hospital LOS, and ICU LOS.
- Statistical analyses
- Summary statistics are reported as the median and interquartile range (IQR) or means with standard deviation (SD) where appropriate. Categorical variables are expressed as number and percentage. The Wilcoxon-rank sum test and unpaired t-test were used to compare the median values of continuous variables and for normally distributed continuous data, respectively. The chi-square test was used to compare frequencies of categorical variables between groups. A p-value of <0.05 was considered to indicate statistical significance. SPSS version 20.0 (IBM Corp., Armonk, NY, USA) and Stata version 14.2 (StataCorp., College Station, TX, USA) were used to analyze the data.
METHODS
- Comparison of demographic characteristics and clinical features between patients admitted during the pre-COVID-19 and COVID-19 periods.
- Of the 7,830 trauma patients admitted during the 5-year study period, 1,696 patients were excluded from the final study population based on the aforementioned criteria. Of the 6,134 patients included, 5,153 were admitted during the pre-COVID-19 period (between 2016 and 2019) and 981 patients were admitted during the COVID-19 period (between January 20, 2020 and September 30, 2020). Table 1 shows the demographic characteristics of patients admitted during the pre-COVID-19 and COVID-19 periods. The daily number of patients admitted to the trauma center was lower during the COVID-19 period than during the pre-COVID-19 period (median 3 days [IQR 3–6 days] vs. 4 days [IQR 3–6 days], p=0.014), representing a mean decrease of 15% during the COVID-19 period (mean 4.0 days [SD 2.2 days] vs. 4.7 days [SD 2.2 days], p=0.010). A comparison of the pre-COVID-19 and COVID-19 periods revealed that patients admitted during the COVID-19 period had a higher proportion of admissions from the scene (58.5% vs. 49.7%, p<0.001), a higher proportion of hemodynamic instability (13.0% vs. 8.6%, p<0.001), and a higher proportion of emergency operations and/or radiologic interventions (34.2% vs. 30.2%, p=0.011). In addition, patients admitted during the COVID-19 period had a longer primary transfer time (52 minutes [IQR 47–88 minutes] vs. 46 minutes [IQR 34–70 minutes], p<0.001), and shorter hospital LOS (10 days [IQR 4–19 days] vs. 16 days [IQR 8–28 days], p<0.001). However, sex, mechanism of injury, heart rate on arrival, shock index, ISS, GCS score, and RTS were not significantly different among patients admitted during the pre-COVID-19 and COVID-19 periods. There was no difference in mortality between the two groups. There have been no cases of nosocomial onset or spread of COVID-19 at Pusan National University Hospital to date.
- Comparison of injury sites between the pre-COVID-19 and COVID-19 periods
- Table 2 shows distribution of injury sites and the most severe injury site during the pre-COVID-19 and COVID-19 periods. Patients admitted during the COVID-19 period had a higher proportion of AIS for the extremities ≥3 than those admitted during the pre-COVID-19 period. In contrast, differences of the proportion of severe head and neck injuries, chest injuries, and abdominal injuries were not statistically significant. Patients admitted during the COVID-19 period had a lower proportion of lung AIS ≥3 (p=0.003) and a lower proportion of kidney AIS ≥3 (p=0.007) than those admitted during the preCOVID-19 period. There were no significant differences in the distribution of rib fractures, liver injuries, spleen injuries, pancreas injuries, pelvic ring injuries, or most severe injury sites between the two groups.
RESULTS
- This study is the first to evaluate the epidemiology and clinical outcomes of patients with trauma before and during the COVID-19 pandemic in South Korea. The main finding of our retrospective observational study is that overall mortality was not significantly different between patients admitted during the COVID-19 period and those admitted during the pre-COVID-19 period. We think that this is because patients who were admitted during the COVID-19 had injuries of comparable severity to those of patients admitted before COVID-19. Furthermore, patients with polytrauma could achieve positive health outcomes with appropriate monitoring and treatment, even during the COVID-19 pandemic. Nonetheless, a larger group of patients and further studies are necessary to draw any definitive conclusions.
- During the COVID-19 period, a trend was found for fewer daily trauma admissions and a shorter hospital LOS (Table 1). Several factors might explain this important observation. First, rigorous public health measures such as social distancing, self-isolation, and quarantining may unintentionally affect established integrated care systems [12-15]. Fear of contracting COVID-19 has also decreased admission rates for common emergencies such as strokes and heart attacks [8,16]. Moreover, the strict instructions to stay at home and fears of infection may have further prevented people from being exposed to the risk of accidents [17]. Stay-at-home orders and suspension of activities have reduced the number of trauma incidents, including traffic collisions [10,15]. COVID-19 quarantines have reduced the volume of trauma patients who are transported by emergency medical services (EMS). For these reasons, the daily number of trauma admissions may have been reduced during the COVID-19 pandemic in our study. In addition, patients with milder symptoms may intentionally avoid staying in the hospital, preferring to be discharged early because of fears of infection within a medical facility.
- The COVID-19 pandemic represents a novel challenge for EMS, and it affects the practice of prehospital and hospital trauma resuscitation [6,12,15,18]. The COVID-19 outbreak has posed significant challenges to paramedics and hospital staff, who must offer optimal and timely care despite the circumstances [6]. Strict safety protocols must be adhered to while providing emergency care for patients with trauma [6,19]. However, personal protective equipment such as face shields, goggles, and gloves can reduce the visual, auditory, and tactile senses of healthcare staff, thus reducing the precision of emergency care [19,20]. Our study showed that the proportion of patients who received emergency operations and/or radiologic interventions was higher during the COVID-19 period than in the pre-COVID-19 period (p=0.011). We think that this was likely due to an increase in referrals of patients requiring emergency operations and/or radiologic interventions during the COVID-19 period.
- Limitations
- Our study is an initial analysis of the volume of patient admissions for trauma during a short period of time, and its scope is limited. There are several other limitations to this study. For example, the study was confined to patients at a single center and from a specific region; it also analyzed a population of patients who required the services of a regional trauma center. The severity and frequency of injuries seen at Regional Trauma Center, Pusan National University Hospital likely differ significantly from those seen at community emergency departments.
DISCUSSION
- This study assessed the epidemiology of trauma patients at a single institution during the pre-COVID-19 and COVID-19 periods. There was a decline in the number of patients admitted to the regional trauma center during the COVID-19 pandemic compared to that before the COVID-19 pandemic. In addition, patients admitted during the COVID-19 pandemic had a significantly shorter hospital LOS than those admitted before the COVID-19 pandemic. With appropriate monitoring and treatment, patients with polytrauma can achieve comparable outcomes, even during the COVID-19 pandemic. These preliminary data warrant validation in larger, multi-center studies, and more studies are needed to evaluate and compare long-term outcomes in patients with polytrauma before and during the COVID-19 pandemic.
CONCLUSION
Values are presented as mean±standard deviation, number (%), or median (interquartile range). Study period: 20 January to 30 September. Hemodynamic instability is defined as SBP <90 mmHg and shock index ≥1.0 on arrival.
COVID-19: coronavirus disease 2019, IQR: interquartile range, SBP: systolic blood pressure, BPM: beats per minute, ISS: Injury Severity Score, GCS: Glasgow Coma Scale, RTS: Revised Trauma Score, ED: emergency department, ICU: intensive care unit, LOS: length of stay.
- 1. Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol 2020;49:717–26. ArticlePubMed
- 2. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. ArticlePubMed
- 3. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–4. ArticlePubMedPMC
- 4. Huang C, Wang Y, Li X, Ren L, Zhao J, H Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. ArticlePubMedPMC
- 5. Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci 2020;35:e61. ArticlePubMedPMC
- 6. Li Y, Zeng L, Li Z, Mao Q, Liu D, Zhang L, et al. Emergency trauma care during the outbreak of corona virus disease 2019 (COVID-19) in China. World J Emerg Surg 2020;15:33. ArticlePubMedPMC
- 7. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2. ArticlePubMedPMC
- 8. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852–3. ArticlePubMed
- 9. Cavallo JJ, Forman HP. The economic impact of the COVID-19 pandemic on radiology practices. Radiology 2020;296:E141–4. ArticlePubMed
- 10. Davies G, Chesters A. Transport of the trauma patient. Br J Anaesth 2015;115:33–7. ArticlePubMed
- 11. Loggers SAI, Koedam TWA, Giannakopoulos GF, Vandewalle E, Erwteman M, Zuidema WP. Definition of hemodynamic stability in blunt trauma patients: a systematic review and assessment amongst Dutch trauma team members. Eur J Trauma Emerg Surg 2017;43:823–33. ArticlePubMed
- 12. Nuñez JH, Sallent A, Lakhani K, Guerra-Farfan E, Vidal N, Ekhtiari S, et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury 2020;51:1414–8. ArticlePubMedPMC
- 13. Kenanidis E, Tsiridis E. “Flattening the curve” of COVID-19 pandemic in orthopaedics and trauma: the Greek perspective. Injury 2020;51:1681–2. ArticlePubMedPMC
- 14. Zhu W, Li X, Wu Y, Xu C, Li L, Yang J, et al. Community quarantine strategy against coronavirus disease 2019 in Anhui: an evaluation based on trauma center patients. Int J Infect Dis 2020;96:417–21. ArticlePubMedPMC
- 15. Yang F, Lu X. The effect of COVID-19 on trauma system in one city of China. Scand J Trauma Resusc Emerg Med 2020;28:57. ArticlePubMedPMC
- 16. Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis 2020;29:104953. ArticlePubMedPMC
- 17. Pellegrini M, Roda M, Di Geronimo N, Lupardi E, Giannaccare G, Schiavi C. Changing trends of ocular trauma in the time of COVID-19 pandemic. Eye (Lond) 2020;34:1248–50. ArticlePubMedPMC
- 18. Motterle G, Morlacco A, Iafrate M, Bianco M, Federa G, Xhafka O, et al. The impact of COVID-19 pandemic on urological emergencies: a single-center experience. World J Urol 2021;39:1985–9. ArticlePubMed
- 19. Søreide K, Hallet J, Matthews JB, Schnitzbauer AA, Line PD, Lai PBS, et al. Immediate and longterm impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg 2020;107:1250–61. ArticlePubMedPMC
- 20. Wang Y, Zeng L, Yao S, Zhu F, Liu C, Di Laura A, et al. Recommendations of protective measures for orthopedic surgeons during COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc 2020;28:2027–35. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- Patientensicherheit bei differenzierter (innerklinischer) Schockraumaktivierung für Schwerverletzte
S. Hagel, K. R. Liedtke, S. Bax, S. Wailke, T. Klüter, P. Behrendt, G. M. Franke, A. Seekamp, P. Langguth, A. Balandin, M. Grünewald, D. Schunk
Die Unfallchirurgie.2023; 126(6): 441. CrossRef - Characteristics of Patients With Traumatic Brain Injury in a Regional Trauma Center: A Single-Center Study
Mahnjeong Ha, Seunghan Yu, Byung Chul Kim, Jung Hwan Lee, Hyuk Jin Choi, Won Ho Cho
Korean Journal of Neurotrauma.2023; 19(1): 6. CrossRef - Changes in Injury Pattern and Outcomes of Trauma Patients after COVID-19 Pandemic: A Retrospective Cohort Study
Myungjin Jang, Mina Lee, Giljae Lee, Jungnam Lee, Kangkook Choi, Byungchul Yu
Healthcare.2023; 11(8): 1074. CrossRef - Análise do atendimento primário de pacientes vítimas de violência interpessoal e autodirigida durante a pandemia da COVID-19
HELOÍSA MORO TEIXEIRA, ANGEL ADRIANY DA-SILVA, ANNE KAROLINE CARDOZO DA-ROCHA, MARIANA ROTHERMEL VALDERRAMA, RAFAELLA STRADIOTTO BERNARDELLI, VITÓRIA WISNIEVSKI MARUCCO SILVA, LUIZ CARLOS VON BAHTEN
Revista do Colégio Brasileiro de Cirurgiões.2023;[Epub] CrossRef - Analysis of primary care of victims of interpersonal and self inflicted violence during the COVID-19 pandemic
HELOÍSA MORO TEIXEIRA, ANGEL ADRIANY DA-SILVA, ANNE KAROLINE CARDOZO DA-ROCHA, MARIANA ROTHERMEL VALDERRAMA, RAFAELLA STRADIOTTO BERNARDELLI, VITÓRIA WISNIEVSKI MARUCCO SILVA, LUIZ CARLOS VON BAHTEN
Revista do Colégio Brasileiro de Cirurgiões.2023;[Epub] CrossRef - Comparison of Clinical Characteristics of Traumatic Brain Injury Patients According to the Mechanism Before and After COVID-19
Jonghyun Sung, Jongwook Choi, Kum Whang, Sung Min Cho, Jongyeon Kim, Seung Jin Lee, Yeon gyu Jang
Korean Journal of Neurotrauma.2023; 19(3): 307. CrossRef - Outcomes improvement despite continuous visits of severely injured patients during the COVID-19 outbreak: experience at a regional trauma centre in South Korea
Sooyeon Kang, Ji Eun Park, Ji Wool Ko, Myoung Jun Kim, Young Un Choi, Hongjin Shim, Keum Seok Bae, Kwangmin Kim
BMC Emergency Medicine.2022;[Epub] CrossRef - Impact of the COVID-19 pandemic on the epidemiology of traffic accidents: a cross-sectional study
ANGEL ADRIANY DA SILVA, GABRIELA REDIVO STRÖHER, HELOÍSA MORO TEIXEIRA, MARIA VICTÓRIA GUTIERREZ CORDEIRO, MARCIA OLANDOSKI, LUIZ CARLOS VON-BAHTEN
Revista do Colégio Brasileiro de Cirurgiões.2022;[Epub] CrossRef - Impacto da pandemia da COVID-19 na epidemiologia dos acidentes de trânsito: um estudo transversal
ANGEL ADRIANY DA SILVA, GABRIELA REDIVO STRÖHER, HELOÍSA MORO TEIXEIRA, MARIA VICTÓRIA GUTIERREZ CORDEIRO, MARCIA OLANDOSKI, LUIZ CARLOS VON-BAHTEN
Revista do Colégio Brasileiro de Cirurgiões.2022;[Epub] CrossRef
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


