Prevalence of posttraumatic stress disorder in orthopedic trauma patients and a call to implement the Injured Trauma Survivor Screen as a prospective screening protocol in the United States
Article information
Abstract
Purpose
Posttraumatic stress disorder (PTSD) is prevalent and is associated with protracted recovery and worse outcomes after injury. This study compared PTSD prevalence using the PTSD checklist for DSM-5 (PCL-5) with the prevalence of PTSD risk using the Injured Trauma Survivor Screen (ITSS).
Methods
Adult trauma patients at a level I trauma center were screened with the PCL-5 (sample 1) at follow-up visits or using the ITSS as inpatients (sample 2).
Results
Sample 1 (n=285) had significantly fewer patients with gunshot wounds than sample 2 (n=45) (8.1% vs. 22.2%, P=0.003), nonsignificantly fewer patients with a fall from a height (17.2% vs. 28.9%, P=0.06), and similar numbers of patients with motor vehicle collision (40.7% vs. 37.8%, P=0.07). Screening was performed at a mean of 154 days following injury for sample 1 versus 7.1 days in sample 2. The mean age of the patients in sample 1 was 45.4 years, and the mean age of those in sample 2 was 46.1 years. The two samples had similar proportions of female patients (38.2% vs. 40.0%, P=0.80). The positive screening rate was 18.9% in sample 1 and 40.0% in sample 2 (P=0.001). For specific mechanisms, the positive rates were as follows: motor vehicle collisions, 17.2% in sample 1 and 17.6% in sample 2 (P>0.999); fall from height, 12.2% in sample 1 and 30.8% in sample 2 (P=0.20); and gunshot wounds, 39.1% in sample 1 and 80.0% in sample 2 (P=0.06).
Conclusions
The ITSS was obtained earlier than PCL-5 and may identify PTSD in more orthopedic trauma patients. Differences in the frequency of PTSD may also be related to the screening tool itself, or underlying patient risk factors, such as mechanism of injury, or mental or social health.
INTRODUCTION
Background
The prevalence of posttraumatic stress disorder (PTSD) in patients with traumatic injuries has been studied extensively and has been shown to substantially exceed rates in the general population [1]. Following orthopedic injury, PTSD prevalence ranges from 19.5% to 51% [2–5] Several studies have found various negative effects of PTSD and/or depression on recovery, including worse general health status, increased likelihood of taking opioids, and worse functional outcomes after ankle fracture, as well as more frequent secondary operations [4–7]. Related healthcare expenses are also higher in the presence of concurrent mental illness [8,9]. It is vital to identify patients who develop PTSD after injury and offer resources expeditiously to effectively improve and mitigate these negative outcomes [10].
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) PTSD diagnosis requires experiencing symptoms for 1 month after the injury or event: at least one re-experiencing symptom, at least one avoidance symptom, at least two arousal and reactivity symptoms, and at least two cognition and mood symptoms [11]. The Injured Trauma Survivor Screen (ITSS) is a nine-item screening tool in a yes/no format that can be administered immediately following injury to predict the risk of developing depression and PTSD independently [12,13]. Furthermore, the nine-item, yes/no format of the ITSS enables it to be administered efficiently, which may help overcome obstacles (e.g., lack of time) that have been reported to prevent screening for psychological illness in trauma patients [10].
Objectives
The objective of this study was to determine the prevalence of PTSD in orthopedic trauma patients using the current standard of screening—the PTSD checklist for DSM-5 (PCL-5) at 1 month or more posttrauma—and compare it to screening with the ITSS. We hypothesized that the ITSS will predict PTSD at a rate similar to the PCL-5 used to diagnose PTSD, and that the ITSS may be more efficient than the PCL-5.
METHODS
Ethics statement
This study was approved by the Institutional Review Board of MetroHealth (No. IRB00000685) with a waiver for informed consent.
Sample 1: orthopedic trauma patients screened with the PCL-5
Participants
A total of 524 adult patients presenting to the outpatient orthopedic clinic at an urban level I trauma center following orthopedic trauma injury between March 1, 2019, and December 31, 2021, were screened with the PCL-5.
Measures
The PCL-5 is a commonly used, validated diagnostic tool for diagnosing PTSD (Material S1). The PCL-5 is a 20-item self-report survey, with a score ranging from 0 to 80. The survey includes a rating from 0 (“not at all”) to 5 (“extremely”) for each item. The National Center for PTSD indicates that from preliminary research, a score of 31 to 33 indicates probable PTSD [14]. For this patient population, the upper limit of this range (33) was considered a positive screening.
Additional demographic data were collected retrospectively through Epic (Epic Systems Corp) including age, sex, mechanism of injury, injury characteristics (type of fracture and single vs. polytrauma), and time (in days) between date of injury and date of screening.
Procedure
PCL-5 questionnaires were handed to patients presenting to their outpatient trauma clinic appointments to be completed as a self-assessment. All patients had been previously hospitalized for an acute injury episode. The current DSM-5 criteria require a minimum of 1 month following injury to qualify for a PTSD diagnosis. Thus, 222 patients of the original 524 were excluded, leaving 302 patients. Seventeen of those patients had an incomplete screening, declined screening, or were unable to complete the screening, leaving 285 patients included in the analysis as sample 1.
Sample 2: orthopedic trauma patients screened with the ITSS
Participants
A total of 45 patients admitted for orthopedic trauma between June 22, 2021 and March 21, 2022, at the same level I trauma center were included in this sample. The exclusion criteria for ITSS administration comprised patients with an age under 18 years, major neurocognitive impairment, active psychotic and/or manic episode, non-English speaking, acute intoxication, under arrest, presentation for suicide attempt, presentation for intentional self-inflicted injury, fall from standing, and inability to communicate. All other patients from the general trauma admission list with at least one fracture were included. The total population of orthopedic trauma patients who were screened with the ITSS within the above time frame was 45 patients.
Measures
The ITSS is a postinjury screening tool to identify PTSD risk prior to discharge from the initial injury hospitalization (Material S2). The ITSS is administered to patients by trained personnel guiding the screening and reading the questions out loud to the patient. The ITSS has a yes (1) or no (0) format for each question, with an overall score of greater than or equal to 2 indicating a positive screen for PTSD risk.
Additional demographic data were collected retrospectively through Epic including age, sex, mechanism of injury, injury characteristics (type of fracture and single vs. polytrauma), and time (in days) between date of injury and date of screening.
Procedure
On admission to the inpatient unit at an average of 7.1 days postinjury, patients in this sample were screened using the ITSS. Since the ITSS can be administered immediately after injury, no screenings had to be excluded from the population based on the timing of administration. A follow-up screen for patients who were screened with the ITSS should occur at outpatient visits or by phone at least 1 month after the initial screening, and should include the PCL-5, Patient Health Questionnaire-9, and the Columbia-Suicide Severity Rating Scale (C-SSRS), if indicated. Due to logistical issues and protocol changes regarding the administration of the C-SSRS, these follow-up screens were not completed at the time of this report.
Statistical analysis
All data are presented using descriptive statistics. Groups were compared using the chi-square test or Fisher exact test for small groups.
RESULTS
Patients were screened with the PCL-5 (sample 1) or the ITSS (sample 2). Fig. 1 shows a timeline for when the different screening tools can be administered. Sample 1, screened using the PCL-5 (n=285), had a mean age of 45.4 years. In total, 109 patients (38.2%) were female, 127 (44.6%) experienced polytrauma, and the average time between the date of injury and the administration of the PCL-5 screen was 154 days (approximately 5 months) (Table 1). The percentage of positive screens on the PCL-5 for orthopedic trauma patients in sample 1 was 18.9%. Sample 2, screened using the ITSS (n=45), had a mean age of 46.1 years. Eighteen patients (40.0%) were female, 17 (37.8%) experienced polytrauma, and the average time between the date of injury and the administration of the ITSS was 7.1 days (Table 2). The percentage of positive PTSD screens on the ITSS for orthopedic trauma patients in sample 2 was 40.0%.
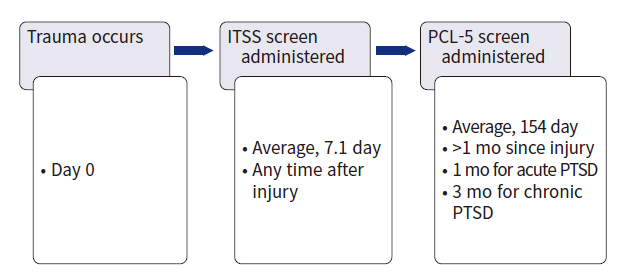
Timeline of posttraumatic stress disorder (PTSD) screening. ITSS, Injured Trauma Survivor Screen; PCL-5, PTSD checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
The two samples had similar numbers of female patients (38.2% in sample 1 vs. 40.0% in sample 2, P=0.80) and polytrauma patients (44.6% vs. 37.8%, P=0.40). The most prevalent mechanism of injury for the sample 1 population was motor vehicle collision, followed by fall from standing/sitting, fall from height, and then gunshot wound (GSW). The most prevalent mechanism of injury for the sample 2 population was motor vehicle collision, followed by fall from height and then GSW. Sample 1 had significantly fewer patients with GSW than sample 2 (8.1% vs. 22.2%, P=0.003), trended towards fewer patients with a fall from a height (17.2% vs. 28.9%, P=0.06), and had similar numbers of patients with motor vehicle collision (40.7% vs. 37.8%, P=0.70) (Table 3).
The rate of positive screens in sample 1 (54 of 285, 18.9%) compared with sample 2 (18 of 45, 40.0%) was significantly different (P=0.001). In patients injured in a motor vehicle collision, the overall positive rate (a positive screen on either the ITSS or PCL-5) was 17.3%, and this rate was similar in both groups (17.6% of patients injured in a motor vehicle collision in sample 2 screened positive with the ITSS and 17.2% in sample 1 screened positive with the PCL-5, P>0.999 from the Fisher exact test). For patients injured from a fall from a height, the overall positive rate was 16.1% (30.8% with a positive ITSS and 12.2% with a positive PCL-5, P=0.20 from the Fisher exact test). For those injured by a GSW, the overall positive rate was higher (51.5%), with a trend toward a higher rate in sample 2 than in sample 1 (80.0% with a positive ITSS and 39.1% with a positive PCL-5, P=0.06 from the Fisher exact test) (Table 4).
DISCUSSION
PTSD is a prevalent diagnosis after orthopedic trauma injuries and can impair outcomes after injury [1–7]. Although a large body of evidence has identified the prevalence of PTSD and its impact on recovery, a standardized protocol for follow-up care, including additional screenings, does not exist. Despite an understanding of the impact of mental health on recovery and clinical outcomes, research addressing psychological conditions after orthopedic trauma has been lacking. Vranceanu et al. [10] found that while most orthopedic surgeons were likely to notice psychological illness in their patients, a much smaller proportion were likely to screen or refer patients for psychological illness. Lack of time was found to be a primary barrier for screening and referring for psychological illness.
This study observed that 18.9% of orthopedic trauma patients presented with PTSD using the PCL-5 at outpatient visits, whereas 40.0% of orthopedic trauma patients were identified as having PTSD risk using the ITSS at initial inpatient presentation. We propose that PTSD would be identified and treated in a greater proportion of the orthopedic trauma population if the ITSS had been administered in the studied time frame. The gap between positive-risk ITSS screenings and positive PCL-5 screenings indicates that only administering the PCL-5 may lead to missing patients at risk of developing PTSD. The ITSS can identify patients at risk for PTSD before the recommended 1-month waiting period, as defined by the DSM-5. If screened earlier, patients could receive support and services at that time. The ITSS has been shown to be effective in predicting PTSD and depression risk. Hunt et al. [12,13] studied the utility of the ITSS in predicting depression and PTSD in trauma patients and found high sensitivity and specificity at both 1 month and 6 months postinjury. If proper interventions are completed, improvement in functional outcomes in these patients and prevention of the future negative impacts of their PTSD diagnosis may be possible. Furthermore, it is not feasible nor warranted to provide additional support to every orthopedic trauma patient, and therefore the ITSS can help by identifying the most at-risk patients to provide supportive resources.
Following GSW, 80.0% of patients screened positive for PTSD risk on the ITSS, while only 39.1% of patients screened positive with the PCL-5. Similarly, 30.8% of patients screened positive on the ITSS after fall from a height, while only 12.2% screened positive on the PCL-5. These findings could be explained in two ways. First, many trauma-exposed patients tend to follow a natural trajectory of psychological recovery; thus, these patients may not develop PTSD even with early risk factors. Second, these patients may go on to develop PTSD, but were less likely to follow-up and therefore were not screened with the PCL-5. This indicates that for certain mechanisms, like GSW or fall from a height, the ITSS could be profoundly useful in identifying those patients early and ensuring expeditious PCL-5 administration to diagnose PTSD after injury.
Administering a self-report screener like the PCL-5 during outpatient visits does capture PTSD symptoms and provides an opportunity to connect patients immediately to resources. However, this approach has several limitations. Some patients may have limited literacy, and completing a self-assessment about their symptoms may be unreasonable, resulting in PTSD symptoms being overlooked. Specifically, 19% of adults in the United States are reported to function at the lowest level of literacy [15]. This is a crucial issue to consider when administering patient screenings. In addition, patients may not be able to hold these forms or fill them out due to the nature of their injury. Additionally, as PTSD is a condition of avoidance, these patients may be more likely to be lost to follow-up and avoid attending future appointments. For these reasons, while the PCL-5 is an effective and accurate tool for determining patients with PTSD after traumatic injury, there are several flaws and limitations to its use that may prevent optimal care for patients with PTSD after injury.
A robust ITSS protocol addresses many of these limitations. By asking patients the questions verbally rather than having them complete a self-assessment, the barrier of low literacy in the screened population can be mitigated. Furthermore, this can help ensure that the patient understands the screening is related to the presenting trauma and not an amalgamation of many past experiences. Furthermore, if patients cannot complete a form by hand due to their injury, the ITSS can be more easily completed. The ITSS is also administered immediately after injury without delay. The ITSS is also a very rapid tool to administer that takes only 5 minutes to complete and has nine questions. This would add very little additional time, and many staff members, not only doctoral-level providers, could administer this screener (Fig. 2).
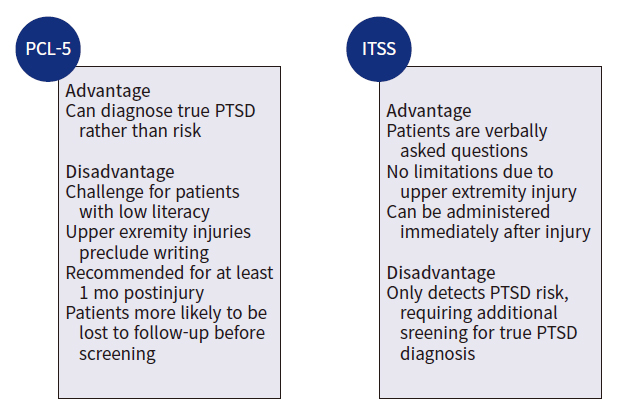
Advantages and disadvantages of the posttraumatic stress disorder (PTSD) checklist for DSM-5 (PCL-5) versus the Injured Trauma Survivor Screen (ITSS).
Given the nature of PTSD, early intervention after trauma may help prevent PTSD development. In one study [16], patients were randomly assigned to receive early intervention after trauma compared to assessment only. The intervention group reported significantly lower posttraumatic stress reactions at 4- and 12-week postinjury, and lower depressive symptoms at 4 weeks, with the effect strongest for victims of sexual assault. However, a follow-up study [17] comparing PTSD symptoms and depression in three groups (one session of intervention, three sessions of intervention, or assessment only) found no differences. While there are conflicting results on the impact of early intervention, it is plausible that early intervention can help mitigate PTSD symptoms. In addition, this indicates that targeted approaches may be needed based on the trauma type, as some types of trauma are more strongly associated with PTSD development [16]. Another study [18] found that early intervention mitigated PTSD symptoms even if patients had a genetic polymorphism deemed high risk for PTSD development. PTSD symptoms correlated with genetic risk for the group without intervention, but there was no correlation in the intervention group, suggesting that intervention negated genetic risk. Therefore, early intervention may help certain high-risk patients mitigate PTSD symptom development, even if predisposing genetic factors are at play.
In early 2022, the American College of Surgeons (ACS) released updated verification guidelines [19], which include mental health screening and referral after injury. Unfortunately, there are no standardized screening methods for PTSD among trauma centers in the United States. A handful of screening tools have been tested in isolated samples to screen patients for PTSD after developing symptoms [20–27]. Many trauma centers incorporate screening using one of these tools in some capacity. However, there is little formality or protocol in how screens are administered or handled, and all trauma centers for active PTSD.
Limitations
This study does have several limitations. First, our samples were small and heterogeneous. Sample 2 had more GSW patients with high severity of injury, which may carry a risk for greater likelihood of a positive screen. Additionally, a score on the PCL-5 of 33 was defined as being positive for PTSD, following the National Center for PTSD updated guidelines; this cutoff was chosen to obtain a population that was as accurate as possible, but this cutoff is still arbitrary [20]. Notably, we were unable to obtain follow-up screenings for our ITSS population. Due to system logistical and protocol issues with the C-SSRS, we had to cease screenings and were unable to complete follow-ups that would confirm PTSD diagnoses, as the ITSS is a screener for PTSD risk only. Follow-up C-SSRS data would have added strength to this study and potentially confirmed that the ITSS identified true PTSD diagnoses early. However, the ITSS has been found in several existing studies to be both sensitive and specific [12,13].
Conclusions
The ITSS would ensure a more standardized process that does not require any waiting period between injury and administration. The PCL-5 is still a crucial tool in monitoring PTSD symptoms and true PTSD diagnoses. However, we suggest adding the ITSS protocol to identify at-risk patients earlier and administer indicated support and interventions.
Notes
Author contributions
Data curation: VJN; Formal analysis: all authors; Funding acquisition: VPH; Investigation: all authors; Methodology: MAB; Project administration: MAB, HAV; Writing–original draft: VJN, HAV; Writing–review & editing: MAB, VPH, HAV. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no other conflicts of interest to declare.
Funding
Vanessa P. Ho is supported by the Clinical and Translational Science Collaborative (CTSC) of Cleveland (No. KL2TR002547 from the National Center for Advancing Translational Sciences [NCATS] component of the US National Institutes of Health and NIH Roadmap for Medical Research).
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
Supplementary materials
Material S1.
PTSD checklist for DSM-5 (PCL-5) survey.
Material S2.
Injured Trauma Survivor Screen (ITSS).
Supplementary materials are available from https://doi.org/10.20408/jti.2023.0068.




