Articles
- Page Path
- HOME > J Trauma Inj > Volume 30(4); 2017 > Article
-
Case Report
Indirect Reduction and Spinal Canal Remodeling through Ligamentotaxis for Lumbar Burst Fracture - Wu Seong Kang, M.D.1, Jung Chul Kim, M.D.1, Ik Sun Choi, M.D.2, Sung Kyu Kim, M.D.2
-
Journal of Trauma and Injury 2017;30(4):212-215.
DOI: https://doi.org/10.20408/jti.2017.30.4.212
Published online: December 30, 2017
- 5,452 Views
- 66 Download
1Divison of Trauma Surgery, Department of Surgery, Chonnam National University Hospital, Gwangju, Korea
2Department of Orthopedics, Chonnam National University Hospital, Gwangju, Korea
- Correspondence to: Sung Kyu Kim, M.D., Department of Orthopedics, Chonnam National University Hospital, 42 Jebong-ro, Dong-gu, Gwangju 61469, Korea, Tel: +82-62-227-1640, Fax: +82-62-225-7794, E-mail: bonjourksk@hanmail.net
• Received: October 18, 2017 • Revised: November 15, 2017 • Accepted: November 16, 2017
Copyright © 2017 The Korean Society of Trauma
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- The choice of the most appropriate treatment for thoracolumbar or lumbar spine burst fracture remains controversial from conservative treatment to fusion through a posterior or anterior approach. There are many cases where ligamentotaxis is used to reduce the burst fracture. However, indirect reduction using ligamentotaxis is often limited in the magnitude of the reduction that it can achieve. In our patient with severe burst fracture, we were able to restore an almost normal level of vertebral height and secure spinal canal widening by using only ligamentotaxis by posterior instrumentation. Before the operation, the patient had more than 95% encroachment of the spinal canal. This was reduced to less than 10% after treatment.
- There are many ways in choosing surgical treatment method for burst fracture of the thoracolumbar or lumbar spine. In selecting surgical treatment, surgeon must consider how much the vertebral body is comminuted, the loss of vertebral height, the sagittal plane alignment changes, and how much the fractured vertebral fragments have retropulsed and invaded the spinal canal. One of the key factors for treatment of burst fracture is the reduction or resolution of the posterior fractured fragments that is retropulsed in the spinal canal. Methods for reducing fractured fragments include ‘direct reduction’ by directly pressing the fractured fragment into initial position and ‘indirect reduction’ using ligamentotaxis. The indirect reduction method is more secure than the direct reduction, but there is some limitation to the reduction completely. Here, we report a case in which a patient with a spinal canal encroachment of 95% or more was reduced almost to normal through intraoperative indirect reduction and spontaneous spinal canal remodeling during follow-up eight months.
INTRODUCTION
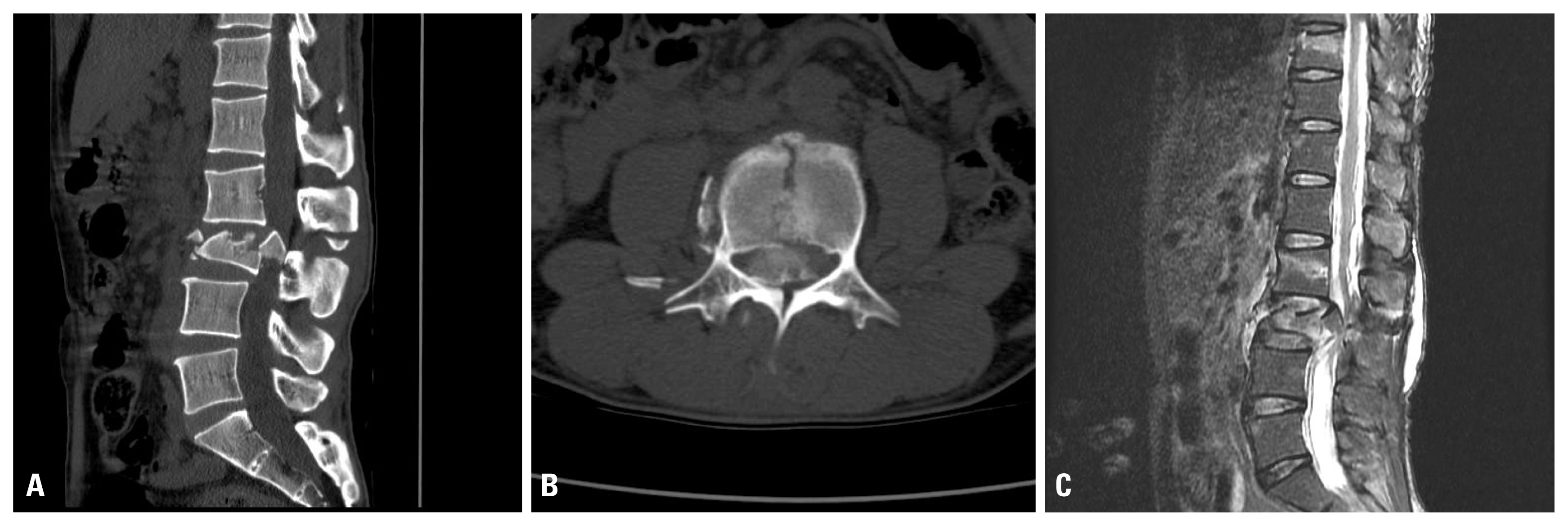
- A 48-year-old male patient with lower back pain and right lower leg pain had tenderness at the 3rd lumbar vertebra (L3) area on physical examination. Plain radiographs showed a 45% decrease in the anterior height of the L3 vertebral body, and computed tomography (CT) showed that posterior fractured fragments were retropulsed into more than 95% of the spinal canal (Fig. 1A, B). On magnetic resonance imaging, the retropulsed fragments almost completely compressed the dura (Fig. 1C). However, surprisingly, the patient’s motor function was greater than grade IV in the lower leg as a whole, and sensory testing showed tingling and hypesthesia in the right lower limb. The bulbocavernous reflex, perianal sense and anal tone were normal.
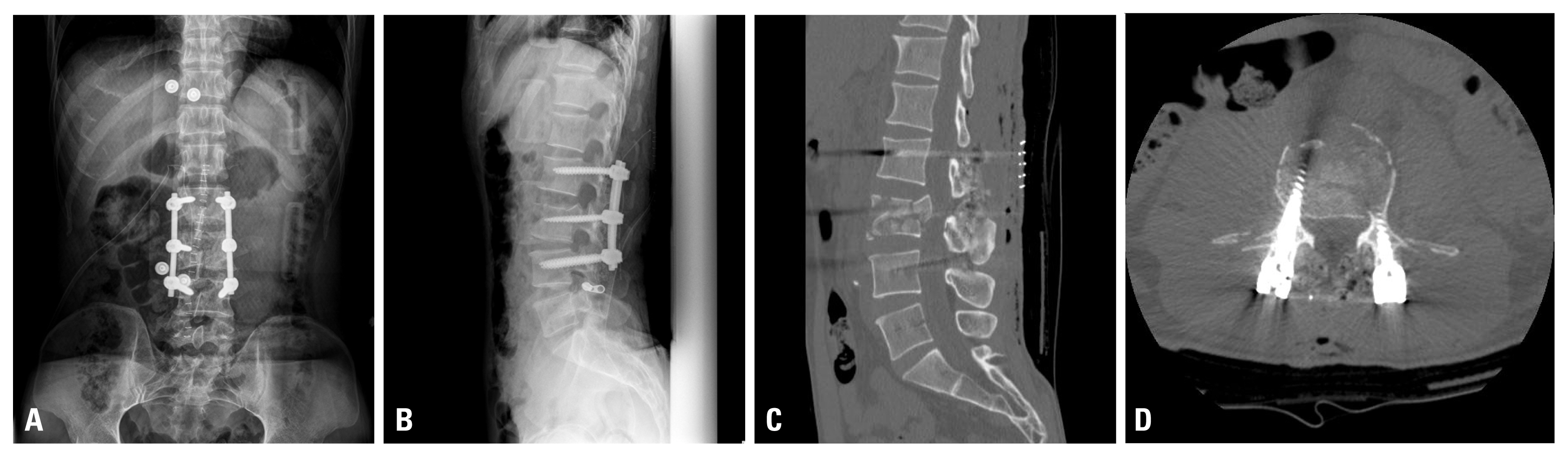
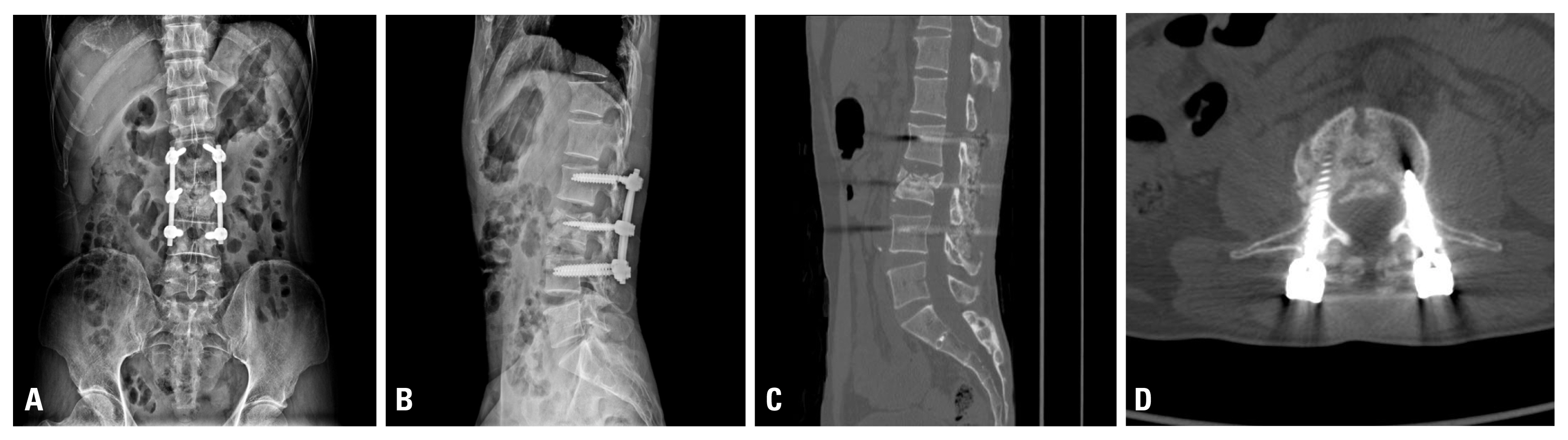
- The operation was planned to perform in two stages. The first stage was performed on the day of admission. L3 was reduced and a posterior fusion was done at L2-3-4. The second stage operation (L3 anterior reconstruction) was planned to be performed if the anterior column of the L3 body is found to be unstable during follow-up. A wide range of hematomas and soft tissue injuries were identified at the L2-3-4 level along skin incision. The pedicle screw was inserted into L2 and L4, and indirect reduction was performed by distraction after connecting the rod. After insertion of the L3 pedicle screw, and further distraction was performed between L2-3 because the location of retropulsed fragments was mainly between L2 and L3 pedicle. The left L3 screw was used as 35 mm length because there was a possibility of L3 anterior reconstruction through a left retroperitoneal approach in the second stage of operation. Posterior fusion, including facet fusion, was performed using an allobone graft. After surgery, the vertebra recovered 100% of its original height, and the spinal canal was widened by more than 50% on CT (Fig. 2). The patient was discharged on the 25th postoperative day. His motor function did not change, and his right lower leg hypesthesia slightly improved. Eight months after surgery, CT scans showed that the bone fragments in the spinal canal were absorbed and restored to almost normal levels (less than 10% encroachment), and the vertebral height was slightly decreased (Fig. 3). At the last follow-up X-ray and CT, we believed that additional anterior reconstruction was not necessary. On the lateral plain radiograph, breakage of the L2 right pedicle screw was observed. It was considered that the posterior fusion between L2 and L3 was incomplete. However, the patient is now walking well, and there have not been any other changes in symptoms. We will continue to observe.
CASE REPORT
- Thoracolumbar or lumbar burst fracture is a common trauma that can cause spinal cord or nerve injury because of the impact on the anterior and middle column of the vertebra when a vertical load is applied [1]. Generally, fragment excision and anterior reconstruction surgery are recommended for patients with severe spinal canal involvement. However, indirect reduction with ligamentotaxis of the posterior longitudinal ligament can also be used to treat thoracolumbar or lumbar burst fractures [2,3]. According to Mueller et al. [4], the spinal canal of patients with a thoracolumbar burst fracture has been widened by about 10% compared to preoperative cases, and spinal canal stenosis remained postoperatively in most cases. At levels below L3, indirect reduction using ligamentotaxis had poor outcomes due to weak posterior longitudinal ligament. On average 6% widening of spinal canal was observed. Only one case (L4 fracture) showed 23% spinal canal widening [5]. Wang et al. [6] reported that reduction was not well achieved when the displacement distance between fractured fragment and vertebral body was greater than 8.5 mm or the rotation angle was greater than 55 degrees.
- In our case, the spinal canal was almost blocked preoperatively. At eight months after surgery, the canal width was 90% of normal. We achieved good reduction even though the displacement distance was about 13 mm, the rotation angle was about 61 degrees, and the ligamentotaxis force of the posterior longitudinal ligament at L3 level was weak. The success of the initial reduction was probably due to the relatively young age of the patient, his thin body type, and good bone density, and also the short time between injury and surgery. Compared with the spinal canal status immediately after the operation, spinal canal remodeling seems to be a reason of additional widening of the spinal canal at postoperative eight months. According to Moon and Lee [7], canal remodeling was influenced by postoperative distraction or comminuted type of fracture. Canal remodeling was thought to be caused by cord pulsation of the thecal sac and venous pulsation of the anterior internal longitudinal plexus, but a clear mechanism has not been elucidated.
- In this case, the patient’s vertebral height and spinal canal were restored nearly to normal levels through indirect reduction and canal remodeling after a burst fracture with very severe spinal canal encroachment. There have been many reported cases of spinal canal widening using indirect reduction. Nevertheless, there has been no reported case of nearly complete reduction and canal remodeling after a thoracolumbar or lumbar burst fracture with more than 95% spinal canal encroachment. The successful results at the eight-month follow-up were thought to be due to the younger age of the patient, the short time between the injury and the surgery, thin body type, good bone density, and canal remodeling. Therefore, indirect reduction with ligamentotaxis may show good results in selective case among patients with thoracolumbar or lumbar burst fracture.
DISCUSSION
Fig. 1(A) Preoperative sagittal CT of a 48-year-old man showing a severe L3 burst fracture and 45% decrease of anterior vertebral height. (B) Preoperative axial CT showing more than 95% encroachment of spinal canal. (C) Preoperative sagittal magnetic resonance imaging showing compression of the cauda equina by a fractured vertebral fragment and a long subcutaneous hemorrhage of the back. CT: computed tomography.


Fig. 2(A) Postoperative anteroposterior and (B) lateral plain radiograph showing significant restoration of the anterior vertebral height. (C) Postoperative sagittal and (D) axial CT showing canal decompression compared with the preoperative axial CT view. CT: computed tomography.
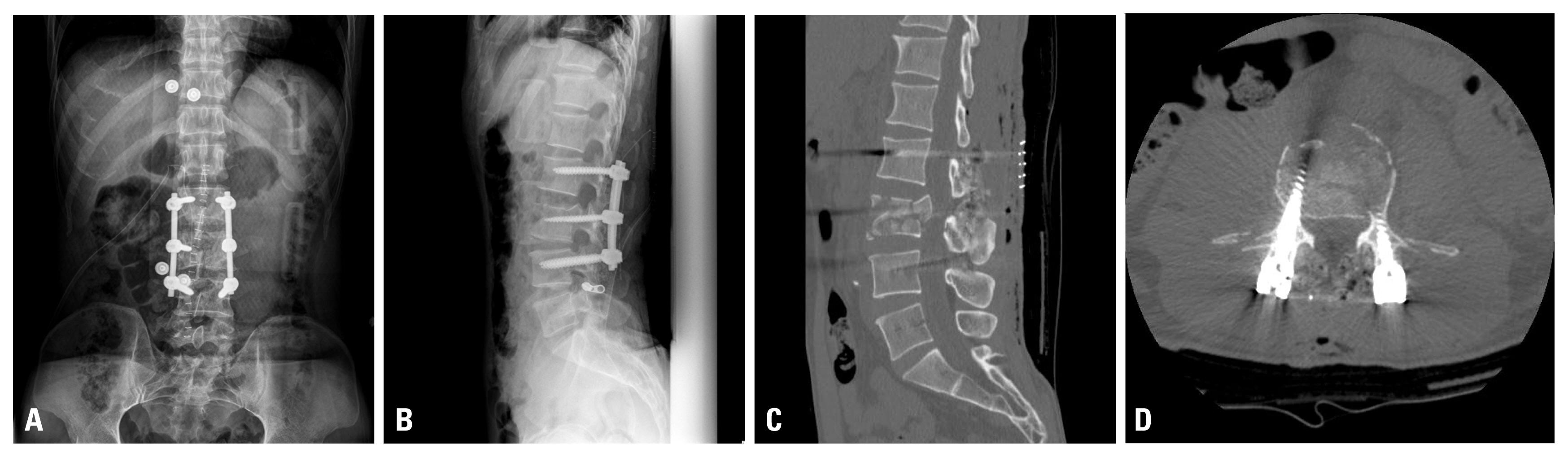
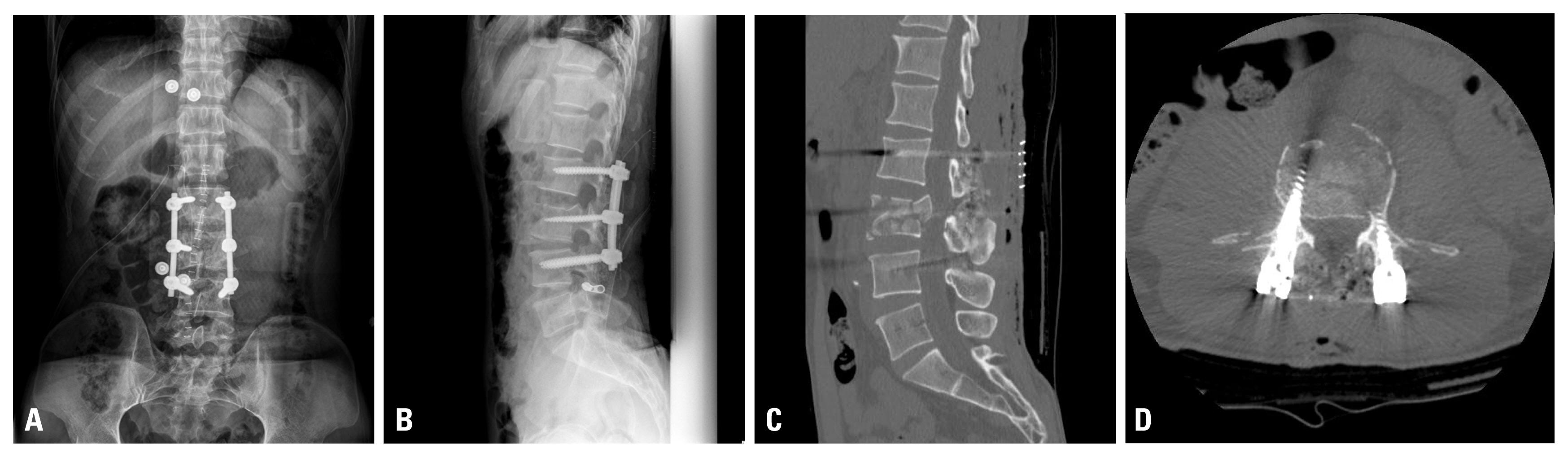
Fig. 3(A) Anteroposterior and (B) lateral plain radiograph of a patient at eight months after surgery showing almost normal anterior vertebral height. (C) Eight months follow-up sagittal and (D) axial computed tomography showing 90% widened state of the spinal canal.


- 1. Seykora P, Beck E, Daniaux H, Pallua A, Kathrein A, Lang T. The value of closed reduction of fractures of the lower thoracic and lumbar spine and computerized tomography follow-up. Unfallchirurgie 1993;19:267–71.ArticlePubMedPDF
- 2. Jeong WJ, Kim JW, Seo DW, Lee HJ, Kim JY, Yoon JP, et al. Efficiency of ligamentotaxis using PLL for thoracic and lumbar burst fractures in the load-sharing classification. Orthopedics 2013;36:e567–74.ArticlePubMed
- 3. Yang H, Shi JH, Ebraheim M, Liu X, Konrad J, Husain I, et al. Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J 2011;20:380–6.ArticlePubMedPDF
- 4. Mueller LA, Mueller LP, Schmidt R, Forst R, Rudig L. The phenomenon and efficiency of ligamentotaxis after dorsal stabilization of thoracolumbar burst fractures. Arch Orthop Trauma Surg 2006;126:364–8.ArticlePubMedPDF
- 5. Kuner EH, Kuner A, Schlickewei W, Mullaji AB. Ligamentotaxis with an internal spinal fixator for thoracolumbar fractures. J Bone Joint Surg Br 1994;76:107–12.ArticlePubMed
- 6. Wang XB, Lü GH, Li J, Wang B, Lu C, Phan K. Posterior distraction and instrumentation cannot always reduce displaced and rotated posterosuperior fracture fragments in thoracolumbar burst fracture. Clin Spin Surg 2017;30:E317–22. Article
- 7. Moon YJ, Lee KB. Relationship between clinical outcomes and spontaneous canal remodeling in thoracolumbar burst fracture. World Neurosurg 2016;89:58–64.ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite