Articles
- Page Path
- HOME > J Trauma Inj > Volume 37(1); 2024 > Article
-
Original Article
Comparison of mortality between open and closed pelvic bone fractures in Korea using 1:2 propensity score matching: a single-center retrospective study -
Jaeri Yoo, MD
 , Donghwan Choi, MD
, Donghwan Choi, MD , Byung Hee Kang, MD
, Byung Hee Kang, MD
-
Journal of Trauma and Injury 2024;37(1):6-12.
DOI: https://doi.org/10.20408/jti.2023.0063
Published online: January 3, 2024
- 756 Views
- 20 Download
Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- Correspondence to Byung Hee Kang, MD Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, 206 World cup-ro, Yeongtong-gu, Suwon 16499, Korea Tel: +82-31-219-7764 Email: kbhname@gmail.com
© 2024 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Open pelvic bone fractures are relatively rare and are considered more severe than closed fractures. This study aimed to compare the clinical outcomes of open and closed severe pelvic bone fractures.
-
Methods
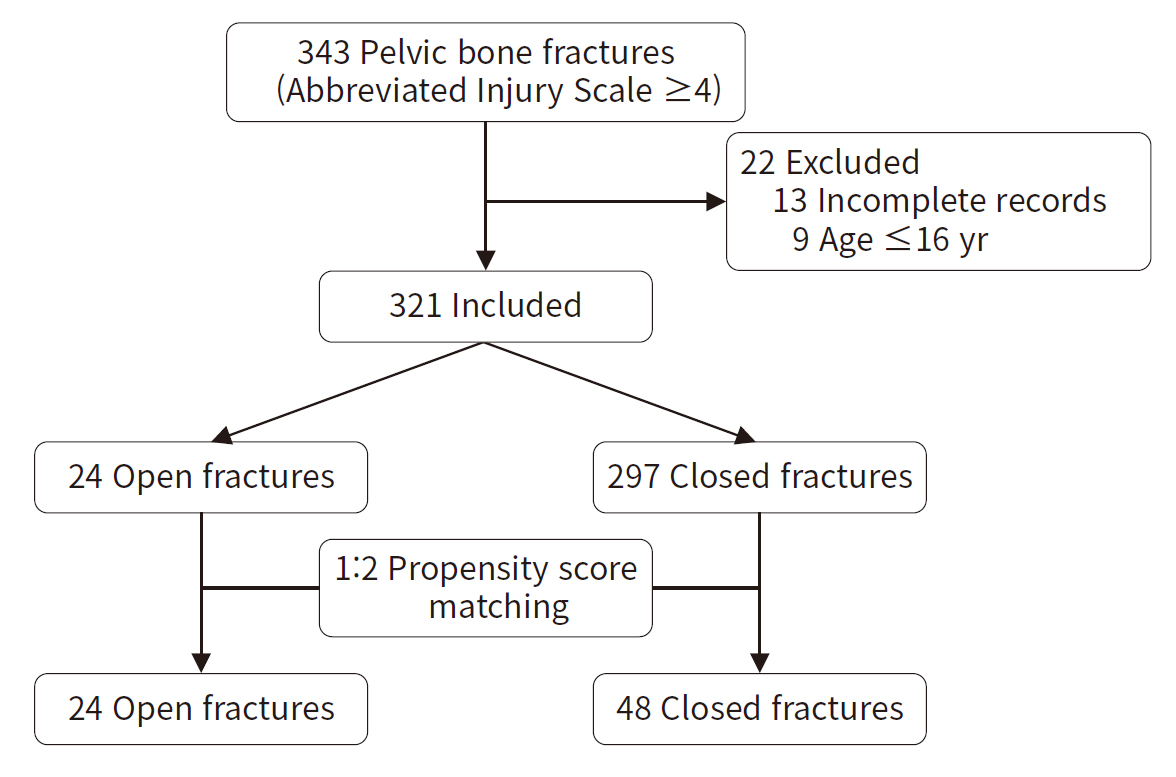
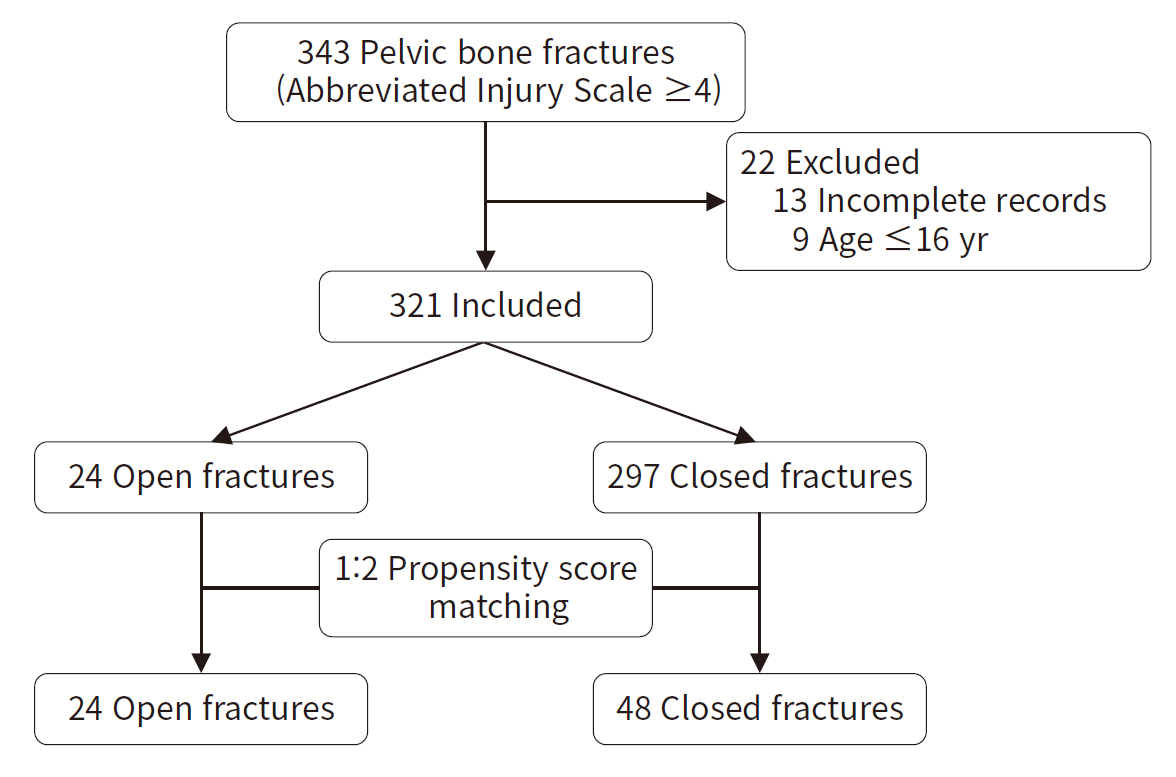
- Patients with severe pelvic bone fractures (pelvic Abbreviated Injury Scale score, ≥4) admitted at a single level I trauma center between 2016 and 2020 were retrospectively analyzed. Patients aged <16 years and those with incomplete medical records were excluded from the study. The patients were divided into open and closed fracture groups, and their demographics, treatment, and clinical outcomes were compared before and after 1:2 propensity score matching.
-
Results
- Of the 321 patients, 24 were in the open fracture group and 297 were in the closed fracture group. The open fracture group had more infections (37.5% vs. 5.7%, P<0.001) and longer stays in the intensive care unit (median 11 days, interquartile range [IQR] 6–30 days vs. median 5 days, IQR 2–13 days; P=0.005), but mortality did not show a statistically significant difference (20.8% vs. 15.5%, P=0.559) before matching. After 1:2 propensity score matching, the infection rate was significantly higher in the open fracture group (37.5% vs. 6.3%, P=0.002), whereas the length of intensive care unit stay (median 11 days, IQR 6–30 days vs. median 8 days, IQR 4–19 days; P=0.312) and mortality (20.8% vs. 27.1%, P=0.564) were not significantly different.
-
Conclusions
- The open pelvic fracture group had more infections than the closed pelvic fracture group, but mortality was not significantly different. Aggressive treatment of pelvic bone fractures is important regardless of the fracture type, and efforts to reduce infection are important in open pelvic bone fractures.
- Background
- Severe pelvic fractures pose a high risk of mortality and morbidity, necessitating rapid treatment with a multidisciplinary approach for effective management [1–3]. While the mortality rate associated with pelvic fractures has improved following the establishment of trauma centers, it remains high, exceeding 40% in cases of closed pelvic bone fractures accompanied by shock [4].
- Open pelvic bone fractures are uncommon, accounting for 2% to 5% of all pelvic bone fractures [5–7]. Open pelvic bone fractures usually involve soft tissue disruption and internal organ damage; hence, they are susceptible to infection. Consequently, open pelvic bone fractures generally have poor outcomes, with a mortality rate that can range widely, from 6% to 58% [7–9]. This rate is notably higher than the mortality of all pelvic bone fractures, which ranges from 5% to 10% [10–12]. However, the inclusion and exclusion criteria are heterogeneous among studies, and severe pelvic bone fractures with shock also have a high mortality rate of approximately 32% to 46% [4,11,13]. The mortality rate of severe pelvic bone fractures is similar to that of open pelvic fractures, and it remains unclear whether an open pelvic fracture is an independent risk factor for mortality.
- Objectives
- Due to the relative rarity of open pelvic bone fractures and the wide-ranging mortality rates reported in the literature, further research is required into whether the fractures type (open or closed) is related to mortality. The aim of this study was to compare the outcomes of open and closed pelvic bone fractures after adjusting for injury severity.
INTRODUCTION
- Ethics statement
- This study was approved by the Institutional Review Board of Ajou University Hospital (No. AJIRB-MED-MDB-21-683). The need for informed consent was waived due to the retrospective nature of the study.
- Study design and patients
- Ajou University Hospital (Suwon, Korea) operates a level I regional trauma center, with >2,500 trauma patients admitted annually. For this study, patients with severe pelvic bone fractures admitted to the center between January 2016 to December 2020 were included. During the study period, a multidisciplinary approach was adopted at our center.
- Patients with severe pelvic bone fractures (Abbreviated Injury Scale [AIS] score updated 2008, ≥4) were included in the study. The exclusion criteria comprised patients under 16 years of age and those for whom a precise Injury Severity Score (ISS) could not be calculated, such as those who were declared dead on arrival or died in the emergency room without a definite diagnosis. The patients were divided into open and closed fracture groups, and their clinical data, treatment procedures, and outcomes were compared. Since open fractures are rare, 1:2 propensity score matching was used to adjust for the severity of injury, and comparisons were made after matching (Fig. 1).
- The primary outcome was the mortality rate for open and closed fractures. The secondary outcomes were the infection rate, length of stay in the intensive care unit, and duration of hospital stay. The operational definition for infection was “sepsis” or “wound infection or surgical site infection” directly related to the fracture; however, superficial infections were not counted.
- Treatment
- Treatment for fractures included, angiography, preperitoneal packing (PPP), or resuscitative endovascular balloon occlusion of the aorta (REBOA) regardless of the fracture type; however, in open fractures additional prophylactic antibiotics (usually first-generation cephalosporin if there was no gastrointestinal organ injury) were administered in the trauma bay. Large open wounds were usually managed using negative pressure wound therapy [14].
- Statistical analysis
- After assessing the data for normality using the Kolmogorov-Smirnov test, continuous variables were compared between the two groups using the Mann-Whitney U-test, and the data were presented as medians with interquartile ranges (IQRs). Categorical variables were compared between the two groups using the chi-square test or the Fisher exact test. Propensity scores were estimated using age, initial and lowest systolic blood pressure, initial heart rate, ISS, lactate level, and pelvic AIS score, which were selected as variables for propensity score matching. After matching, the Mann-Whitney U-test, chi-square test, or Fisher exact test was used. All analyses were performed using IBM SPSS ver. 23.0 (IBM Corp).
METHODS
- Of the 343 patients selected for the study, 321 patients were included in the final analysis. In total, 297 cases involved closed fractures and 24 involved open fractures. The open fractures had significantly higher lactate levels (7.13 mmol/L [IQR, 5.09–10.33 mmol/L] vs. 3.85 mmol/l [IQR, 2.46–6.62 mmol/L], P<0.001) and proportion of AIS score 5 fractures (75.0% vs. 50.8%, P<0.001). The lowest systolic blood pressure in the trauma bay was also significantly lower in the open fracture group (60 mmHg [IQR, 48–79 mmHg] vs. 86 mmHg [IQR, 63–106 mmHg], P=0.001) (Table 1). This group had more transfusions and more frequently underwent aggressive treatment methods (angiography, PPP, and laparotomy); however, the mortality rate was not significantly different (20.8% vs. 15.5%, P=0.559) (Table 2).
- After 1:2 propensity score matching, 24 open fracture patients were compared with 48 patients in the closed fracture group. After matching, patients’ characteristics and treatment methods were not significantly different between the two groups (Table 3).
- After matching, no significant differences were seen in mortality (20.8% vs. 27.1%, P=0.564), length of stay in the intensive care unit (11 days [IQR, 6–30 days] vs. 8 days [IQR, 4–19 days], P=0.312), and duration of hospital stay (49 days [IQR, 20–73 days] vs. 28 days [IQR, 15–58 days], P=0.127). However, the infection rate was significantly higher in the open fracture group (37.5% vs. 6.3%; P=0.002) (Table 4).
RESULTS
- In this study, open pelvic fractures were associated with a higher infection rate, although the mortality rate did not show a statistically different difference after propensity matching. Open pelvic fractures tend to be more lethal than closed fractures. The average mortality rate for generalized pelvic bone fractures is 10% [12]. However, Dente et al. [8] reported a significantly higher mortality rate of 45% for open pelvic fractures, with an average ISS of 30. Another comparative study [15] also reported a 50% mortality rate in open pelvic fractures compared to 10.5% in closed fractures. Despite advancements in treatment methods that have improved survival rates, open pelvic bone fractures still have a high mortality rate. A review of studies conducted between 2005 and 2019 [9] revealed that the average mortality rate for open fractures was 23.7%. Open pelvic fractures are typically the result of a substantial force, such as a severe automobile accident or a high-level fall, which can cause extensive damage to the patient's body [6]. This damage can result in injuries to both internal organs and tissues, including bone fractures. These injuries, which are exposed to the external environment, can lead to complications such as excessive blood loss, infection, and sepsis [16,17]. Consequently, open pelvic fractures should be regarded as a potentially life-threatening condition.
- In the present study, the mortality rate was found to be higher in the open fracture group, although the difference was not statistically significant. Prior studies did not adjust for disease severity, which could potentially influence variations in mortality trends. Given that only severe pelvic bone fractures (AIS score, ≥4) were included in this study, the mortality rate of closed fractures was higher than in previous studies that included all types of pelvic bone fractures. Furthermore, Greenspan et al. [18] reported that the presence of open wounds in open pelvic fractures was assigned a score of 4 in the AIS system, thus categorizing open fractures as more severe injuries. Additionally, after matching, the mortality rate was higher in the closed fracture group, but the difference was not statistically significant. While open fractures are associated with high mortality, it appears that a fracture being open is not an independent risk factor.
- Several management strategies for pelvic fractures have been developed. These include resuscitation treatments such as transfusion and bleeding control, as well as pelvic fracture fixation and the management of soft tissue or associated injuries [9]. In cases of unstable pelvic fractures, invasive procedures like PPP, pelvic angioembolization, and REBOA may be necessary [4]. The same treatment approach has been attempted for open pelvic fractures, with PPP in particular being a plausible method for controlling bleeding and reducing mortality [14]. Hermans et al. [19] reported a mortality rate of only 4% in the open fracture group, which had an average ISS of 31, compared to a 14% mortality rate in the closed fracture group. In the current study, the closed group included fewer transfusions and PPP cases. These were adjusted for using propensity score matching, but the results were not significant.
- An open pelvic fracture is a complex musculoskeletal injury that involves communication between the skin, rectum, or vagina and the wound. This can lead to an increased risk of infection due to contamination from colonized microorganisms present in fecal matter [7,20]. The likelihood of infection also hinges on the location of the open wound, with the pelvis being particularly susceptible to infection [21]. Therefore, careful infection control is necessary, taking into account the severity and location of the open wounds. A study conducted by Wang et al. [13] found that the infection rate was higher in the open pelvic fracture group than in the closed fracture group. They categorized pelvic fractures into three types based on the World Society of Emergency Surgery (WSES) classification system: minor, moderate, and severe. All three types of open pelvic fractures demonstrated statistically significant tendencies toward infection. These findings align with the results of our study, even after propensity score matching.
- Limitations
- This study has several limitations. First, the sample size of open pelvic bone fractures was relatively small, with only 24 cases included. This may have introduced selection bias. However, we attempted to mitigate the impact of this small sample size by employing 1:2 propensity score matching. Second, in this study, pelvic fractures with an AIS score of ≥4 were classified as severe, but in the updated 2008 version, all open pelvic bone fractures are assigned an AIS score of 4. Despite this, all cases included were blunt trauma incidents, and no simple open fractures were identified. We also used propensity score matching to adjust for severity. Third, our definition of infection is narrower than that used in other studies. We opted for a more limited definition to objectively measure and manage the data. It is important to note that apart from pelvic injury infection, sepsis could also arise from other conditions such as pneumonia. Fourth, this study did not consider the chronic effects or long-term outcomes of pelvic bone fractures. Future studies that include regular follow-up, rehabilitation, and quality of life assessments may help to better understand the differences between open and closed pelvic bone fractures.
- Conclusions
- The type of fracture did not influence treatment outcomes or mortality rates after adjusting for injury severity. However, patients with open pelvic fractures exhibited a higher risk of infection compared to those with closed fractures. Therefore, judicious management strategies for infection control may be crucial for patients with open pelvic fractures.
DISCUSSION
-
Author contributions
Conceptualization: BHK; Formal analysis: BHK, DC; Investigation: JY, BHK; Methodology: BHK, DC; Writing–original draft: JY, BHK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION
| Characteristic | Closed fracture (n=297) | Open fracture (n=24) | P-value |
|---|---|---|---|
| Age (yr) | 51 (37–63) | 44 (26–61) | 0.140 |
| Sex | 0.215 | ||
| Male | 198 (66.7) | 13 (54.2) | |
| Female | 99 (33.3) | 11 (45.8) | |
| Admission route | 0.031 | ||
| Direct | 155 (52.2) | 18 (75.0) | |
| Transfer | 142 (47.8) | 6 (25.0) | |
| Initial vital sign | |||
| Systolic BP (mmHg) | 118 (96–140)a) | 110 (75–130) | 0.032 |
| Diastolic BP (mmHg) | 79 (62–95)a) | 78 (53–107) | 0.915 |
| Heart rate (beats/min) | 97 (82–114)b) | 107 (94–128) | 0.009 |
| Respiratory rate (breaths/min) | 22 (18–25)b) | 24 (20–28) | 0.466 |
| Glasgow Coma Scale | 15 (13–15)c) | 14 (9–15) | 0.069 |
| Lowest systolic BP (mmHg) | 86 (63–106)d) | 60 (48–79) | 0.001 |
| Laboratory data | |||
| Lactate (mmol/L) | 3.85 (2.46–6.62)e) | 7.13 (5.09–10.33) | <0.001 |
| Hemoglobin (g/L) | 11.7 (10.1–13.1)b) | 11.9 (10.1–13.1) | 0.955 |
| International normalized ratio | 1.24 (1.10–1.40)f) | 1.36 (1.16–1.65) | 0.055 |
| Injury Severity Score | 36 (29–43) | 42 (26–50) | 0.302 |
| Abbreviated Injury Scale | |||
| Head ≥3 | 77 (25.9) | 4 (16.7) | 0.315 |
| Thorax ≥3 | 184 (62.0) | 15 (62.5) | > 0.999 |
| Abdomen ≥3 | 102 (34.3) | 14 (58.3) | 0.019 |
| Extremity (pelvis) | |||
| 4 | 146 (49.2) | 6 (25.0) | 0.023 |
| 5 | 151 (50.8) | 18 (75.0) | <0.001 |
| Amount transfusion in 24 hr | |||
| Packed red blood cell (U) | 5 (1–13) | 20 (12–31) | <0.001 |
| Fresh frozen plasma (U) | 4 (0–14) | 19 (11–30) | <0.001 |
| Platelet (U) | 0 (0–8) | 9 (2–16) | <0.001 |
- 1. Biffl WL, Smith WR, Moore EE, et al. Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg 2001;233:843–50. ArticlePubMedPMC
- 2. Cullinane DC, Schiller HJ, Zielinski MD, et al. Eastern Association for the Surgery of Trauma practice management guidelines for hemorrhage in pelvic fracture: update and systematic review. J Trauma 2011;71:1850–68. ArticlePubMed
- 3. Magnone S, Coccolini F, Manfredi R, et al. Management of hemodynamically unstable pelvic trauma: results of the first Italian consensus conference (cooperative guidelines of the Italian Society of Surgery, the Italian Association of Hospital Surgeons, the Multi-specialist Italian Society of Young Surgeons, the Italian Society of Emergency Surgery and Trauma, the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care, the Italian Society of Orthopaedics and Traumatology, the Italian Society of Emergency Medicine, the Italian Society of Medical Radiology-Section of Vascular and Interventional Radiology-and the World Society of Emergency Surgery). World J Emerg Surg 2014;9:18. ArticlePubMedPMCPDF
- 4. Jang JY, Bae KS, Chang SW, Jung K, Kim DH, Kang BH. Current management and clinical outcomes for patients with haemorrhagic shock due to pelvic fracture in Korean regional trauma centres: a multi-institutional trial. Injury 2022;53:488–95. ArticlePubMed
- 5. Cannada LK, Taylor RM, Reddix R, et al. The Jones-Powell Classification of open pelvic fractures: a multicenter study evaluating mortality rates. J Trauma Acute Care Surg 2013;74:901–6. PubMed
- 6. Ferrera PC, Hill DA. Good outcomes of open pelvic fractures. Injury 1999;30:187–90. ArticlePubMed
- 7. Grotz MR, Allami MK, Harwood P, Pape HC, Krettek C, Giannoudis PV. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury 2005;36:1–13. ArticlePubMed
- 8. Dente CJ, Feliciano DV, Rozycki GS, et al. The outcome of open pelvic fractures in the modern era. Am J Surg 2005;190:830–5. ArticlePubMed
- 9. Mi M, Kanakaris NK, Wu X, Giannoudis PV. Management and outcomes of open pelvic fractures: an update. Injury 2021;52:2738–45. ArticlePubMed
- 10. Chen HT, Wang YC, Hsieh CC, et al. Trends and predictors of mortality in unstable pelvic ring fracture: a 10-year experience with a multidisciplinary institutional protocol. World J Emerg Surg 2019;14:61. ArticlePubMedPMCPDF
- 11. Costantini TW, Coimbra R, Holcomb JB, et al. Current management of hemorrhage from severe pelvic fractures: results of an American Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care Surg 2016;80:717–25. PubMed
- 12. Holtenius J, Bakhshayesh P, Enocson A. The pelvic fracture: indicator of injury severity or lethal fracture. Injury 2018;49:1568–71. ArticlePubMed
- 13. Wang SH, Fu CY, Bajani F, et al. Accuracy of the WSES classification system for pelvic ring disruptions: an international validation study. World J Emerg Surg 2021;16:54. ArticlePubMedPMCPDF
- 14. Choi D, Cho WT, Song HK, et al. Management strategy for open pelvic fractures: a 11-year single-centre, retrospective observational study. Injury 2023;54:1156–62. ArticlePubMed
- 15. Rothenberger D, Velasco R, Strate R, Fischer RP, Perry JF Jr. Open pelvic fracture: a lethal injury. J Trauma 1978;18:184–7. PubMed
- 16. Watkins RJ, Hsu JM. The road to survival for haemodynamically unstable patients with open pelvic fractures. Front Surg 2020;7:58. ArticlePubMedPMC
- 17. Tseng IC, Chen IJ, Chou YC, Hsu YH, Yu YH. Predictors of acute mortality after open pelvic fracture: experience from 37 patients from a level i trauma center. World J Surg 2020;44:3737–42. ArticlePubMedPMCPDF
- 18. Greenspan L, McLellan BA, Greig H. Abbreviated Injury Scale and Injury Severity Score: a scoring chart. J Trauma 1985;25:60–4. PubMed
- 19. Hermans E, Edwards MJ, Goslings JC, Biert J. Open pelvic fracture: the killing fracture? J Orthop Surg Res 2018;13:83. ArticlePubMedPMCPDF
- 20. Yu YH, Hsu YH, Chou YC, Liu CH, Tseng IC, Chen IJ. Three-year functional outcome after open pelvic fracture treatment: a retrospective case series from a level I trauma center. Eur J Orthop Surg Traumatol 2023;33:937–45. ArticlePubMedPDF
- 21. Faringer PD, Mullins RJ, Feliciano PD, Duwelius PJ, Trunkey DD. Selective fecal diversion in complex open pelvic fractures from blunt trauma. Arch Surg 1994;129:958–64. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite