Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Case Report
Percutaneous screw fixation and external stabilization as definitive surgical intervention for a pelvic ring injury combined with an acetabular fracture in the acute phase of polytrauma in Korea: a case report -
Hohyoung Lee, MD1
 , Myung-Rae Cho, MD2
, Myung-Rae Cho, MD2 , Suk-Kyoon Song, MD2
, Suk-Kyoon Song, MD2 , Euisun Yoon, MD1
, Euisun Yoon, MD1 , Sungho Lee, MD1
, Sungho Lee, MD1
-
Journal of Trauma and Injury 2023;36(3):298-303.
DOI: https://doi.org/10.20408/jti.2023.0002
Published online: July 13, 2023
- 895 Views
- 48 Download
1Department of Orthopedic and Traumatic Surgery, Cheju Halla General Hospital, Jeju, Korea
2Department of Orthopedic Surgery, Daegu Catholic University Medical Center, Daegu, Korea
- Correspondence to Sungho Lee, MD Department of Orthopedic and Traumatic Surgery, Cheju Halla General Hospital, 65 Doryeong-ro, Jeju 63127, Korea Tel: +82-64-740-4277 Email: drsh0330@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Unstable pelvic ring injuries are potentially life-threatening and associated with high mortality and complication rates in polytrauma patients. The most common cause of death in patients with pelvic ring injuries is massive bleeding. With resuscitation, external fixation can be performed as a temporary stabilization procedure for hemostasis in unstable pelvic fractures. Internal fixation following temporary external fixation of the pelvic ring yields superior and more reliable stabilization. However, a time-consuming extended approach to open reduction and internal fixation of the pelvic ring is frequently precluded by an unacceptable physiologic condition and/or concomitant injuries in patients with multiple injuries. Conservative treatment may lead to pelvic ring deformity, which is associated with various functional disabilities such as limb length discrepancy, gait disturbance, and sitting intolerance. Therefore, if the patient is not expected to be suitable for additional surgery due to a poor expected physiologic condition, definitive external fixation in combination with various percutaneous screw fixations to restore the pelvic ring should be considered in the acute phase. Herein, we report a case of unstable pelvic ring injury successfully treated with definitive external fixation and percutaneous screw fixation in the acute phase in a severely injured polytrauma patient.
- Hemodynamically unstable pelvic ring injuries are among the most challenging high-energy traumas in polytrauma patients [1,2]. Hemorrhage is the leading cause of death in patients with pelvic ring injuries, and most bleeding in such injuries originates from the presacral venous plexus and fractured bone [3]. In patients with these injuries, pelvic ring instability can be the primary reason for hemodynamic instability, and hemorrhage control should be a part of resuscitation. Therefore, damage control in the form of temporary mechanical stabilization such as external fixation, pelvic wrapping, or pelvic packing is necessary to control bleeding [4]. Although the contemporary literature includes new concepts such as safe definitive surgery, early appropriate care, and prompt individualized safe management [5], to ensure more stable and reliable fixation, definitive open reduction and internal fixation are usually performed during the “window of opportunity” after resuscitation and restoration of physiologic condition [5]. However, the patient’s physiologic condition may not recover sufficiently to support pelvic fracture surgery within the window of opportunity. Because pelvic fracture surgery with an extended approach is time-consuming and associated with numerous complications, this aggressive surgical impact during the acute phase as part of early total care can induce a “second hit” [5]. In contrast, external fixation and various percutaneous screw fixations are minimally invasive surgical procedures that minimize secondary complications. We report a case of a hemodynamically unstable polytrauma patient for whom future definitive surgery was expected to be precluded due to an unacceptable physiologic condition. The patient was successfully treated with definitive external fixation and percutaneous screw fixations in the acute phase.
INTRODUCTION
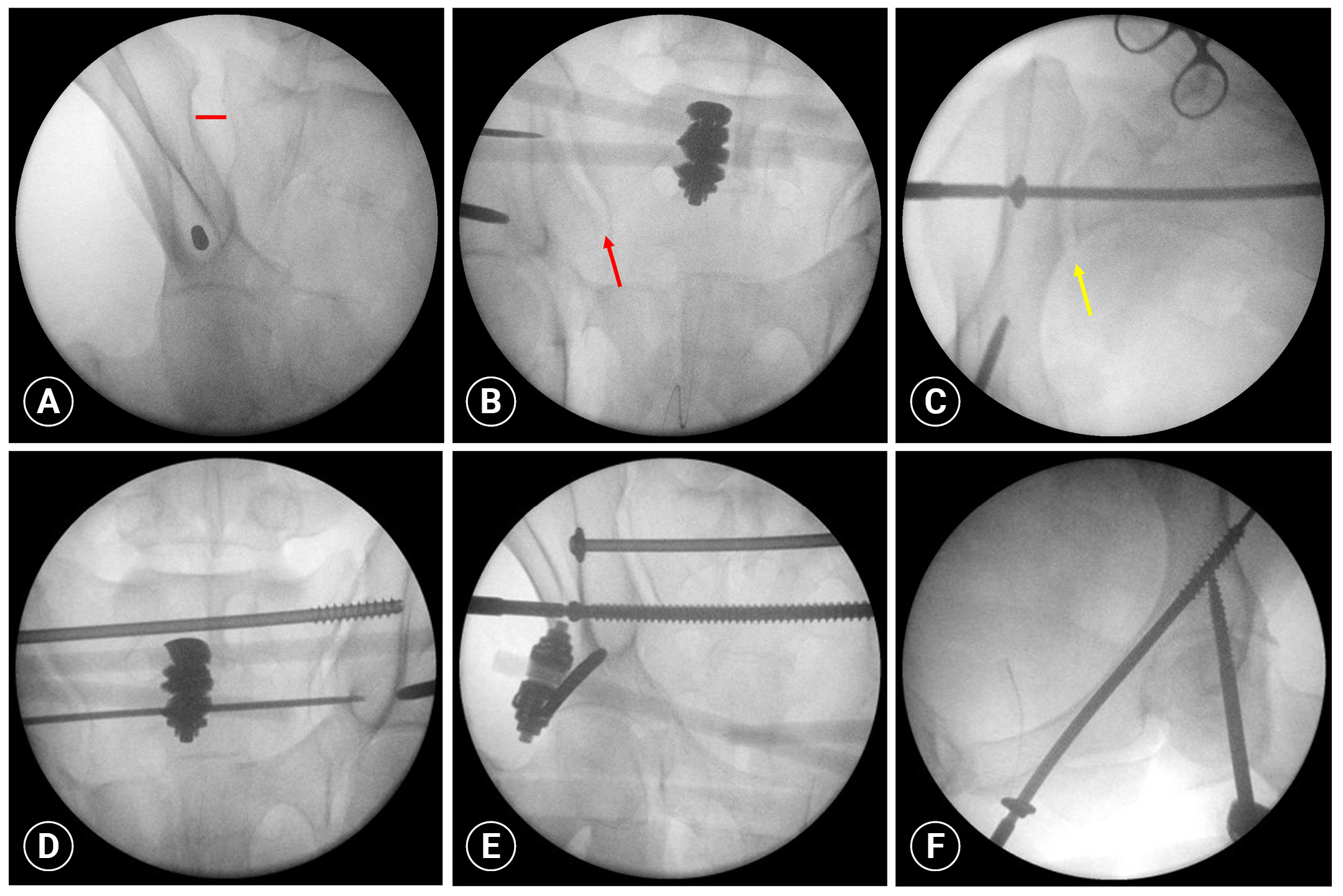
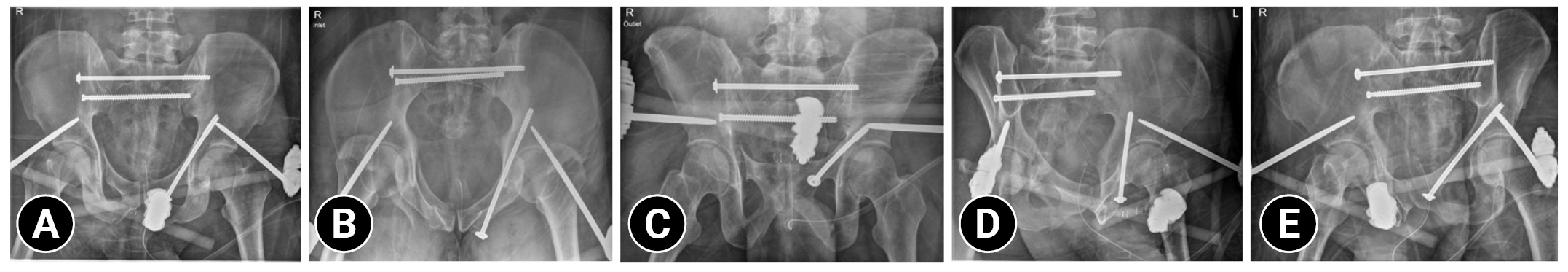
- An American Society of Anesthesiologists (ASA) physical status class I, healthy 33-year-old male patient was transferred to a level I trauma center after being struck by an excavator bucket at a construction site. The patient had no significant past medical history. On arrival, the patient was confused, and his vital signs included an unstable blood pressure of 95/44 mmHg, a pulse rate of 144 beats/min, and a respiration rate of 40 breaths/min. Given the patient’s unstable condition, a massive transfusion protocol was initiated with the transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio. Radiography and computed tomography demonstrated an unstable pelvic ring injury consisting of right sacroiliac joint dislocation, a non-displaced transverse fracture of the left acetabulum, right pubic rami fractures, and an anterior wall fracture of the right acetabulum (Fig. 1). The patient also had traumatic hemopneumothorax with multiple rib fractures, subarachnoid hemorrhage with depressed skull fracture of the temporal bone, and facial maxillary bone fracture. The patient was determined to have an Injury Severity Score of 34, indicating polytrauma. Emergent closed thoracostomy with chest tube insertion, cranioplasty with hematoma evacuation, and external fixation along with percutaneous screw fixation were performed. Because the patient’s condition was life-threatening, we expected future definitive internal fixation to be precluded by an unacceptable physiologic condition. Therefore, we opted to perform minimally invasive definitive fixation in the acute phase if possible. We planned external pelvic fixation with percutaneous iliosacral (IS) screw fixation for the pelvic ring and percutaneous screw fixation for the left acetabular fracture. After application of a supra-acetabular external fixator using 6-mm–diameter Schanz pins, percutaneous IS screw fixations were performed to the S1 body using a 7.3-mm partially threaded cannulated screw with a washer in compression mode and to the S2 body using a 7.3-mm fully threaded cannulated screw in position mode. Both the S1 and S2 screws had purchase with the contralateral sacroiliac joint to ensure stability. During this procedure, an external fixator frame was utilized to reduce the posterior pelvic ring by joystick maneuver and was subsequently left in place. Percutaneous in situ fixation of the left acetabulum was performed using a 7.3-mm cannulated screw. This screw was introduced just inferior to the pubic tubercle and was passed through the intramedullary corridor of the superior pubic ramus to the posterior column to achieve bicolumnar fixation of the acetabulum (Figs. 2, 3). The patient was subsequently admitted to the intensive care unit for ongoing resuscitation. After spending 16 days in the intensive care unit, the patient was transferred to the general ward. During this critical period for lifesaving, the patient’s physiologic condition, including coagulopathy and acid-base imbalance with lactate level, had not recovered sufficiently for additional surgery [5]. On serial follow-up, radiographs indicated that reduction of the pelvis and acetabulum were well maintained, and no further displacement was observed. We decided to keep an external fixator as definitive stabilization for the anterior pelvic ring and to use adjunct stabilization with IS screw fixations for the posterior ring. However, we removed the external fixator 24 days after surgery due to pin site infection. Because no residual fluoroscopic displacement was observed after removal of the external fixator, we performed no further surgery (Fig. 4). Despite the lack of scientific evidence, a pelvic binder was applied to prevent secondary displacement after removal of the external fixator. The patient’s mental and general condition completely recovered by approximately 4 weeks after the injury. The patient was then allowed to sit and move by wheelchair as tolerated. From 6 weeks postoperatively, the patient was allowed protected weight-bearing and could transition to full weight-bearing as tolerated. Eight weeks after surgery, the patient was allowed to walk independently. At 6-month follow-up, radiographs demonstrated complete healing and favorable alignment of the pelvic ring, and the patient returned to full activity (Fig. 5).
- Ethics statement
- This study was reviewed and approved by the Institutional Review Board of Cheju Halla General Hospital (No. 2023-L05-01). The requirement for informed consent was waived, as all data were de-identified to protect patient’s right to privacy.
CASE REPORT
- Unstable pelvic ring injuries require surgical reduction and fixation to restore the pelvic anatomy and allow the patient to regain physical function [6]. However, because unstable pelvic ring injuries are life-threatening and associated with high mortality and complication rates, initial assessment and management to resuscitate is a priority [1,2]. The timing of major fracture care in polytrauma patients has been updated. The current understanding avoids the use of a “window of opportunity,” in which surgery is avoided on days 2 to 4 after injury [7]. Instead, the contemporary literature includes new concepts such as safe definitive surgery, early appropriate care, and prompt individualized safe management [5]. However, because the present patient’s physiologic condition did not recover for a long period, these new concepts were inappropriate. We decided to apply a single-bar and single-pin supra-acetabular pelvic external fixator for damage control in the acute phase. External fixation of the pelvis is associated with hemostasis due to reduction of pelvic volume, hematoma formation by the tamponade effect, and fracture fragment stabilization [8]. However, posterior stabilization cannot be achieved using an anteriorly placed external fixator. The most important step in ensuring pelvic ring stability is the reduction and fixation of the posterior sacroiliac complex [6]. A C-clamp is used to stabilize the posterior pelvic ring to control hemorrhage, particularly in vertical shear injury patterns [1,2]. Some trauma surgeons advocate the use of an anti-shock IS screw or rescue screw instead of posterior stabilization with a C-clamp [9]. In the present case, posterior ring stabilization was achieved with percutaneous IS screws to the S1 and S2 bodies. We performed percutaneous IS screw fixation to the S1 body using a 7.3-mm partially threaded cannulated screw with a washer in compression mode and to the S2 body using a 7.3-mm fully threaded cannulated screw in position mode. During this procedure, an external fixator frame was utilized to reduce the posterior pelvic ring by the joystick maneuver and was subsequently left in place. Because we expected additional surgery to be precluded due to a poor physiologic condition, we endeavored in each stage of procedures to attain anatomical reduction and simple stabilization with minimally invasive procedures during damage control surgery in the acute phase. In this case, the functions of the external fixator included not only damage control to minimize bleeding, but also definitive fixation to the anterior pelvic ring and adjunctive fixation with IS screws to the posterior pelvic ring. Several authors have reported high complication rates and poor outcomes when a pelvic external fixator is used as definitive fixation of the pelvic ring [10]. Another study indicated that pelvic external fixators have insufficient biomechanical stability and mixed outcomes after surgery [11]. In contrast, the contemporary orthopedic trauma literature suggests that a pelvic external fixator can be used for the definitive fixation of a pelvic ring injury. Tosounidis et al. [8] reported that the application of a pelvic external fixator as definitive fixation in specific polytrauma settings is a safe and efficient method for pelvic ring stabilization. In that study, they stated that the rates of complications such as infection, aseptic loosening, and neurogenic complications were low, while the overall outcomes were good. Therefore, their study showed that in polytrauma patients, external fixation can be a useful alternative to internal fixation, yielding acceptable clinical outcomes with low complication rates. In the present case, a minimally displaced transverse fracture of the left acetabulum was also stabilized by percutaneous screw fixation without reduction. A guide pin was introduced just inferior to the pubic tubercle. Then, it was passed through the intramedullary corridor of the superior pubic ramus to the posterior column to achieve bicolumnar fixation of the acetabulum. Percutaneous fixation of acetabular fractures with or without closed reduction has been proposed to prevent potential further displacement of simple fractures with minimal displacement [12]. Based on the concept of the roof arc angle, Olson and Matta [13] concluded that in fractures with roof arc measurements greater than 45° on anteroposterior (medial roof arc), iliac oblique (posterior roof arc), and obturator oblique (anterior roof arc) radiographs, sufficient weight-bearing articular surface remained intact for nonoperative treatment to be considered when the femoral head remained congruent with the superior acetabulum. In the present case, the patient’s measured roof arc angles on anteroposterior, iliac oblique, and obturator oblique radiographs were 51°, 68°, and 65°, respectively. The femoral head remained congruent with the superior acetabulum. In addition, the patient’s physiologic condition was too poor for additional surgical procedures, so we decided not to perform surgery for the anterior wall fracture of the right acetabulum to avoid surgical impact that could induce a “second hit.” The optimal timing of removal of the external fixator also raised issues. Typically, union of the pelvic ring may be achieved after 8 to 12 weeks [14]. Problematically, however, due to the lack of an indicator of ligamentous healing, the timing of removal in this case was based on a combination of factors such as surgeon clinical judgment, pin site concern, and concomitant injury. Despite every effort to maintain the external fixator as long as possible, it had to be removed 24 days after surgery due to pin site infection. Because the external fixator was used for adjunctive stabilization of the posterior ring, no residual displacement was observed after the removal of external fixation. Although Hoyt et al. [14] reported that the timing of removal and their definition of clinical union were based on predetermined removal timing and examination under anesthesia instead of guidance by radiographic or functional milestones, we did not perform an examination under anesthesia due to fear of iatrogenic further displacement. Despite the lack of scientific evidence, a pelvic binder was applied to prevent secondary displacement after the removal of the external fixator.
- A limitation of this case report is that the follow-up duration was only 9 months. This may be insufficient to evaluate all complications, including posttraumatic degenerative changes in bones and joints. Furthermore, pelvic ring injuries have various fracture and dislocation patterns, and multiple factors may affect the outcomes. Therefore, prudent decision-making in the acute critical phase is essential. Nevertheless, when additional definitive surgery is precluded by unacceptable physiologic conditions in hemodynamically unstable pelvic ring injuries, minimally invasive definitive stabilization in the acute phase can be a treatment option.
DISCUSSION
-
Author contributions
Conceptualization: HL, SL; Data curation: EY; Formal analysis: SKS; Methodology: HL, SL; Project administration: MRC, SL; Visualization: EY; Writing-original draft: HL, SL; Writing-review & editing: MRC, SKS, SL. All authors read and approved the final manuscript
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
-
Data sharing statement
Not applicable.
ARTICLE INFORMATION



- 1. Tosounidis TI, Giannoudis PV. Pelvic fractures presenting with haemodynamic instability: treatment options and outcomes. Surgeon 2013;11:344–51. ArticlePubMed
- 2. Ertel W, Keel M, Eid K, Platz A, Trentz O. Control of severe hemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. J Orthop Trauma 2001;15:468–74. ArticlePubMed
- 3. Balogh Z, Caldwell E, Heetveld M, et al. Institutional practice guidelines on management of pelvic fracture-related hemodynamic instability: do they make a difference? J Trauma 2005;58:778–82. ArticlePubMed
- 4. Manson T, O’Toole RV, Whitney A, Duggan B, Sciadini M, Nascone J. Young-Burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? J Orthop Trauma 2010;24:603–9. ArticlePubMed
- 5. Pape HC, Halvachizadeh S, Leenen L, Velmahos GD, Buckley R, Giannoudis PV. Timing of major fracture care in polytrauma patients: an update on principles, parameters and strategies for 2020. Injury 2019;50:1656–70. ArticlePubMed
- 6. Pohlemann T, Gansslen A, Schellwald O, Culemann U, Tscherne H. Outcome after pelvic ring injuries. Injury 1996;27 Suppl 2:B31–8. ArticlePubMed
- 7. Pape HC, Pfeifer R. Safe definitive orthopaedic surgery (SDS): repeated assessment for tapered application of early definitive care and damage control?: an inclusive view of recent advances in polytrauma management. Injury 2015;46:1–3. ArticlePubMed
- 8. Tosounidis TH, Sheikh HQ, Kanakaris NK, Giannoudis PV. The use of external fixators in the definitive stabilisation of the pelvis in polytrauma patients: safety, efficacy and clinical outcomes. Injury 2017;48:1139–46. ArticlePubMed
- 9. Gardner MJ, Routt ML Jr. Transiliac-transsacral screws for posterior pelvic stabilization. J Orthop Trauma 2011;25:378–84. ArticlePubMed
- 10. Dickson KF, Matta JM. Skeletal deformity after anterior external fixation of the pelvis. J Orthop Trauma 2009;23:327–32. ArticlePubMed
- 11. Papathanasopoulos A, Tzioupis C, Giannoudis VP, Roberts C, Giannoudis PV. Biomechanical aspects of pelvic ring reconstruction techniques: evidence today. Injury 2010;41:1220–7. ArticlePubMed
- 12. Parker PJ, Copeland C. Percutaneous fluoroscopic screw fixation of acetabular fractures. Injury 1997;28:597–600. ArticlePubMed
- 13. Olson SA, Matta JM. The computerized tomography subchondral arc: a new method of assessing acetabular articular continuity after fracture (a preliminary report). J Orthop Trauma 1993;7:402–13. ArticlePubMed
- 14. Hoyt BW, Lundy AE, Purcell RL, Harrington CJ, Gordon WT. Definitive external fixation for anterior stabilization of combat-related pelvic ring injuries, with or without sacroiliac fixation. Clin Orthop Relat Res 2020;478:779–89. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite






