Articles
- Page Path
- HOME > J Trauma Inj > Volume 34(2); 2021 > Article
-
Original Article
Indications for Laparotomy in Patients with Abdominal Penetrating Injuries Presenting with Ambiguous Computed Tomography Findings - Eun Ji Choi, M.D.1, Sanghee Choi, M.D.1,2, Byung Hee Kang, M.D.1
-
Journal of Trauma and Injury 2021;34(2):112-118.
DOI: https://doi.org/10.20408/jti.2020.0058
Published online: June 8, 2021
- 2,727 Views
- 88 Download
1Department of Surgery, Ajou University School of Medicine, Suwon, Korea
2Department of Radiology, Ajou University School of Medicine, Suwon, Korea
- Correspondence to Byung Hee Kang, M.D. Department of Surgery, Ajou University School of Medicine, 164 World cup-ro, Yeongtong-gu, Suwon 16499, Korea Tel: +82-31-219-7764 Fax: +82-31-219-7781 E-mail: kbhname@ajou.ac.kr
• Received: October 12, 2020 • Revised: December 7, 2020 • Accepted: December 8, 2020
Copyright © 2021 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Negative laparotomy in patients with abdominal penetrating injuries (APIs) is associated with deleterious outcomes and unnecessary expense; however, the indications for laparotomy in hemodynamically stable patients with ambiguous computed tomography (CT) findings remain unclear. This study aimed to identify the factors associated with negative laparotomy. findings
-
Methods
- Data of patients who underwent laparotomy for APIs between 2011 and 2019 were retrospectively reviewed. Patients who presented with definite indications for laparotomy were excluded. The patients were dichotomized into negative and positive laparotomy groups, and the baseline characteristics, laboratory test results, and CT findings were compared between the groups.
-
Results
- Of 55 patients with ambiguous CT findings, 38 and 17 patients were assigned to the negative and positive laparotomy groups, respectively. There was no significant difference between the groups with respect to the baseline characteristics or the nature of the ambiguous CT findings. However, the laboratory test results showed that there was a difference in the percentage of neutrophils between the groups (negative: 55.6% [range 47.4–66.1%] vs. positive: 79.8% [range 77.6–88.2%], p<0.001), although the total white blood cell count was not significantly different. The mean duration of hospital stay for the negative laparotomy group was 13.1 days, and seven patients (18.4%) experienced complications.
-
Conclusions
- Diagnostic factors definitively indicative of laparotomy were not identified, although the percentage of neutrophils might be helpful. However, routine laparotomy in patients with peritoneal injuries could result in instances of negative laparotomy.
- Patients with penetrating injuries are less commonly encountered than those with blunt injuries in the Republic of Korea. As the use of firearms is not allowed in the Republic of Korea, stab wounds account for most penetrating injuries [1]. In addition, the suicide rate is high in the Republic of Korea; thus, cases of self-inflicted abdominal penetrating injuries (APIs) are encountered [2].
- Unstable vital signs or diffuse abdominal pain is an absolute indication for laparotomy in patients with APIs [3,4]. A foreign body in the abdominal cavity is also an acceptable indication for laparotomy if the foreign body is removable [5]. However, it is difficult to select laparotomy for hemodynamically stable patients with ambiguous symptoms or unreliable physical examination findings due to brain injury, alcohol intoxication, or need for sedation. Although many diagnostic tools have been developed, they are still inadequate with respect to decision-making for laparotomy [6,7]. Moreover, diagnostic peritoneal lavage and focused assessment with sonography for trauma (FAST) are not routinely performed by physicians in Korea, because computed tomography (CT) can be easily performed at a low cost for diagnostic evaluation. The positive predictive value of CT for anterior stab wounds has been reported to be 47–97%; therefore, injuries are still missed, and non-therapeutic laparotomy is commonly performed [8-11].
- If the peritoneum is not opened on local wound exploration (LWE), laparotomy is not required [12]. However, decision-making regarding whether to perform laparotomy is also difficult if the peritoneum is opened, as observed during LWE or CT. Active bleeding of the abdominal muscle may be an indication for surgery; however, the extension of the incision is another concern. Although an additional incision is not required for peritoneal or muscle repair, it is required for exploring a bowel injury. Unnecessary laparotomy is associated with complications, unnecessary expense, longer hospital stay, and even mortality [13]. However, a missed organ injury is an adverse event for patients and poses a concern for physicians. Hence, we reviewed patients with stab wounds with ambiguous CT findings who underwent laparotomy and explored possible factors that may be associated with negative laparotomy findings.
INTRODUCTION
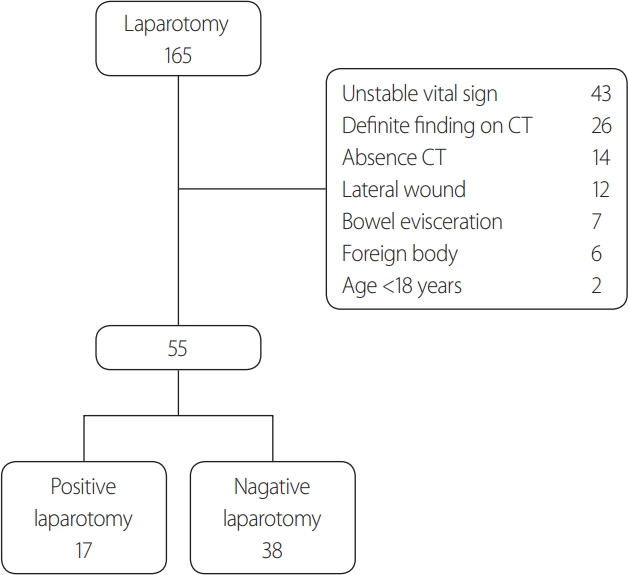
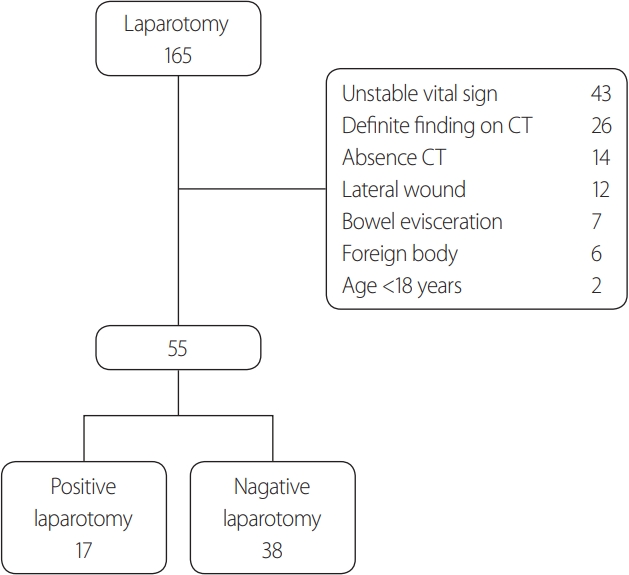
- Patients who underwent laparotomy owing to APIs at Ajou University Hospital trauma center between January 2011 and December 2019 were included. Patients with a lack of CT data or with definite indications for surgery, such as unstable vital signs, bowel evisceration, a foreign body in the abdominal cavity, and identified organ injury on CT were excluded. Patients with stab wounds on the sides or on the back that were not potentially related to bowel injuries were also excluded.
- At Ajou University Hospital trauma center, laparotomy was performed if peritoneal penetration was confirmed on either LWE or CT. If peritoneal penetration was not confirmed on LWE, abdominal CT was performed for a further evaluation. However, when abdominal CT was conducted before a trauma surgeon examined the patient, LWE was not mandatorily performed. FAST was not performed in all patients because it was not available in the early study period.
- Ambiguous CT findings were defined as the absence of definite intra-abdominal organ injuries or intraperitoneal bleeding observed on CT as confirmed by a radiologist. Minimal hemoperitoneum and minimal pneumoperitoneum observed on CT were considered ambiguous CT findings because these findings may develop due to abdominal wounds. A suspected bowel injury was also considered to be an ambiguous finding because this finding was not indicative of a definite diagnosis. CT findings were classified as minimal hemoperitoneum, pneumoperitoneum, and possible bowel injury findings (findings suspicious for an injury, such as bowel wall thickening or infiltration) after consulting a radiologist. Negative laparotomy was defined as the absence of hollow viscus injuries or the observation of minimal injuries not requiring surgical repair.
- Patients were divided into negative laparotomy and positive laparotomy groups, and the general characteristics and clinical findings were compared between the groups. The chi-square test or Fisher exact test was used for categorical variables, and the Student t-test or Mann-Whitney test was used for continuous variables after normality testing. Statistical analysis was performed using SPSS version 23 (IBM Corp., Armonk, NY, USA).
METHODS
- Patients’ characteristics
- Initially, 165 patients were included in this study, and the data of 55 patients were reviewed after applying the exclusion criteria. Of these patients, 38 and 17 were assigned to the negative and positive laparotomy groups, respectively (Fig. 1). All patients had experienced a penetrating injury by a knife (Fig. 2). The general characteristics were not significantly different between the two groups (Table 1).
- Diagnostic test for laparotomy
- The numerical pain scale scores and FAST findings were not significantly different between the two groups. With respect to laboratory test results, a significant difference was observed in the percentage of neutrophils (negative: 55.6% [range 47.4–66.1%] vs. positive: 79.8% [range 77.6–88.2%], p<0.001), but other laboratory test results including the white blood cell count did not show significant differences (Table 2). Among the stable patients, 81 patients underwent CT and 26 patients presented with definite injures; however, 28 patients presented with ambiguous findings and 27 patients presented with negative findings (no definite intra-abdominal injuries). The analysis of the CT findings revealed no significant difference between the negative and positive laparotomy groups. Seven patients required surgical treatment, including those with negative CT findings (Table 3).
- Clinical outcomes of negative laparotomy
- Mortality was not noted in this study. The mean duration of hospital stay was 13.1 days, as 25 patients required psychiatric treatment for previous suicide attempts. In addition, the hospital stay was prolonged owing to concomitant injuries, such as wrist lacerations or neck injuries, although negative laparotomy findings were obtained. Seven patients experienced complications after negative laparotomy, and two patients required surgery because of wound problems (Table 4).
RESULTS
- Routine laparotomy for API is no more recommeded for hemodynamically stable patients, since negative laparotomy is associated with adverse outcomes and unnecessary expense. Thus, additional evaluation procedures, such as CT, are recommended with respect to decision-making regarding the performance of laparotomy [3,4]. A meta-analysis reported the sensitivity, specificity, negative predictive value, positive predictive value, and accuracy of CT for indicating laparotomy was high at 94.90%, 95.38%, 98.62%, 84.51%, and 94.70%, respectively, in hemodynamically stable patients with APIs [14]. However, lower values were reported for CT with respect to the detection of bowel injuries. Jawad et al. [15] reported that the sensitivity, specificity, negative predictive value, and positive predictive value were 88%, 72%, 80%, and 82%, respectively. For better diagnosis, CT tractography may be performed for detecting peritoneal penetration; however, bowel injuries could not be detected with CT tractography [11]. Unlike blunt injuries, APIs may lead to the development of hemoperitoneum or pneumoperitoneum; thus, the CT findings may appear more ambiguous. To date, there is no definitive recommendation for the evaluation procedure that should be performed if the CT findings are ambiguous. The sensitivity and specificity of sonography or diagnostic peritoneal lavage are lower than those of CT. Presently, a definitive diagnostic modality for detecting intraabdominal injuries is not available, as was also noted in this study.
- Although laboratory test is not included as an indication for laparotomy in guidelines, they might be helpful when deciding whether to perform laparotomy. No significant differences were found between the positive and negative laparotomy groups in terms of blood cell count, lactate, base excess, amylase, and total bilirubin levels. However, the percentage of neutrophils was significantly different between the two groups. Increased levels of immature neutrophils in the bloodstream, also known as a “left shift”, are associated with inflammatory conditions, and this finding can be used to predict infectious conditions such as bowel perforation in patients with APIs. However, the neutrophil percentage alone cannot be a perfect indicator for laparotomy. Recently, the delta neutrophil index (DNI) has been utilized to predict the prognosis of trauma patients [16]. Although blood cell analyzers at Ajou University Hospital trauma center do not provide the DNI, other inflammatory markers such as procalcitonin and C-reactive protein might be helpful when deciding whether to perform laparotomy.
- In the current study, 38 patients underwent unnecessary laparotomy, with a complication rate of 18.4%. Two patients required surgical repair for wounds, while others recovered after receiving conservative care. The duration of hospital stay was 13.1 days; however, this was not necessarily because of the development of complications. The patients who had attempted suicide needed psychiatric admission, and the hospital stay was prolonged for patients with other concomitant injuries, such as wrist lacerations and neck injuries. Demetriades et al. [17] reported that selective non-operative management of APIs was associated with a high success rate and relatively low complication rates, even for patients with high-grade injuries. Laparoscopy may be another option. Hajibandeh et al. [18] reported that the sensitivity of laparoscopy for detecting APIs was 100%, and unnecessary laparotomy was avoided in 45.6% of the patients. Moreover, the patients in whom laparoscopy was performed had a lower complication rates and a shorter hospital stay. In the current study, laparoscopy was performed in three patients, and no patients showed intra-abdominal injuries. Unnecessary laparotomy was avoided, and these patients were discharged without any complications.
- Vital signs and physical examination findings have been considered definite indications for laparotomy for many years [19]. In patients with unreliable physical examination findings due to brain injury, alcohol intoxication, or need for sedation, serial physical examinations could be helpful in deciding whether to perform laparotomy. Peev et al. [20] demonstrated that delayed laparotomy after serial physical examinations in patients with ambiguous symptoms did not increase the complication rate. van Haarst et al. [21] also demonstrated that serial physical examinations decreased the negative laparotomy rate to zero. In addition, delayed laparotomy did not increase mortality and morbidity. Despite advancements in laboratory tests and imaging procedures, bedside examinations are markedly more important with respect to decision-making regarding laparotomy. Additional studies are required to identify objective tests that could be used; however, it seems that the surgeon’s diagnostic skill is likely to remain important in the future.
- There are several limitations of this study. First, the number of patients was too small for the study to have sufficient statistical power. Second, owing to the retrospective nature of the study, the records of physical examinations, which may contain strong indications for laparotomy, were not available for all patients. Third, negative laparotomy did not always correspond to unnecessary surgery. Some patients experienced massive bleeding from the inferior epigastric artery and required surgery, although they had no injuries in the intraperitoneal organs. However, unnecessary incisions may still be created during exploratory laparotomy.
- In conclusion, routine laparotomy in patients with peritoneal violation can lead to instances of negative laparotomy and unnecessary complications. However, no definite indication for laparotomy was found in hemodynamically stable patients with ambiguous CT findings. In these patients, a laparosopic approach or serial physical examinations could be utilized. In addition, the percentage of neturophils might be helpful when deciding whether to perform laparotomy.
DISCUSSION
Table 1.General characteristics of the patients
Table 2.Diagnostic findings indicative of laparotomy
| Negative laparotomy group (n=38) | Positive laparotomy group (n=17) | p-value | |
|---|---|---|---|
| White blood count | 8.9 (7.3–12.0) | 11.5 (9.7–12.4) | 0.099 |
| Neutrophil percent | 55.6 (47.4–66.1) | 79.8 (77.6–88.2) | <0.001 |
| Lactate | 2.6 (1.7–3.5) | 2.0 (1.2–3.6) | 0.384 |
| Base excess | -4.1 (-2.5 to -5.6) | -3.8 (-2.1 to -5.3) | 0.585 |
| Amylase | 53 (36–63) | 45 (36–60) | 0.291 |
| Total bilirubin | 0.6 (0.4–1.0) | 0.5 (0.4–0.7) | 0.396 |
| Numeric rating scale for pain | 3 (2–5) | 3 (3–4) | 0.642 |
| FAST (positive/performed) | 5/28 (17.9%) | 4/9 (24.3%) | 0.178a |
Table 3.Computed tomography findings
| Negative laparotomy group (n=38) | Positive laparotomy group (n=17) | p-value | |
|---|---|---|---|
| Minimal hemoperitoneum | 16 (42.1) | 8 (47.1) | 0.732 |
| Minimal pneumoperitoneum | 2 (5.4) | 4 (23.5) | 0.066a |
| Possible organ injury | 8 (21.6) | 5 (38.5) | 0.733a |
| No definite intraperitoneal injury | 20 (52.6) | 7 (41.2) | 0.432 |
Table 4.Outcomes of the negative laparotomy group
| Duration of hospital stay (days) | 13.1±2.0 |
|---|---|
| Complications | |
| Wound problems | 3 (7.9) |
| Ileus | 2 (5.2) |
| Vocal cord palsy | 1 (2.6) |
| Catheter-related infection | 1 (2.6) |
- 1. Byun CS, Park IH, Oh JH, Bae KS, Lee KH, Lee E. Epidemiology of trauma patients and analysis of 268 mortality cases: trends of a single center in Korea. Yonsei Med J 2015;56:220–6. ArticlePubMed
- 2. Woo S, Lee SW, Lee K, Seo WS, Lee J, Kim HC, et al. Characteristics of high-intent suicide attempters admitted to emergency departments. J Korean Med Sci 2018;33:e259. ArticlePubMedPMC
- 3. Biffl WL, Leppaniemi A. Management guidelines for penetrating abdominal trauma. World J Surg 2015;39:1373–80. ArticlePubMedPDF
- 4. Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 2010;68:721–33. ArticlePubMed
- 5. Dienstknecht T, Horst K, Sellei RM, Berner A, Nerlich M, Hardcastle TC. Indications for bullet removal: overview of the literature, and clinical practice guidelines for European trauma surgeons. Eur J Trauma Emerg Surg 2012;38:89–93. ArticlePubMedPDF
- 6. Dreizin D, Munera F. Multidetector CT for penetrating torso trauma: state of the art. Radiology 2015;277:338–55. ArticlePubMed
- 7. Quinn AC, Sinert R. What is the utility of the Focused Assessment with Sonography in Trauma (FAST) exam in penetrating torso trauma? Injury 2011;42:482–7. ArticlePubMed
- 8. Bansal V, Reid CM, Fortlage D, Lee J, Kobayashi L, Doucet J, et al. Determining injuries from posterior and flank stab wounds using computed tomography tractography. Am Surg 2014;80:403–7. ArticlePubMed
- 9. Berardoni NE, Kopelman TR, O'Neill PJ, August DL, Vail SJ, Pieri PG, et al. Use of computed tomography in the initial evaluation of anterior abdominal stab wounds. Am J Surg 2011;202:690–6. ArticlePubMed
- 10. Bruckner BA, Norman M, Scott BG. CT Tractogram: technique for demonstrating tangential bullet trajectories. J Trauma 2006;60:1362–3. ArticlePubMed
- 11. Uzunosmanoğlu H, Çorbacıoğlu ŞK, Çevik Y, Akıncı E, Hacıfazlıoğlu Ç, Yavuz A, et al. What is the diagnostic value of computed tomography tractography in patients with abdominal stab wounds? Eur J Trauma Emerg Surg 2017;43:273–7. ArticlePubMedPDF
- 12. Cothren CC, Moore EE, Warren FA, Kashuk JL, Biffl WL, Johnson JL. Local wound exploration remains a valuable triage tool for the evaluation of anterior abdominal stab wounds. Am J Surg 2009;198:223–6. ArticlePubMed
- 13. Schnüriger B, Lam L, Inaba K, Kobayashi L, Barbarino R, Demetriades D. Negative laparotomy in trauma: are we getting better? Am Surg 2012;78:1219–23. ArticlePubMed
- 14. Goodman CS, Hur JY, Adajar MA, Coulam CH. How well does CT predict the need for laparotomy in hemodynamically stable patients with penetrating abdominal injury? A review and meta-analysis. AJR Am J Roentgenol 2009;193:432–7. ArticlePubMed
- 15. Jawad H, Raptis C, Mintz A, Schuerer D, Mellnick V. Single-contrast CT for detecting bowel injuries in penetrating abdominopelvic trauma. AJR Am J Roentgenol 2018;210:761–5. ArticlePubMed
- 16. Bang HJ, Kim K, Shim H, Kim S, Jung PY, Choi YU, et al. Delta neutrophil index for predicting mortality in trauma patients who underwent emergent abdominal surgery: a case controlled study. PLoS One 2020;15:e0230149. ArticlePubMedPMC
- 17. Demetriades D, Hadjizacharia P, Constantinou C, Brown C, Inaba K, Rhee P, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg 2006;244:620–8. ArticlePubMedPMC
- 18. Hajibandeh S, Hajibandeh S, Gumber AO, Wong CS. Laparoscopy versus laparotomy for the management of penetrating abdominal trauma: a systematic review and meta-analysis. Int J Surg 2016;34:127–36. ArticlePubMed
- 19. Demetriades D, Rabinowitz B. Indications for operation in abdominal stab wounds. A prospective study of 651 patients. Ann Surg 1987;205:129–32. ArticlePubMedPMC
- 20. Peev MP, Chang Y, King DR, Yeh DD, Kaafarani H, Fagenholz PJ, et al. Delayed laparotomy after selective non-operative management of penetrating abdominal injuries. World J Surg 2015;39:380–6. ArticlePubMedPDF
- 21. van Haarst EP, van Bezooijen BP, Coene PP, Luitse JS. The efficacy of serial physical examination in penetrating abdominal trauma. Injury 1999;30:599–604. ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite